Graphical Abstract
Abstract
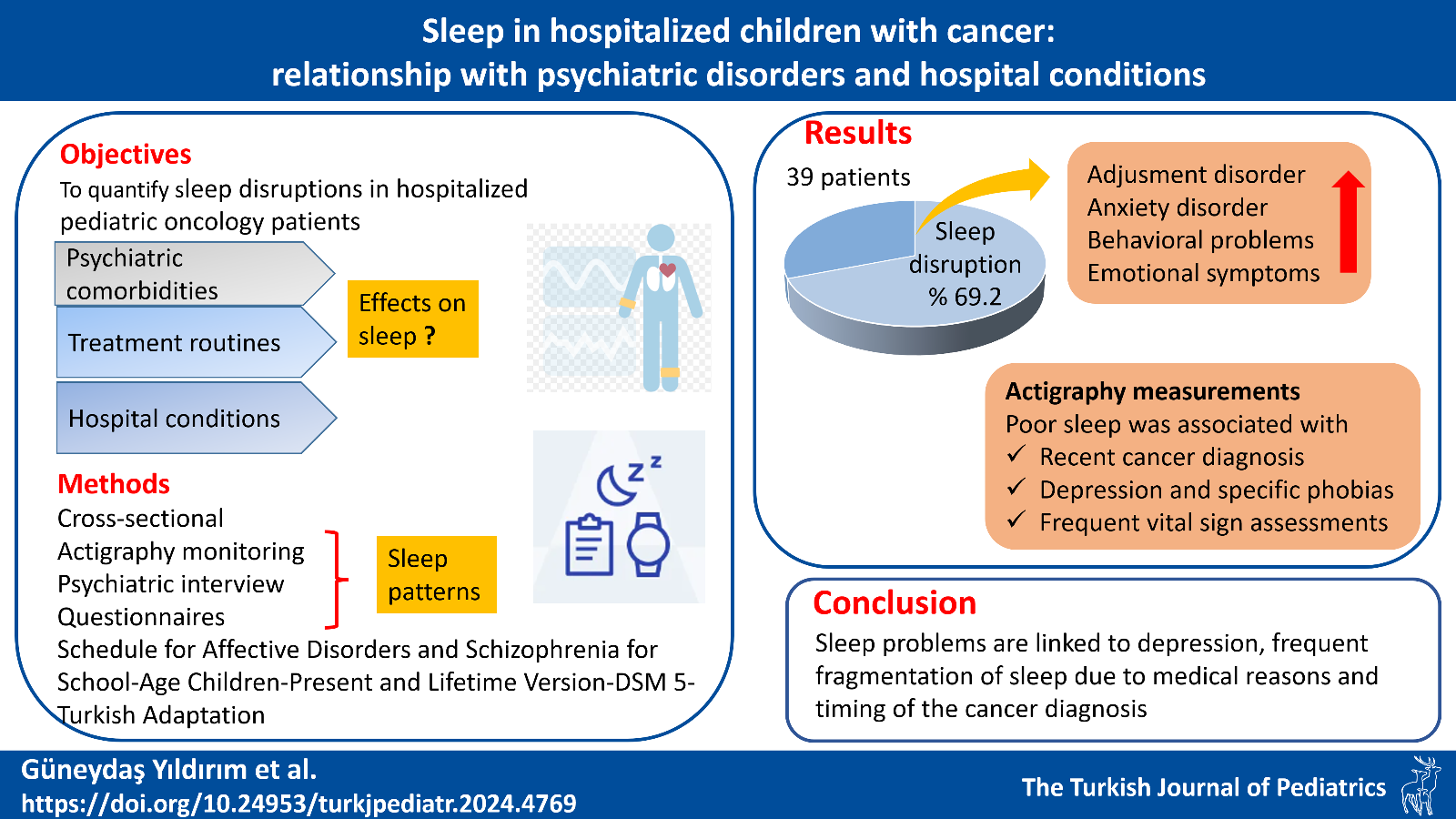
Background. Children with cancer often undergo prolonged and recurrent hospitalization, which leads to an increased incidence of sleep disruptions and psychiatric disorders. This study aimed to objectively quantify the prevalence of sleep disruptions in hospitalized pediatric oncology patients and to determine the effects of psychiatric disorders, treatment regimens, and hospital conditions on sleep patterns.
Method. This cross-sectional study included 39 children who were undergoing treatment and monitoring in the pediatric oncology inpatient service. Parents completed questionnaires providing information about their child’s sleep patterns, quality of life, and hospital conditions. The children were monitored for five days using actigraphy to record sleep parameters. They were evaluated with a semi-structured interview form (Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version-DSM 5-Turkish Adaptation) for psychiatric diagnoses.
