Graphical Abstract
Abstract
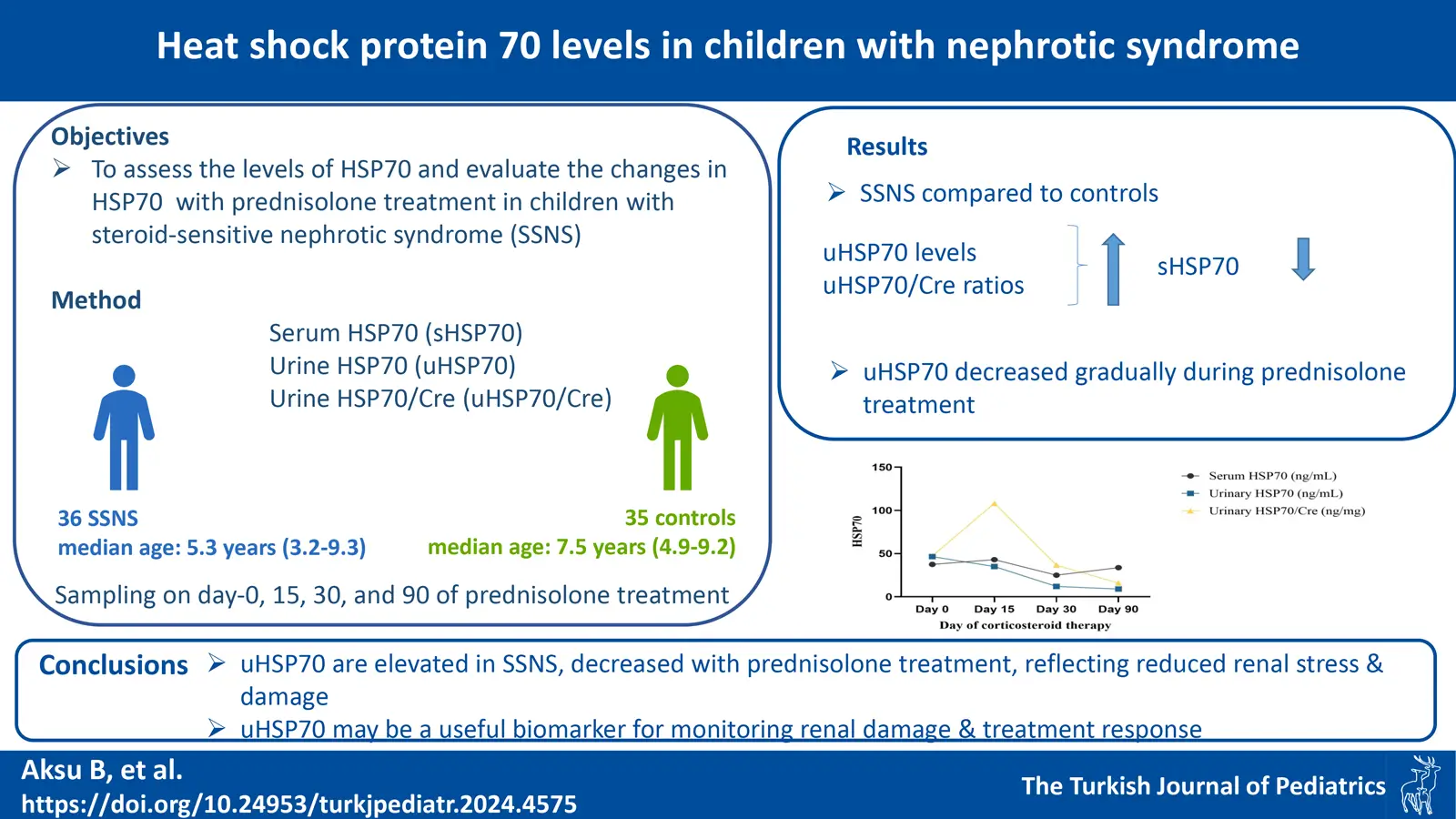
Background. Idiopathic nephrotic syndrome (NS) is the most prevalent glomerular disease in children. Heat shock protein 70 (HSP70) is synthesized in response to diverse stress factors like infections and oxidative stress. We aimed to evaluate serum and urine levels of HSP70 in children with steroid-sensitive nephrotic syndrome (SSNS) and to assess changes in HSP70 levels with prednisolone treatment. Additionally, we seek to determine whether serum and urine levels of HSP70 can differentiate between frequently relapsing and infrequently relapsing cases in children with SSNS.
Methods. A total of 36 patients with SSNS and 35 healthy children were included in the study. Samples were taken from all patients at four time points; before corticosteroid treatment (day 0) and on days 15, 30, and 90 after the initiation of corticosteroid treatment. Serum and urine levels of HSP70 were measured by enzyme-linked immunosorbent assay (ELISA).
Results. In the NS group before steroid treatment (day 0), urine HSP70 (uHSP70) levels and urine HSP70/creatinine (uHSP70/Cre) ratios were significantly higher (p<0.0001), whereas serum HSP70 (sHSP70) levels were lower (p=0.002), compared to the healthy group. uHSP70 levels decreased gradually during prednisolone treatment in the patient group (p<0.0001). There was no difference in terms of sHSP70, uHSP70, and uHSP70/Cre ratios between patients with frequently relapsing and infrequently relapsing.
Conclusions. Our study demonstrates that uHSP70 levels are elevated in SSNS prior to treatment and decrease with prednisolone therapy, reflecting reduced renal stress and damage. uHSP70 may be a useful biomarker for monitoring renal damage and treatment response. Serum and urine levels of HSP70, as well as uHSP70/Cre ratios, did not differentiate between frequent and infrequent relapses.
