Graphical Abstract
Abstract
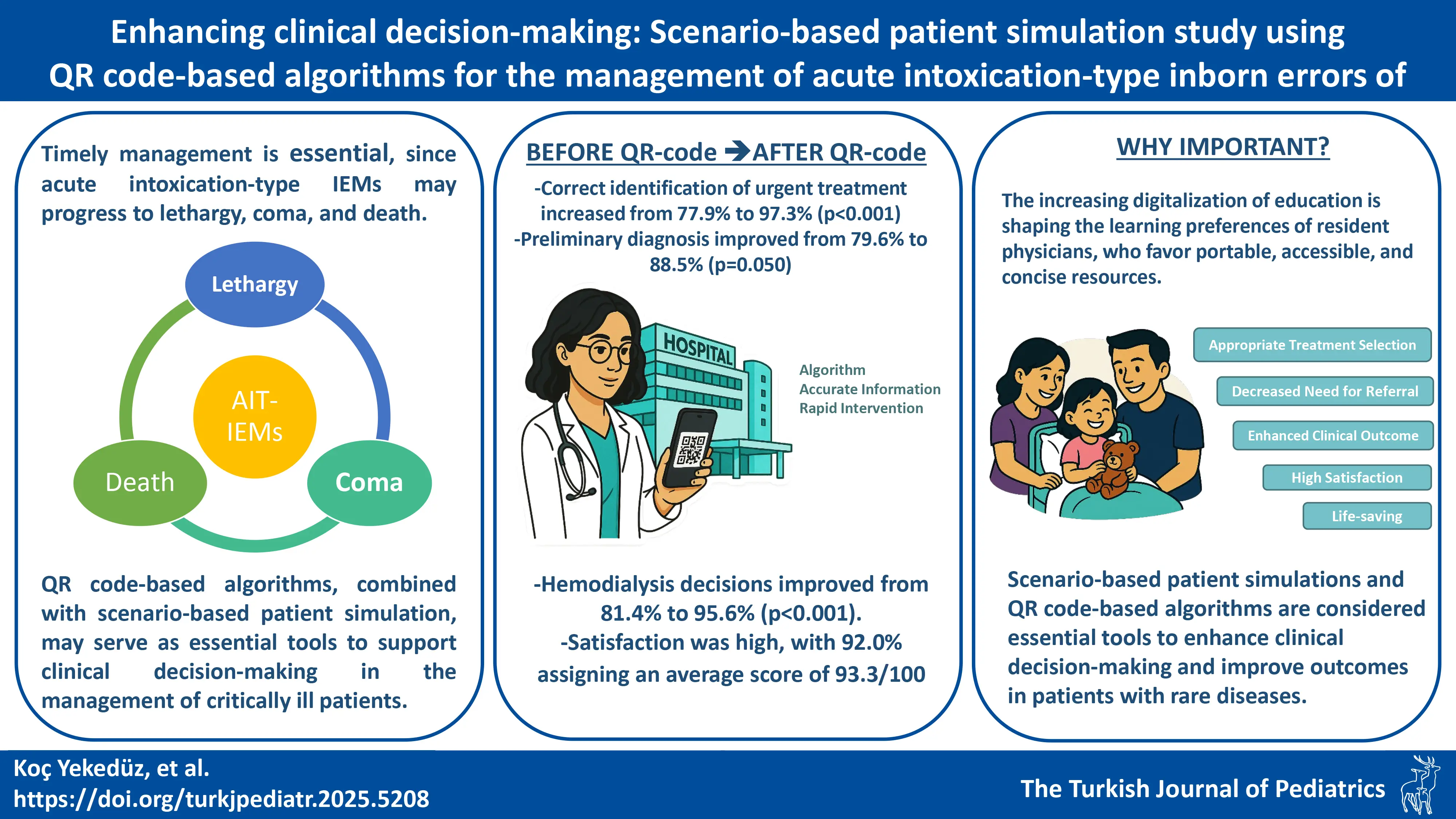
Background. Acute intoxication-type inborn errors of metabolism (IEMs) present significant challenges in pediatric care. Prompt recognition and appropriate management are essential to prevent serious complications and reduce mortality. Recent studies increasingly highlight the use of quick response (QR) code-based tools to facilitate rapid intervention, particularly in emergency departments and primary healthcare settings. In this study, the effectiveness of a newly developed QR code-based algorithm, designed to support the accurate recognition and effective management of acute intoxication-type IEMs and, indirectly, to reduce sequelae and mortality, was evaluated for the first time.