Results. Sleep disruptions were identified in 27 (69.2%) children with cancer. In addition to adjustment disorder and anxiety disorder psychiatric diagnoses, behavioral problems and emotional symptoms were more common in the group with sleep disruptions. Actigraphy measurements indicated that poor sleep was associated with younger age, recent cancer diagnosis, specific phobias, depression, daytime napping, and frequent vital sign assessments.
Conclusion. Sleep problems in hospitalized children with cancer are linked to psychiatric comorbidities, treatment routines, and hospital conditions. By recognizing psychiatric symptoms and optimizing hospital conditions that affect sleep, healthcare providers can enhance the quality of sleep for these children.
Keywords: cancer, sleep, actigraphy, child psychiatry, Schedule for Affective Disorders and Schizophrenia for School-Age Children - Present and Lifetime Version, K-SADS-PL
References
- Ward E, DeSantis C, Robbins A, Kohler B, Jemal A. Childhood and adolescent cancer statistics, 2014. CA Cancer J Clin 2014; 64: 83-103. https://doi.org/10.3322/caac.21219
- Geçkalan Soysal D, Yazıcı N, Erbay A. Epidemiology and survival analysis of children with malignant tumors. Cukurova Medical Journal 2020; 45: 1042-1050. https://doi.org/10.17826/cumj.685250
- Linder LA, Christian BJ. Nighttime sleep characteristics of hospitalized school-age children with cancer. J Spec Pediatr Nurs 2013; 18: 13-24. https://doi.org/10.1111/jspn.12005
- Traube C, Rosenberg L, Thau F, et al. Sleep in hospitalized children with cancer: a cross-sectional study. Hosp Pediatr 2020; 10: 969-976. https://doi.org/10.1542/hpeds.2020-0101
- Stremler R, Micsinszki S, Adams S, Parshuram C, Pullenayegum E, Weiss SK. Objective sleep characteristics and factors associated with sleep duration and waking during pediatric hospitalization. JAMA Netw Open 2021; 4: e213924. https://doi.org/10.1001/jamanetworkopen.2021.3924
- Kaleyias J, Manley P, Kothare SV. Sleep disorders in children with cancer. Semin Pediatr Neurol 2012; 19: 25-34. https://doi.org/10.1016/j.spen.2012.02.013
- Rosen G, Brand SR. Sleep in children with cancer: case review of 70 children evaluated in a comprehensive pediatric sleep center. Support Care Cancer 2011; 19: 985-994. https://doi.org/10.1007/s00520-010-0921-y
- Perrin JM, Gnanasekaran S, Delahaye J. Psychological aspects of chronic health conditions. Pediatr Rev 2012; 33: 99-109. https://doi.org/10.1542/pir.33-3-99
- Varni JW, Limbers CA, Burwinkle TM. Impaired health-related quality of life in children and adolescents with chronic conditions: a comparative analysis of 10 disease clusters and 33 disease categories/severities utilizing the PedsQL 4.0 Generic Core Scales. Health Qual Life Outcomes 2007; 5: 43. https://doi.org/10.1186/1477-7525-5-43
- Çöp E, Şenses Dinç G, Çengel Kültür SE. Relationship with psychiatric symptoms: a preliminary report coping styles of mothers of children with chronic diseases and their. Turkish Journal of Pediatric Disease 2016; 10: 170-176.
- Kosir U, Wiedemann M, Wild J, Bowes L. Psychiatric disorders in adolescent cancer survivors: a systematic review of prevalence and predictors. Cancer Rep (Hoboken) 2019; 2: e1168. https://doi.org/10.1002/cnr2.1168
- Ford DE, Kamerow DB. Epidemiologic study of sleep disturbances and psychiatric disorders. An opportunity for prevention? JAMA 1989; 262: 1479-1484. https://doi.org/10.1001/jama.1989.03430110069030
- Richdale AL, Schreck KA. Sleep problems in autism spectrum disorders: Prevalence, nature, & possible biopsychosocial aetiologies. Sleep Med Rev 2009; 13: 403-411. https://doi.org/10.1016/j.smrv.2009.02.003
- van de Wouw E, Evenhuis HM, Echteld MA. Prevalence, associated factors and treatment of sleep problems in adults with intellectual disability: a systematic review. Res Dev Disabil 2012; 33: 1310-1332. https://doi.org/10.1016/j.ridd.2012.03.003
- Kaufman J, Birmaher B, Brent D, et al. Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry 1997; 36: 980-988. https://doi.org/10.1097/00004583-199707000-00021
- Ünal F, Öktem F, Çetin Çuhadaroğlu F, et al. Reliability and Validity of the Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version, DSM-5 November 2016-Turkish Adaptation (K-SADS-PL-DSM-5-T). Turk Psikiyatri Derg 2019; 3: 42-50. https://doi.org/10.5080/u23408
- Goodman R. The strengths and difficulties questionnaire: a research note. J Child Psychol Psychiatry 1997; 38: 581-586. https://doi.org/10.1111/j.1469-7610.1997.tb01545.x
- Bourdon KH, Goodman R, Rae DS, Simpson G, Koretz DS. The Strengths and Difficulties Questionnaire: U.S. normative data and psychometric properties. J Am Acad Child Adolesc Psychiatry 2005; 44: 557-564. https://doi.org/10.1097/01.chi.0000159157.57075.c8
- Güvenir T, Özbek A, Baykara B, Arkar H, Şentürk B, İncekaş S. Psychometric properties of the Turkish version of the Strengths and Difficulties Questionnaire (SDQ). Turkish Journal of Child and Adolescent Mental Health 2008; 15: 65-74.
