Graphical Abstract
Abstract
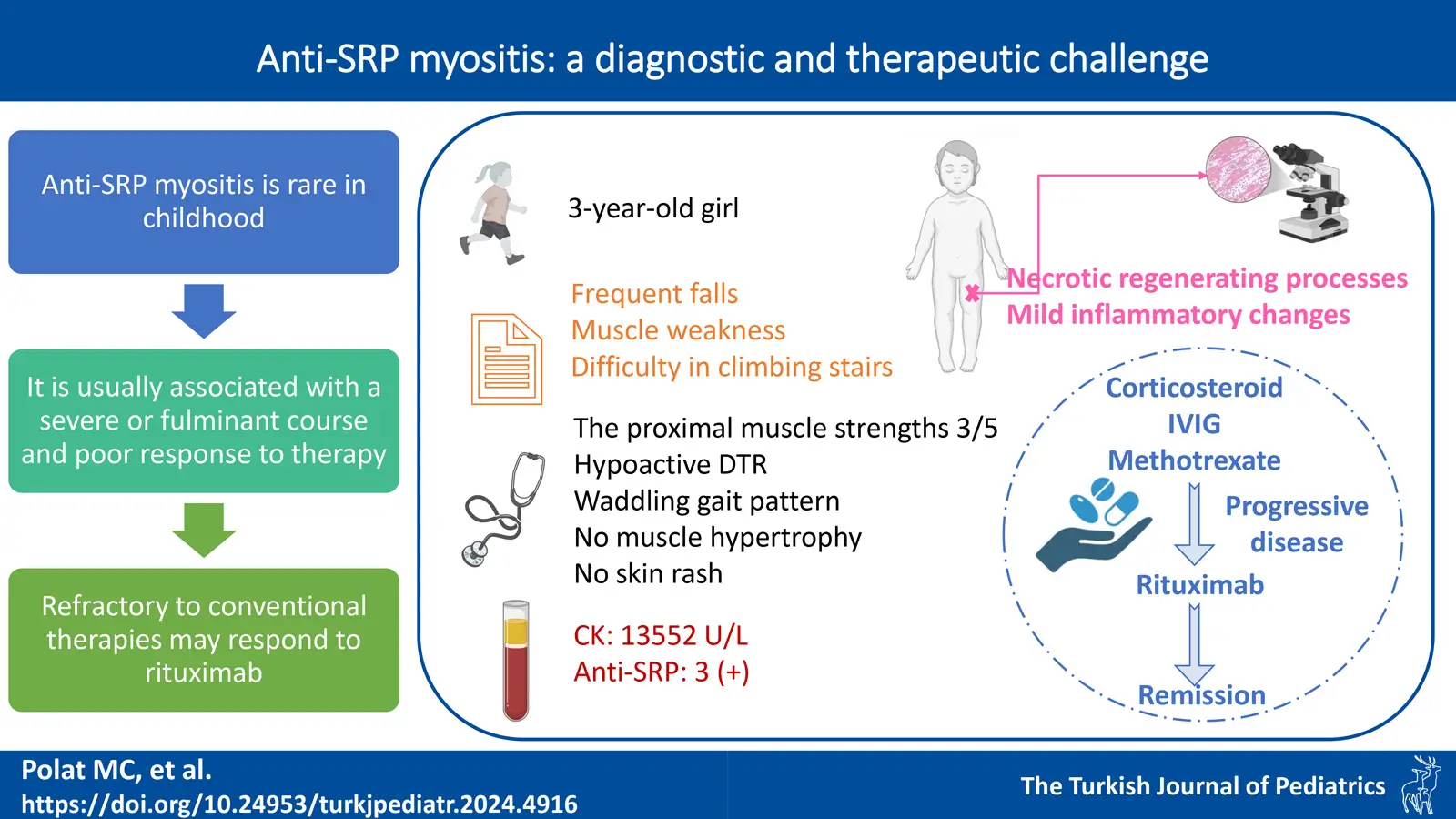
Background. Anti-signal recognition protein (anti-SRP) myopathy is a rare idiopathic inflammatory myopathy in children. Herein, a 3-year-old patient with severe anti-SRP myopathy showing a rapidly progressive disease course is presented in order to increase the awareness of pediatricians about idiopathic inflammatory myopathies.
Case Presentation. A previously healthy 3-year-old girl presented with progressive symmetrical proximal muscle weakness that caused difficulty in climbing stairs for two months prior to evaluation, and a marked elevation of the serum creatine kinase levels. A skeletal muscle biopsy revealed necrotic and regenerating processes, with mild inflammatory changes. Myositis-specific and associated autoantibodies tested by the immunoblot method were positive for anti-SRP. Pulse corticosteroid, intravenous immunoglobulin, and methotrexate were administered. However, muscle weakness progressed, respiratory distress and dysphagia developed. Rituximab was initiated. While on rituximab treatment, she was able to walk independently and muscle enzymes were within normal range at the 15th month of diagnosis.
Conclusion. Early diagnosis of patients with anti-SRP myositis is important to control inflammation and prevent disease progression and complications. To our knowledge, our patient is the youngest case reported in the literature and was successfully treated with rituximab added to conventional therapy.