Methods. This study included 113 pediatric residents from two centers, one with (Group 1, n=77) and one without (Group 2, n=36) a mandatory pediatric metabolism rotation. All participants completed a scenario-based simulation with 10 clinical questions on a standardized patient case of acute intoxication-type inborn errors of metabolism, both before and after using the QR code-based algorithm. The algorithm, developed in accordance with international guidelines, was accessed via mobile devices. Pre- and post-intervention responses were compared using appropriate statistical tests. The effectiveness of the QR code in guiding the management of a simulated patient was analyzed.
Results. Of the participants, 73 (64.6%) were female and 40 (35.4%) male; the median age was 28.0 years. Forty-two residents (37.2%) had previous experience in a pediatric metabolism unit. Correct identification of urgent treatment increased from 77.9% to 97.3% (p<0.001). Preliminary diagnosis improved from 79.6% to 88.5% (p=0.050). Only 0.9% initially selected the correct treatment sequence versus 81.4% post-intervention (p<0.001). Hemodialysis decisions improved from 81.4% to 95.6% (p<0.001). Satisfaction was high, with 92.0% assigning an average score of 93.3/100.
Conclusion. Considering the limited knowledge of rare diseases among physicians, scenario-based simulation training and the widespread use of QR code-accessed algorithms in emergency departments appear essential to improve outcomes in patients at risk of severe complications.
Keywords: acute intoxication-type inborn errors of metabolism, QR code algorithms, scenario-based training
Introduction
Healthcare services are continuously evolving in line with technological advances, and digitalization is at the forefront of this transformation. Quick Response (QR) codes have become a vital tool facilitating the storage, sharing, and accessing of information, supporting numerous applications in the healthcare sector.1-3
QR codes have a broad range of applications in the provision of healthcare education and services, and have been employed in numerous areas to date, such as medical school student training4, resident physician training in emergency departments5, the provision of evidence-based care to newborns and mothers in emergency departments6, the expediting of consent processes in emergency departments7, the management of emergencies such as anaphylaxis8,9, in family medicine residency clinics1, facilitating pharmacy service operations10, COVID-19 pandemic management11 and health profile card creation, while also providing access to healthcare and educational services for those with disabilities.8,12 The advantages of QR code systems in these areas have been reported, along with their efficacy in enhancing various healthcare processes.
Inborn errors of metabolism (IEMs), although individually rare, collectively represent a significant group of disorders. Awareness-raising activities to highlight inborn errors of metabolism are organized worldwide, and physicians receive both pre-graduate and post-graduate training to ensure the proper management of patients.13 In acute intoxication type IEMs, such as organic acidaemia, maple syrup urine disease, urea cycle disorders, and fatty acid oxidation defects, sequelae or death may occur if acute attacks are not managed correctly.14,15 The rapid initiation of disease-specific treatment, which these patients require, can be lifesaving.16 Therefore, the widespread adoption of technologies such as QR codes, which have the potential to facilitate patient management and expedite treatments in emergency departments, may play an important role.
The current literature includes only a limited number of studies examining the use of QR code-based algorithms for the management of patients with IEM, A study in the United Kingdom has put forward recommendations for both patients and healthcare professionals related to the management of metabolic emergencies such as hyperammonaemia. These are based on Royal College of Paediatrics and Child Health17 and British Inherited Metabolic Disease Group18,19 guidelines, in which the emphasis is on acting swiftly to save lives.
This study evaluates the effectiveness of a QR code-based algorithm developed in Pediatric Metabolism Department, designed to aid in the accurate recognition, management, and reduction of sequelae and mortality risks associated with acute intoxication-type IEMs—such as urea cycle disorders, organic acidaemias, maple syrup urine disease, and fatty acid oxidation defects—across all levels of care, from primary to tertiary. To achieve this, pediatric residents from two centers, one with and one without a pediatric metabolism department, were included. Responses to patient scenario questions were analyzed both before and after their exposure to the QR code algorithm, considering whether they had completed a rotation in a pediatric metabolism department. This approach allowed us to assess both the general applicability of the algorithm and its utility in different training environments.
