Graphical Abstract
Abstract
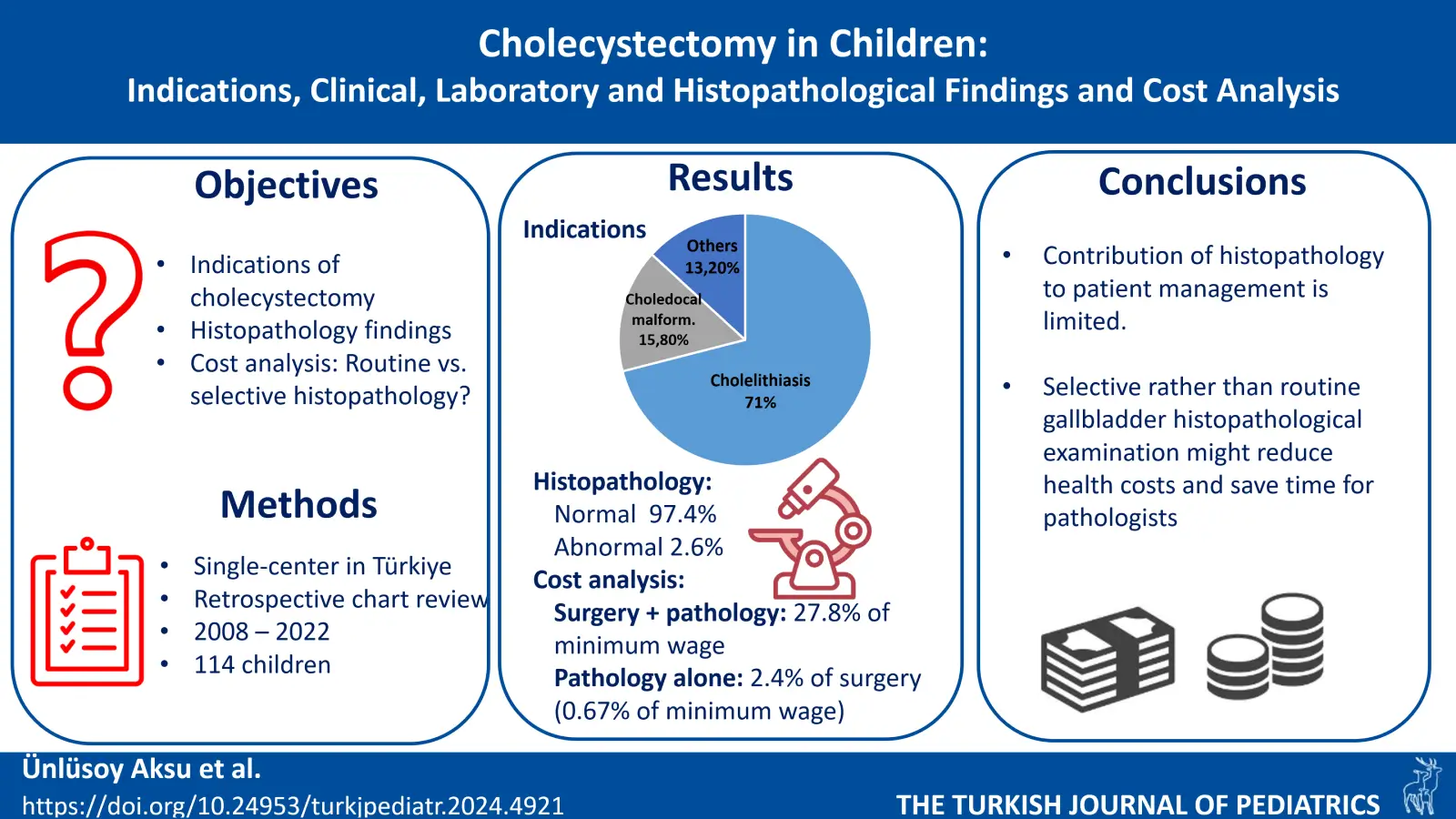
Background. The most common indication for cholecystectomy in children is cholelithiasis, and routine histopathological examination is performed on all gallbladder specimens. Currently, selective histopathological examination is suggested instead of routine examination due to the low frequency of gallbladder cancer in adults. The purpose of this study was to evaluate the indications, clinical, laboratory and histopathological findings of the cholecystectomy in children. We also questioned the contribution and cost-effectiveness of routine histopathological evaluation in diagnosis and treatment.