- Varni JW, Seid M, Rode CA. The PedsQL: measurement model for the pediatric quality of life inventory. Med Care 1999; 37: 126-139. https://doi.org/10.1097/00005650-199902000-00003
- Uneri OS, Agaoglu B, Coskun A, Memik NC. Validity and reliability of Pediatric Quality of Life Inventory for 2- to 4-year-old and 5- to 7-year-old Turkish children. Qual Life Res 2008; 17: 307-315. https://doi.org/10.1007/s11136-007-9303-4
- Memik NÇ, Ağaoğlu B, Coşkun A, Üneri ÖŞ, Karakaya I. The validity and reliability of the Turkish Pediatric Quality of Life Inventory for Children 13-18 years old. Turk Psikiyatri Derg 2007; 18: 353-363.
- Uğraş S, Koşe Demiray Ç, Mutluer T, Coşkun M. The reliability and validity of Turkish version of Preschool Anxiety Scale. Turkish Journal of Child and Adolescent Mental Health 2018; 25: 63-76.
- Edrissi F, Havighurst SS, Aghebati A, Habibi M, Arani AM. A pilot study of the tuning in to kids parenting program in Iran for reducing preschool children’s anxiety. Journal of Child and Family Studies 2019; 28: 1695-1702. https://doi.org/10.1007/s10826-019-01400-0
- Chorpita BF, Ebesutani C, Spence SH. Revised Children’s Anxiety and Depression Scale: User’s Guide. Jan 25, 2022. Available at: https://www.childfirst.ucla.edu/wp-content/uploads/sites/163/2022/01/RCADSUsersGuide20220125.pdf
- Gormez V, Kılınçaslan A, Orengul AC, et al. Psychometric properties of the Turkish version of the Revised Child Anxiety and Depression Scale – Child Version in a clinical sample. Psychiatry and Clinical Psychopharmacology 2017; 27: 84-92. https://doi.org/10.1080/24750573.2017.1297494
- Meltzer LJ, Davis KF, Mindell JA. Patient and parent sleep in a children’s hospital. Pediatr Nurs 2012; 38: 64-72.
- Owens JA, Spirito A, McGuinn M. The Children’s Sleep Habits Questionnaire (CSHQ): psychometric properties of a survey instrument for school-aged children. Sleep 2000; 23: 1043-1051.
- Perdahlı Fiş N, Arman A, Ay P, et al. The validity and the reliability of Turkish version of Children’s Sleep Habits Questionnaire. Alpha Psychiatry 2010; 11: 151-160.
- Goodlin-Jones BL, Sitnick SL, Tang K, Liu J, Anders TF. The Children’s Sleep Habits Questionnaire in toddlers and preschool children. J Dev Behav Pediatr 2008; 29: 82-88. https://doi.org/10.1097/dbp.0b013e318163c39a
- Shui AM, Richdale AL, Katz T. Evaluating sleep quality using the CSHQ-Autism. Sleep Med 2021; 87: 69-76. https://doi.org/10.1016/j.sleep.2021.08.022
- Ekinci O, Isik U, Gunes S, Ekinci N. Understanding sleep problems in children with epilepsy: associations with quality of life, attention-deficit hyperactivity disorder and maternal emotional symptoms. Seizure 2016; 40: 108-113. https://doi.org/10.1016/j.seizure.2016.06.011
- Teicher MH. Actigraphy and motion analysis: new tools for psychiatry. Harv Rev Psychiatry 1995; 3: 18-35. https://doi.org/10.3109/10673229509017161
- McLaughlin Crabtree V, Williams NA. Normal sleep in children and adolescents. Child Adolesc Psychiatr Clin N Am 2009; 18: 799-811. https://doi.org/10.1016/j.chc.2009.04.013
- van Litsenburg RRL, Waumans RC, van den Berg G, Gemke RJBJ. Sleep habits and sleep disturbances in Dutch children: a population-based study. Eur J Pediatr 2010; 169: 1009-1015. https://doi.org/10.1007/s00431-010-1169-8
- Le Guen Y, Gagnadoux F, Hureaux J, et al. Sleep disturbances and impaired daytime functioning in outpatients with newly diagnosed lung cancer. Lung Cancer 2007; 58: 139-143. https://doi.org/10.1016/j.lungcan.2007.05.021
- Chang WP, Lin CC. Relationships of salivary cortisol and melatonin rhythms to sleep quality, emotion, and fatigue levels in patients with newly diagnosed lung cancer. Eur J Oncol Nurs 2017; 29: 79-84. https://doi.org/10.1016/j.ejon.2017.05.008