Materials and Methods
Included in the study were pediatric residents who were assigned to two groups, with Group 1 comprised of residents from the Ankara University Faculty of Medicine Department of Pediatrics, in which a metabolism rotation is included as part of pediatric training, and Group 2 comprising residents from the Gazi Yaşargil Training and Research Hospital Department of Pediatrics, in which the training does not include a metabolism rotation. Pediatric residents in Group 1 are required to undergo mandatory foundational pediatric metabolism training, as stipulated by university regulations, and this training is assessed through an annual examination. The basic characteristics of the respondent residents, including age, gender and details of their pediatric training, were also recorded.
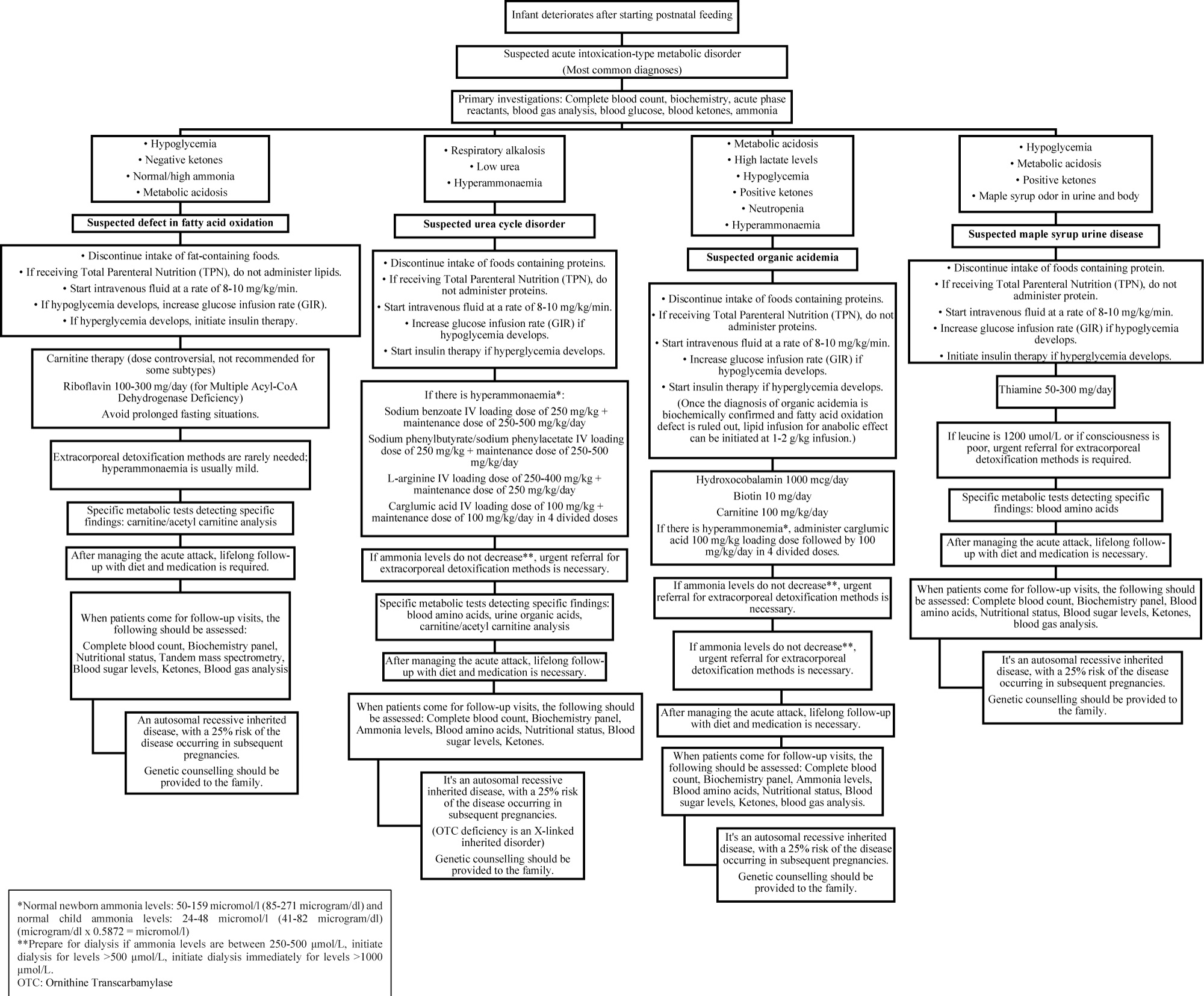
A total of 113 residents participated in the study, including 77 residents from the Ankara University Faculty of Medicine Department of Pediatrics (Group 1) and 36 residents from the Gazi Yaşargil Training and Research Hospital Department of Pediatrics (Group 2). All residents participated in a Scenario-Based Patient Simulation in which they were presented with 10 questions (Supplementary Materials) related to acute intoxication-type IEM. The baseline information for this scenario included the neonatal history, consanguinity status, sibling history, presenting complaints, clinical progression, and physical examination findings of each case. Prior to applying the QR code-based algorithm, all residents answered the same 10 questions related to each case based on their prior knowledge, and subsequently answered the same 10 questions after accessing the QR code-based algorithm (Fig. 1). Of the 10 questions, eight were multiple choice questions, while two were open-ended. The responses to the open-ended questions were categorised as correct, incorrect, incomplete, or unanswered. Pediatric residents utilized the hospital internet or their personal mobile internet for access to the QR code. During the time each participant answered the scenario questions, one of authors was present alongside them at both centers, and the questions were presented to the participants one at a time. This ensured that returning to and modifying previous questions were prevented.