Methods. A total of 114 children underwent cholecystectomy between the years 2008 and 2022. The clinical findings, laboratory, and imaging results of the patients and histopathological findings of the gallbladder specimens were evaluated retrospectively.
Results. Cholelithiasis were diagnosed in 71%, choledochal malformation in 15.8%, hydrops of gallbladder and/or biliary sludge in 12.3%, and hypoplasia of gallbladder in 0.9% of the patients. Histopathologically significant findings were observed in only 3 patients (2.6%); adenomyomatosis in 2 and angiodysplasia and pyloric metaplasia in 1. While the cost of a cholecystectomy and histopathologic examination combined amounted to 27.77% of the minimum wage in Türkiye in 2024, the histopathologic examination alone constitutes just 0.67% of the minimum wage and 2.4% of the operation fee.
Conclusion. In children undergoing cholecystectomy, histopathological examination does not provide any significant contribution to the patient’s diagnosis and follow-up management. In children, selective gallbladder histopathological examination might reduce health costs and save time for pathologists.
Keywords: cholecystectomy, histopathology, cholelithiasis, adenomyomatosis, children
References
- Mehta S, Lopez ME, Chumpitazi BP, Mazziotti MV, Brandt ML, Fishman DS. Clinical characteristics and risk factors for symptomatic pediatric gallbladder disease. Pediatrics 2012; 129: e82-e88. https://doi.org/10.1542/peds.2011-0579
- Zdanowicz K, Daniluk J, Lebensztejn DM, Daniluk U. The etiology of cholelithiasis in children and adolescents-a literature review. Int J Mol Sci 2022; 23: 13376. https://doi.org/10.3390/ijms232113376
- Walker SK, Maki AC, Cannon RM, et al. Etiology and incidence of pediatric gallbladder disease. Surgery 2013; 154: 927-933. https://doi.org/10.1016/j.surg.2013.04.040
- Pelizzo G, Bussani R, De Silvestri A, et al. Laparoscopic cholecystectomy for symptomatic cholecystic disease in children: defining surgical timing. Front Pediatr 2020; 8: 203. https://doi.org/10.3389/fped.2020.00203
- Limaiem F, Sassi A, Talbi G, Bouraoui S, Mzabi S. Routine histopathological study of cholecystectomy specimens. Useful? A retrospective study of 1960 cases. Acta Gastroenterol Belg 2017; 80: 365-370.
- Hundal R, Shaffer EA. Gallbladder cancer: epidemiology and outcome. Clin Epidemiol 2014; 6: 99-109. https://doi.org/10.2147/CLEP.S37357
- Kokoroskos N, Peponis T, Lee JM, et al. Gallbladder wall thickness as a predictor of intraoperative events during laparoscopic cholecystectomy: a prospective study of 1089 patients. Am J Surg 2020; 220: 1031-1037. https://doi.org/10.1016/j.amjsurg.2020.03.007
- Li ZZ, Guan LJ, Ouyang R, Chen ZX, Ouyang GQ, Jiang HX. Global, regional, and national burden of gallbladder and biliary diseases from 1990 to 2019. World J Gastrointest Surg 2023; 15: 2564-2578. https://doi.org/10.4240/wjgs.v15.i11.2564
- Peery AF, Crockett SD, Murphy CC, et al. Burden and cost of gastrointestinal, liver, and pancreatic diseases in the United States: update 2021. Gastroenterology 2022; 162: 621-644. https://doi.org/10.1053/j.gastro.2021.10.017
- Destro F, Pierucci UM, Durante E, et al. Laparoscopic cholecystectomy in children: the experience of two centers focusing on indications and timing in the era of "New Technologies". Children (Basel) 2023; 10: 1771. https://doi.org/10.3390/children10111771
- Mattson A, Sinha A, Njere I, Borkar N, Sinha CK. Laparoscopic cholecystectomy in children: a systematic review and meta-analysis. Surgeon 2023; 21: e133-e141. https://doi.org/10.1016/j.surge.2022.09.003
- Lam R, Zakko A, Petrov JC, Kumar P, Duffy AJ, Muniraj T. Gallbladder disorders: a comprehensive review. Dis Mon 2021; 67: 101130. https://doi.org/10.1016/j.disamonth.2021.101130
- Bazoua G, Hamza N, Lazim T. Do we need histology for a normal-looking gallbladder? J Hepatobiliary Pancreat Surg 2007; 14: 564-568. https://doi.org/10.1007/s00534-007-1225-6
- Parolini F, Indolfi G, Magne MG, et al. Adenomyomatosis of the gallbladder in childhood: a systematic review of the literature and an additional case report. World J Clin Pediatr 2016; 5: 223-227. https://doi.org/10.5409/wjcp.v5.i2.223
- Terada T. Histopathologic features and frequency of gall bladder lesions in consecutive 540 cholecystectomies. Int J Clin Exp Pathol 2013; 6: 91-96.