Keywords: pediatric, steroid-sensitive nephrotic syndrome, heat shock protein 70, HSP70, relapse, prednisolone
References
- Rheault MN. Nephrotic syndrome. In: Kher KK, Schnaper HW, Greenbaum LA, editors. Clinical Pediatric Nephrology. 3rd ed. Boca Raton: Taylor & Francis Group; 2017: 285-304.
- Somlo S, Mundel P. Getting a foothold in nephrotic syndrome. Nat Genet 2000; 24: 333-335. https://doi.org/10.1038/74139
- Barisoni L, Schnaper HW, Kopp JB. A proposed taxonomy for the podocytopathies: a reassessment of the primary nephrotic diseases. Clin J Am Soc Nephrol 2007; 2: 529-542. https://doi.org/10.2215/CJN.04121206
- Chebotareva N, Bobkova I, Shilov E. Heat shock proteins and kidney disease: perspectives of HSP therapy. Cell Stress Chaperones 2017; 22: 319-343. https://doi.org/10.1007/s12192-017-0790-0
- Beck FX, Neuhofer W, Müller E. Molecular chaperones in the kidney: distribution, putative roles, and regulation. Am J Physiol Renal Physiol 2000; 279: F203-F215. https://doi.org/10.1152/ajprenal.2000.279.2.F203
- Yilmaz A, Gedikbasi A, Yuruk Yildirim Z, et al. Higher urine heat shock protein 70/creatinine ratio in type 1 diabetes mellitus. Ren Fail 2016; 38: 404-410. https://doi.org/10.3109/0886022X.2015.1136893
- Yuruk Yildirim ZN, Usta Akgul S, Alpay H, et al. Progress Study: Progression of chronic kidney disease in children and heat shock proteins. Cell Stress Chaperones 2021; 26: 973-987. https://doi.org/10.1007/s12192-021-01239-9
- Hosseiniyan Khatibi SM, Ardalan M, Abediazar S, Zununi Vahed S. The impact of steroids on the injured podocytes in nephrotic syndrome. J Steroid Biochem Mol Biol 2020; 196: 105490. https://doi.org/10.1016/j.jsbmb.2019.105490
- van Husen M, Kemper MJ. New therapies in steroid-sensitive and steroid-resistant idiopathic nephrotic syndrome. Pediatr Nephrol 2011; 26: 881-892. https://doi.org/10.1007/s00467-010-1717-5
- Skrzypczyk P, Panczyk-Tomaszewska M, Roszkowska-Blaim M, et al. Long-term outcomes in idiopathic nephrotic syndrome: from childhood to adulthood. Clin Nephrol 2014; 81: 166-173. https://doi.org/10.5414/CN108044
- Bai M, Zhang J, Su X, et al. Serum IL-12p40: a novel biomarker for early prediction of minimal change disease relapse following glucocorticoids therapy. Front Med (Lausanne) 2022; 9: 922193. https://doi.org/10.3389/fmed.2022.922193
- Liao J, Wu XC, Cheng Q, et al. Predictability of urinary CD80 in the relapse of primary nephrotic syndrome. Biomed Res Int 2017; 2017: 9429314. https://doi.org/10.1155/2017/9429314
- Ling C, Chen Z, Fan J, et al. Decreased circulating transitional B-cell to memory B-cell ratio is a risk factor for relapse in children with steroid-sensitive nephrotic syndrome. Nephron 2021; 145: 107-112. https://doi.org/10.1159/000511319
- The primary nephrotic syndrome in children. Identification of patients with minimal change nephrotic syndrome from initial response to prednisone. A report of the International Study of Kidney Disease in Children. J Pediatr 1981; 98: 561-564. https://doi.org/10.1016/s0022-3476(81)80760-3
- Trautmann A, Boyer O, Hodson E, et al. IPNA clinical practice recommendations for the diagnosis and management of children with steroid-sensitive nephrotic syndrome. Pediatr Nephrol 2023; 38: 877-919. https://doi.org/10.1007/s00467-022-05739-3
- Chebotareva N, Bobkova I, Lysenko L, Neprinzeva N, Vinogradov A, Moiseev S. Heat shock protein 70 and anti-heat shock protein 70 antibodies in patients with chronic glomerulonephritis. Cell Stress Chaperones 2018; 23: 1229-1235. https://doi.org/10.1007/s12192-018-0928-8
- Kaysen GA. Plasma composition in the nephrotic syndrome. Am J Nephrol 1993; 13: 347-359. https://doi.org/10.1159/000168649
- Rothschild MA, Oratz M, Schreiber SS. Serum albumin. Hepatology 1988; 8: 385-401. https://doi.org/10.1002/hep.1840080234
- Yildirim ZY, Aksu B, Gedikbasi A, et al. Serum heat shock protein levels in IgA nephropathy. Iran J Pediatr 2018; 28: 1-6. https://doi.org/10.5812/ijp.63358
- Kyrieleis HAC, Löwik MM, Pronk I, et al. Long-term outcome of biopsy-proven, frequently relapsing minimal-change nephrotic syndrome in children. Clin J Am Soc Nephrol 2009; 4: 1593-1600. https://doi.org/10.2215/CJN.05691108
Copyright and license
Copyright © 2024 The Author(s). This is an open access article distributed under the Creative Commons Attribution License (CC BY), which permits unrestricted use, distribution, and reproduction in any medium or format, provided the original work is properly cited.