This algorithm was devised taking into account the most common acute intoxication-type IEMs, such as urea cycle disorders, organic acidaemia, maple syrup urine disease and fatty acid oxidation defects. The algorithm steps (Fig. 1) were developed by the Ankara University Faculty of Medicine Department of Pediatric Metabolism based on international guidelines, reviews and clinical experience.16,20-25
For the creation of the QR codes, a web-based “QR-Code Generator”26 was utilized. The pediatric residents participating in the study accessed the disease management protocol in one step by scanning the QR code using their mobile phones, tablets, or computer cameras.
In the descriptive analysis of the data, mean±standard deviation was used for continuous variables with a normal distribution, median (25th and 75th percentiles, Q1-Q3) for variables with a non-normal distribution, and percentages for categorical variables. For comparisons of two groups, between-group differences in the means of the groups were analysed with a t-test, and differences in median values were analysed with a Mann-Whitney U test. When comparing percentages, Pearson’s chi-square or Fisher’s exact tests were used for independent variables, while the McNemar test was employed for dependent variables. A p-value less than 0.05 was considered statistically significant for all analyses. IBM SPSS Statistics for Macintosh (Version 22.0. Armonk, NY: IBM Corp.) was used for the analysis of data.
This study was approved by the Institutional Review Board (IRB) of Ankara University Faculty of Medicine Ethics Committee (Date: 15 February 2024, Number: İ02-117-24)
Results
Of the residents, 73 (64.6%) were female, and 40 (35.4%) were male, and the median age of the residents was 28.0 years (26.0–31.0) and the median duration of residency was 1.5 years (1.0–3.0). Among the residents, 42 (37.2%) had previously worked in the pediatric metabolism department of their institution, while three had worked in a metabolism department during external rotations, due to the lack of a metabolism department in their institution. Furthermore, 83 residents (73.5%) had worked in a pediatric emergency department, 83 (73.5%) in a pediatric intensive care and 82 (72.6%) in a neonatal intensive care department (Table I).