- Pasierbek M, Korlacki W, Grabowski A. Adenomyomatosis of the gallbladder in an adolescent, a very rare condition. Arch Argent Pediatr 2020; 118: e43-e47. https://doi.org/10.5546/aap.2020.eng.e43
- Ghartimagar D, Shrestha MK, Jhunjhunwala A, et al. Non-neoplastic lesions of gallbladder among cholecystectomy specimens of a tertiary care center: a descriptive cross-sectional study. JNMA J Nepal Med Assoc 2021; 59: 970-974. https://doi.org/10.31729/jnma.5861
- Švagelj I, Vučko M, Hrskanović M, Švagelj D. Angiodysplasia of the gallbladder: an unknown risk factor for cholecystolithiasis. Case Rep Pathol 2020; 2020: 7192634. https://doi.org/10.1155/2020/7192634
- Garzón G LN, Jaramillo B LE, Valero H JJ, Quintero C EM. Eosinophilic cholecystitis in children: case series. J Pediatr Surg 2021; 56: 550-552. https://doi.org/10.1016/j.jpedsurg.2020.05.039
- Argon A, Yağcı A, Taşlı F, et al. A different perspective on macroscopic sampling of cholecystectomy specimens. Korean J Pathol 2013; 47: 519-525. https://doi.org/10.4132/KoreanJPathol.2013.47.6.519
- Abdullazade S, Akarca FG, Esendagli G, et al. The contribution of additional sampling in cholecystectomy materials: a multicenter prospective study. Turk Patoloji Derg 2020; 36: 188-194. https://doi.org/10.5146/tjpath.2020.01483
- Deng YL, Xiong XZ, Zhou Y, Shrestha A, Li FY, Cheng NS. Selective histology of cholecystectomy specimens-is it justified? J Surg Res 2015; 193: 196-201. https://doi.org/10.1016/j.jss.2014.07.039
- Olthof PB, Metman MJH, de Krijger RR, Scheepers JJ, Roos D, Dekker JWT. Routine pathology and postoperative follow-up are not cost-effective in cholecystectomy for benign gallbladder disease. World J Surg 2018; 42: 3165-3170. https://doi.org/10.1007/s00268-018-4619-5
- Bastiaenen VP, Tuijp JE, van Dieren S, et al. Safe, selective histopathological examination of gallbladder specimens: a systematic review. Br J Surg 2020; 107: 1414-1428. https://doi.org/10.1002/bjs.11759
- Bastiaenen VP, van Vliet JLP, de Savornin Lohman EAJ, et al. Safety and economic analysis of selective histopathology following cholecystectomy: multicentre, prospective, cross-sectional FANCY study. Br J Surg 2022; 109: 355-362. https://doi.org/10.1093/bjs/znab469
Copyright and license
Copyright © 2024 The Author(s). This is an open access article distributed under the Creative Commons Attribution License (CC BY), which permits unrestricted use, distribution, and reproduction in any medium or format, provided the original work is properly cited.