- Üstün G, Akan B, Küçük L. Examining the relationship between psychosocial symptoms in hospitalized children and the anxiety levels of their mothers. E-Journal of Dokuz Eylul University Nursing Faculty 2021; 14: 207-216. https://doi.org/10.46483/deuhfed.832698
- Crisp J, Ungerer JA, Goodnow JJ. The impact of experience on children’s understanding of illness. J Pediatr Psychol 1996; 21: 57-72. https://doi.org/10.1093/jpepsy/21.1.57
- Barlow JH, Ellard DR. The psychosocial well-being of children with chronic disease, their parents and siblings: an overview of the research evidence base. Child Care Health Dev 2006; 32: 19-31. https://doi.org/10.1111/j.1365-2214.2006.00591.x
- Rait DS, Jacobsen PB, Lederberg MS, Holland JC. Characteristics of psychiatric consultations in a pediatric cancer center. Am J Psychiatry 1988; 145: 363-364. https://doi.org/10.1176/ajp.145.3.363
- Kouros CD, El-Sheikh M. Daily mood and sleep: reciprocal relations and links with adjustment problems. J Sleep Res 2015; 24: 24-31. https://doi.org/10.1111/jsr.12226
- Roy-Byrne PP, Davidson KW, Kessler RC, et al. Anxiety disorders and comorbid medical illness. Gen Hosp Psychiatry 2008; 30: 208-225. https://doi.org/10.1016/j.genhosppsych.2007.12.006
- Akyay A, Olcay L. Early and late side effects of acute lymphoblastic leukemia therapy in children. Turkish Journal of Pediatric Disease 2014; 1: 46-54.
- Wilkinson SR. Germs. Nursery school children’s views on the causality of illness. Clin Pediatr (Phila) 1987; 26: 465-469. https://doi.org/10.1177/000992288702600906
- Riemann D, Schnitzler M, Hohagen F, Berger M. Depression and sleep-the status of current research. Fortschr Neurol Psychiatr 1994; 62: 458-478. https://doi.org/10.1055/s-2007-1002303
- Ersöz Alan B, Akdemir D. Psikiyatrik Hastalıklar ve Uyku Bozuklukları. In: Özçelik U, Aslan AT, Erdem Eralp E, editors. Çocuklarda Uyku Bozuklukları. İstanbul: Logos Yayıncılık; 2022: 574-588.
- Nelson CJ, Cho C, Berk AR, Holland J, Roth AJ. Are gold standard depression measures appropriate for use in geriatric cancer patients? A systematic evaluation of self-report depression instruments used with geriatric, cancer, and geriatric cancer samples. J Clin Oncol 2010; 28: 348-356. https://doi.org/10.1200/JCO.2009.23.0201
- Nutt D, Wilson S, Paterson L. Sleep disorders as core symptoms of depression. Dialogues Clin Neurosci 2008; 10: 329-336. https://doi.org/10.31887/DCNS.2008.10.3/dnutt
- Smedje H, Broman JE, Hetta J. Associations between disturbed sleep and behavioural difficulties in 635 children aged six to eight years: a study based on parents’ perceptions. Eur Child Adolesc Psychiatry 2001; 10: 1-9. https://doi.org/10.1007/s007870170041
- Liu G, Fang L, Pan Y, Zhang D. Media multitasking and adolescents’ sleep quality: the role of emotional-behavioral problems and psychological suzhi. Children and Youth Services Review 2019; 100: 415-421. https://doi.org/10.1016/j.childyouth.2019.03.026
- Erickson JM, Beck SL, Christian BR, et al. Fatigue, sleep-wake disturbances, and quality of life in adolescents receiving chemotherapy. J Pediatr Hematol Oncol 2011; 33: e17-e25. https://doi.org/10.1097/MPH.0b013e3181f46a46
- Sheikh IN, Roth M, Stavinoha PL. Prevalence of sleep disturbances in pediatric cancer patients and their diagnosis and management. Children (Basel) 2021; 8: 1100. https://doi.org/10.3390/children8121100
Copyright and license
Copyright © 2024 The Author(s). This is an open access article distributed under the Creative Commons Attribution License (CC BY), which permits unrestricted use, distribution, and reproduction in any medium or format, provided the original work is properly cited.