| Table I. Baseline characteristics of participants. | |||
|
|
|
|
|
| Resident Age, years | |||
| Median |
|
|
|
| (min-max) |
|
|
|
| [25th-75th] |
|
|
|
| Mean (Standard deviation) |
|
|
|
| Gender, n (%) | |||
| Female |
|
|
|
| Male |
|
|
|
| Duration of Residency, years | |||
| Median |
|
|
|
| (min-max) |
|
|
|
| [25th-75th] |
|
|
|
| Mean (Standard deviation) |
|
|
|
| Previously Worked in a Metabolism Department? n (%) | |||
| Yes |
|
|
|
| No |
|
|
|
| Previously Worked in a Pediatric Emergency Department? | |||
| Yes |
|
|
|
| No |
|
|
|
| Previously Worked in a Pediatric Intensive Care Department? n (%) | |||
| Yes |
|
|
|
| No |
|
|
|
| Previously Worked in a Neonatology Department? n (%) | |||
| Yes |
|
|
|
| No |
|
|
|
Of the total, 108 (95.6%) of the residents accurately identified the initial tests to be performed upon the patient’s first presentation, and the QR code directive did not support any significant changes in the initially requested tests. Information on respiratory alkalosis, hyperammonaemia and hypoglycaemia was provided alongside the patient’s laboratory results, and the QR code-based algorithm presented differential flowcharts to be applied for different acute intoxication-type IEMs, including fatty acid oxidation defects, urea cycle disorders, organic acidaemia and maple syrup urine disease (Fig. 1). One of the scenario questions focused on the identification of the priority initial treatment to be administered before proceeding with a differential diagnosis based on the provided laboratory information. Of the total, 88 residents (77.9%) before access to the QR code-based algorithm and 110 residents (97.3%) after access gave correct responses to the question (p<0.001), and a comparable difference was noted in both groups (respectively, Group 1 after accessing QR code vs. before accessing QR code: 80.5% vs. 97.4%, p<0.001; Group 2 after accessing QR code vs. before accessing QR code: 72.2% vs. 97.2%, p=0.004). The residents were then asked about the appropriate actions to take upon the development of hyperglycaemia in the patient (blood sugar 340 mg/dl), with some incorrect options available for selection, such as reducing the rate of glucose infusion or reducing the rate of dextrose infusion, both of which can lead to increased catabolism. Of the total, 64 residents (56.6%) answered the question correctly without using the QR code-based algorithm, whereas 104 residents (92.0%) answered correctly after accessing the QR code-based algorithm flowchart recommendations (p<0.001). The correct answer was to initiate insulin – an important step in increasing anabolism, and the contribution of the QR code-based algorithm to the correct identification of this crucial treatment step was observed in both Group 1 and Group 2 (respectively, Group 1 after accessing QR code vs. before accessing QR code: 58.4% vs. 93.5%, p<0.001; Group 2 after accessing QR code vs. before accessing QR code: 52.8% vs. 88.9%, p=0.002).
Of the total, 90 residents (79.6%) were able to determine a preliminary diagnosis for the scenario patient based on their existing knowledge, and this rate increased to 88.5% with QR code-based algorithm assistance (p=0.050). The residents not only considered the possibility of urea cycle disorders in the patient, but also took action to prepare for emergency treatments aimed at reducing ammonia levels, such as sodium benzoate and sodium phenylacetate, considering the advice received from the QR code-based algorithm. After being instructed to place treatment orders for the patient, only one resident (0.9%) provided the correct order without the QR code-based algorithm, while the use of the QR code-based algorithm resulted in 92 residents (81.4%) providing complete and accurate treatment orders with correct dosages (p<0.001).
When the hyperammonaemia persisted (ammonia: 680 μmol/L), despite the administration of ammonia-lowering treatments, and emergency haemodialysis was deemed necessary, the residents were asked for treatment recommendations. Of the total, 92 residents (81.4%) made this critical decision based on existing knowledge, and the number increased to 108 (95.6%) after accessing the QR code-based data, demonstrating a significant improvement (p <0.001). The benefit of the QR code-based algorithm in critical haemodialysis decision-making was found to be greater among the residents of the centre with a metabolism department (respectively, Group 1 after accessing QR code vs. before accessing QR code: 81.8% vs. 97.4%, p <0.001).
When asked about the specific metabolic tests to be requested to support a diagnosis, Group 1 residents answered correctly at a rate of 80.5% based on their existing knowledge, whereas Group 2 residents answered correctly at a rate of 69.4%. The QR code-based algorithm increased the correct response rate for the tests to be requested among all residents in both groups, from 77% to 90.3% (p=0.001). It was noted that the QR code-based algorithm was beneficial to both groups in terms of identifying the routine tests to be requested during subsequent follow-up visits (respectively, Group 1 after accessing QR code vs. before accessing QR code: 79.2% vs. 97.2%, p<0.001; Group 2 after accessing QR code vs. before accessing QR code: 72.2% vs. 97.2%, p=0.004). The final question regarding the scenario patient, who was born to a consanguineous marriage, concerned recommendations for future pregnancies. While 83% of the residents provided the correct information for genetic counselling, this number increased to 91.2% following the QR code-based algorithm recommendations (p<0.001).