Keywords: anti-signal recognition protein myopathy, anti-SRP, rituximab, inflammatory myopathy, children
References
- Papadopoulou C, Chew C, Wilkinson MGL, McCann L, Wedderburn LR. Juvenile idiopathic inflammatory myositis: an update on pathophysiology and clinical care. Nat Rev Rheumatol 2023; 19: 343-362. https://doi.org/10.1038/s41584-023-00967-9
- Suzuki S, Nishikawa A, Kuwana M, et al. Inflammatory myopathy with anti-signal recognition particle antibodies: case series of 100 patients. Orphanet J Rare Dis 2015; 10: 61. https://doi.org/10.1186/s13023-015-0277-y
- Binns EL, Moraitis E, Maillard S, et al. Effective induction therapy for anti-SRP associated myositis in childhood: a small case series and review of the literature. Pediatr Rheumatol Online J 2017; 15: 77. https://doi.org/10.1186/s12969-017-0205-x
- Watanabe Y, Uruha A, Suzuki S, et al. Clinical features and prognosis in anti-SRP and anti-HMGCR necrotising myopathy. J Neurol Neurosurg Psychiatry 2016; 87: 1038-1044. https://doi.org/10.1136/jnnp-2016-313166
- Luca NJC, Atkinson A, Hawkins C, Feldman BM. Anti-signal recognition particle-positive juvenile polymyositis successfully treated with rituximab. J Rheumatol 2012; 39: 1483-1485. https://doi.org/10.3899/jrheum.111592
- Suzuki S, Ohta M, Shimizu Y, Hayashi YK, Nishino I. Anti-signal recognition particle myopathy in the first decade of life. Pediatr Neurol 2011; 45: 114-116. https://doi.org/10.1016/j.pediatrneurol.2011.04.009
- Rouster-Stevens KA, Pachman LM. Autoantibody to signal recognition particle in African American girls with juvenile polymyositis. J Rheumatol 2008; 35: 927-929.
- Kawabata T, Komaki H, Saito T, et al. A pediatric patient with myopathy associated with antibodies to a signal recognition particle. Brain Dev 2012; 34: 877-880. https://doi.org/10.1016/j.braindev.2012.02.009
- Huber AM. Juvenile idiopathic inflammatory myopathies. Pediatr Clin North Am 2018; 65: 739-756. https://doi.org/10.1016/j.pcl.2018.04.006
- Capoferri G, Milani GP, Ramelli GP, Ferrarini A, Bianchetti MG, Lava SAG. Sporadic acute benign calf myositis: systematic literature review. Neuromuscul Disord 2018; 28: 443-449. https://doi.org/10.1016/j.nmd.2018.02.005
- Mercuri E, Bönnemann CG, Muntoni F. Muscular dystrophies. Lancet 2019; 394: 2025-2038. https://doi.org/10.1016/S0140-6736(19)32910-1
- Suzuki S, Satoh T, Sato S, et al. Clinical utility of anti-signal recognition particle antibody in the differential diagnosis of myopathies. Rheumatology (Oxford) 2008; 47: 1539-1542. https://doi.org/10.1093/rheumatology/ken325
- Allenbach Y, Benveniste O. Acquired necrotizing myopathies. Curr Opin Neurol 2013; 26: 554-560. https://doi.org/10.1097/WCO.0b013e328364e9d9
- Xiong A, Yang G, Song Z, et al. Rituximab in the treatment of immune-mediated necrotizing myopathy: a review of case reports and case series. Ther Adv Neurol Disord 2021; 14: 1756286421998918. https://doi.org/10.1177/1756286421998918
- Kishi T, Rider LG, Pak K, et al. Association of anti-3-hydroxy-3-methylglutaryl-coenzyme a reductase autoantibodies with DRB1*07:01 and severe myositis in juvenile myositis patients. Arthritis Care Res (Hoboken) 2017; 69: 1088-1094. https://doi.org/10.1002/acr.23113
- Della Marina A, Pawlitzki M, Ruck T, et al. Clinical course, myopathology and challenge of therapeutic intervention in pediatric patients with autoimmune-mediated necrotizing myopathy. Children (Basel) 2021; 8: 721. https://doi.org/10.3390/children8090721
- Momomura M, Miyamae T, Nozawa T, et al. Serum levels of anti-SRP54 antibodies reflect disease activity of necrotizing myopathy in a child treated effectively with combinatorial methylprednisolone pulses and plasma exchanges followed by intravenous cyclophosphamide. Mod Rheumatol 2014; 24: 529-531. https://doi.org/10.3109/14397595.2013.852852
- Zhao Y, Liu X, Zhang W, Yuan Y. Childhood autoimmune necrotizing myopathy with anti-signal recognition particle antibodies. Muscle Nerve 2017; 56: 1181-1187. https://doi.org/10.1002/mus.25575
- Kobayashi I, Tozawa Y, Ueki M, et al. Tacrolimus in combination with methotrexate and corticosteroid for the treatment of child-onset anti-signal recognition particle antibody-positive necrotizing myopathy. Scand J Rheumatol 2017; 46: 409-410. https://doi.org/10.1080/03009742.2016.1241297
- Rider LG, Miller FW, Targoff IN, et al. A broadened spectrum of juvenile myositis. Myositis-specific autoantibodies in children. Arthritis Rheum 1994; 37: 1534-1538. https://doi.org/10.1002/art.1780371019
- Rider LG, Shah M, Mamyrova G, et al. The myositis autoantibody phenotypes of the juvenile idiopathic inflammatory myopathies. Medicine (Baltimore) 2013; 92: 223-243. https://doi.org/10.1097/MD.0b013e31829d08f9
Copyright and license
Copyright © 2024 The Author(s). This is an open access article distributed under the Creative Commons Attribution License (CC BY), which permits unrestricted use, distribution, and reproduction in any medium or format, provided the original work is properly cited.