When asked about their satisfaction with the QR code-based algorithm application, 104 of the residents (92.0%) reported being satisfied, assigning it an average score of 93.3 out of 100 (Table II).
|
Table II. Responses to patient scenarios with and without QR code algorithm. Scenario:
|
|||||||||
| Patient Scenario Questions, Correct Answer Rates, n (%) |
|
|
|
|
|
|
|
|
|
| Question 1: What tests should be performed initially for the patient? |
|
|
|
|
|
|
|
|
|
| Question 2: Respiratory alkalosis and hyperammonaemia (ammonia: 392 μmol/L), hypoglycaemia were detected in the patient. Acute phase reactants are negative. What should be the initial treatment approach in the emergency department? |
|
|
|
|
|
|
|
|
|
| Question 3: During follow-up, the patient's blood sugar is measured as 340 mg/dl, what would you do? |
|
|
|
|
|
|
|
|
|
| Question 4: What is the possible preliminary diagnosis for the patient and what should be the second-line treatments to be reached? |
|
|
|
|
|
|
|
|
|
| Question 5: Please provide medication orders for the patient. (Open-ended question) |
|
|
|
||||||
| - Correct answer |
|
|
|
|
|
|
|||
| - Incorrect answer |
|
|
|
|
|
|
|||
| - Incomplete answer |
|
|
|
|
|
|
|||
| - Unanswered |
|
|
|
|
|
|
|||
| Question 6: Despite initiating ammonia-lowering treatments, the patient's ammonia level continues to rise (ammonia: 680 μmol/L). What treatment should be applied at this stage? |
|
|
|
|
|
|
|
|
|
| Question 7: What are the priority metabolic tests to be requested for diagnosis? |
|
|
|
|
|
|
|
|
|
| Question 8: After the patient's general condition has improved and the diagnosis has been clarified, what are your recommendations for treatment follow-up? |
|
|
|
|
|
|
|
|
|
| Question 9: Which of the following tests should be scheduled when patients come for follow-up? |
|
|
|
|
|
|
|
|
|
| Question 10: The patient's mother mentions a desire to become pregnant again in the future, how would you inform the family? (Open-ended question) |
|
|
|
||||||
| - Correct answer |
|
|
|
|
|
|
|||
| - Incorrect answer |
|
|
|
|
|
|
|||
| - Unanswered |
|
|
|
|
|
|
|||
| Were you satisfied with the QR code? Yes |
|
|
|
|
|
|
|||
| QR code satisfaction score (out of 100) |
|
|
|
|
|
|
|||
Discussion
The QR code-based algorithm applied in the present study was found to be successful in correctly identifying life-saving recommendations for the management of acute intoxication-type inborn errors of metabolism. In metabolic emergencies such as hyperammonaemia, which are rare but pose a high risk of complications within hours, physicians easy access resources in the absence of sufficient experience or knowledge contributed significantly to effective patient management and addressed the urgent time-sensitive nature of treatment.
Medical training focuses on common diagnoses and treatments, but this study explored acute intoxication-type inborn errors of metabolism, a rare condition. Many physicians lack knowledge of rare diseases, leaving them unprepared to manage such cases.27 Studies show over 90% of physicians lack knowledge of rare conditions, with less than 5% confident in managing them. Over 75% believe curricula should include more training on diagnosing and managing rare diseases.27 Delays in diagnosing rare conditions significantly affect survival, with research showing that insufficient physician knowledge increases complications and mortality.28 These findings suggest that there is a need to disseminate educational materials on rare conditions, both during medical education and in postgraduate training.27,29-31
Providing access to digital databases through such tools as QR code applications, and thus providing easy access to such data as educational materials, algorithms and guidelines, could contribute to a transformative strategy for the more effective management of emergencies related to rare conditions.27,32
Diagnosing rare conditions is challenging for non-specialist physicians, as they often require distinguishing overlapping symptoms and specialized tests.33 While numerous guidelines exist in literature for the diagnosis and treatment of rare diseases, physician awareness and easy access to these guidelines are crucial for the effective management of these conditions.8,34 For physicians outside the field of rare diseases, quickly accessing resources and managing emergencies can be challenging. This study used a urea cycle disorder scenario, asking residents to diagnose based on findings like respiratory alkalosis, hyperammonaemia, and low urea using a QR code-based algorithm. The algorithm significantly improved pediatric residents’ diagnostic abilities and their ordering of crucial metabolic tests for higher-level referrals.
In urea cycle disorders, the priority is to stop catabolism, which raises ammonia levels. This is achieved by halting protein intake and initiating high-glucose intravenous hydration.16,35 Approximately three-quarters of the pediatric residents participating in our study were able to initiate this critical treatment based on their existing knowledge, while nearly all residents were able to do so after accessing the QR-code application. In response to the open-ended question, “Please provide medication orders for the patient,” only one resident physician was able to respond correctly before accessing the QR-code application but was a senior resident with previous experience in a centre with a metabolism department who completed rotations in the neonatal and intensive care units, and who had been involved in the management of numerous metabolic patients. Following the use of the QR code application, more than three-quarters of the residents correctly and comprehensively answered the medication order question, highlighting the contribution of the QR code algorithm to both the diagnosis and initial treatment processes.
Another crucial life-saving recommendation in our scenario relates to extracorporeal detoxification decisions (such as haemodialysis). Authors generally agree on the importance of the early initiation of haemodialysis.36,37 In the sixth step of our scenario, despite the initiation of ammonia-lowering treatments, the patient’s ammonia level was measured at 680 μmol/L. After accessing the QR code-based algorithm, the respondent physicians were able to make a prompt hemodialysis decision. It was observed that pediatric residents trained in centres with pediatric metabolism departments were able to make more effective decisions related to dialysis after accessing the QR code-based algorithms. In contrast, in the centre without a pediatric metabolism department, although there was an increase in the rate of dialysis decisions after accessing the QR code-based algorithms, the difference was not statistically significant. The small number of participants in Group 2 is a significant limitation of the present study and increasing the sample size may yield more accurate evidence-based results.
After stabilizing and managing the acute episode in patients, it is essential to ensure they are referred to specialized centers with third-level pediatric metabolism departments for comprehensive long-term care. These centers are equipped to provide the multidisciplinary expertise required for the ongoing management of metabolic disorders, including tailored treatment plans, dietary adjustments, and monitoring for potential complications. By including these referral steps in the algorithm, the goal is not only to guide resident physicians through the immediate management process but also to emphasize the importance of continuity of care. This approach aims to enhance the residents’ understanding of the broader, long-term needs of metabolic patients and foster awareness of the critical role that specialized care plays in improving patient outcomes. Our observations indicate that the QR code-based algorithm enhanced the education and awareness of resident physicians of the required tests during follow-up, as well as recommendations for future pregnancies. Genetic counselling based on detailed family information should be provided by an expert, as a crucial intervention.38 In Türkiye, with a consanguinity rate of 21%, they should consider that rare diseases inherited in an autosomal recessive manner may be more common than expected. Sharing scientific information with families at every stage in the prevision of healthcare services can play a crucial role in fostering healthier future generations.39
The digitalization of medical education and hybrid learning models have rapidly advanced worldwide, accelerated by the COVID-19 pandemic, familiarizing healthcare students and professionals with these methods.40 Studies show that new-generation physicians quickly adapt to digital materials, preferring softcopy resources on devices for their portability and information accessibility over hardcopy materials40-42 In the present study, the satisfaction levels of the resident physicians regarding the QR code-based algorithm were investigated, and nearly all reported being satisfied, giving very high ratings. This pioneering study in the field of rare conditions suggests that raising awareness among physicians and assisting them in the management of patients with life-saving critical interventions through this method can be considered a highly effective approach.
This preliminary study evaluates the use of a QR code and algorithm-based material for simulating patient management by pediatric residents, though with limitations. The design does not compare the QR code to a printed algorithm, and success depends on the combined material rather than the QR code alone. The authors suggest such algorithms could aid pediatric emergency management of IEM patients, given the difficulty of quickly accessing guidelines and literature. While simulation questions align with the algorithm and are multiple-choice, real-life cases are more complex. This study, while requiring further refinement for real-world application, offers a foundation for developing new digital tools.
The reason for dividing the residents into groups in our study is that participation was from two different centers, and the most significant distinction between these two centers is the presence or absence of a metabolism department. Working as a resident in a center with a metabolism department allows for certain experience with metabolic diseases through multidisciplinary patient management in other departments, even if the residents have not yet completed their metabolism rotation. We believe that the residents from these two centers have different levels of awareness and background knowledge regarding metabolic diseases. For this reason, we aimed to compare the two centers. However, the number of metabolic patients encountered by each resident is not the same. Therefore, as a subgroup analysis, we created subgroups of residents who had completed and not completed a rotation in the metabolism department. Another limitation of our study is that not all pediatric residents working in centers with a pediatric metabolism department have completed their metabolism rotation. However, due to frequent consultations that occur when they rotate through pediatric emergency, pediatric intensive care, neonatal intensive care, or other departments, they are generally well-versed in the approach to metabolic patients. The percentages for rotations in these departments are high as shown in Table I. Moreover, residents are required to undergo mandatory foundational metabolism training, assessed through an annual examination. Although they have not completed the rotation, the infrastructure of the center means that residents are accustomed to managing metabolic patients. Nevertheless, it can be discussed as a limitation that not all residents in Group 1, where the center has a metabolism department, have completed their metabolism rotation. Another significant limitation of our study is that the difficulty and quality levels of each question vary, and a discrimination index could not be calculated. For this reason, rather than creating a total score for all questions, each question was assessed based on its individual accuracy percentages. Nevertheless, future studies that can evaluate question quality and discrimination indices would be invaluable for assessing this algorithm.
Our algorithm, based on seven international guidelines, reviews, and clinical experience, requires further development and study. As a preliminary example, it tested a QR code-integrated homemade algorithm. Since pediatric residents mostly encounter common diseases, rare disease algorithms may mislead without proper training. Therefore, QR codes must be paired with detailed training before use on real patients. This study provides only preliminary findings.
In conclusion, the digitalization of our world is transforming the nature of educational materials accessed by resident physicians. There is a global preference for resources that are easily transportable and quickly accessible, and that provide the right amount of information needed. Considering the inadequate knowledge of physicians of rare conditions, we believe that scenario-based patient simulation training and the widespread adoption of QR code-based algorithms in emergency departments are necessary for improving the outcomes of patients who may otherwise face mortality or significant sequelae. Although the contribution to education was not measured during the data collection phase due to the design of this study, it is believed that further studies of this nature could make significant contributions to postgraduate and in-service training.
Acknowledgements
The authors thank Sasan Shoaei for assisting in the organization of participants.
Ethical approval
This study was approved by the Institutional Review Board (IRB) of Ankara University Faculty of Medicine (Date: 15 February 2024 Number: İ02-117-24).
Source of funding
The authors declare the study received no funding.
Conflict of interest
The authors declare that there is no conflict of interest.
References
- Nakamura Y, Muppala V, Nguyen BM. Using a QR code to register voters in a family medicine residency clinic. PRiMER 2021; 5: 27. https://doi.org/10.22454/PRiMER.2021.519685
- Kane SK, Wetzel EA, Niehaus JZ, et al. Development and implementation of a Quick Response (QR) code system to streamline the process for fellows’ evaluation in the Pediatric Intensive Care Unit (PICU) and the Neonatal Intensive Care Unit (NICU) at a large academic center. Cureus 2023; 15: e47462. https://doi.org/10.7759/cureus.47462
- Chen S, Liu T, Li X, et al. Health QR code application in the novel containment strategy and healthcare plan for pregnant women and children under quarantine during the summer outbreak of SARS-CoV-2 delta variant in Chengdu, China: an observational study. Risk Manag Healthc Policy 2021; 14: 4499-4510. https://doi.org/10.2147/RMHP.S335803
- Brodie K, Madden LL, Rosen CA. Applications of Quick Response (QR) codes in medical education. J Grad Med Educ 2020; 12: 138-140. https://doi.org/10.4300/JGME-D-19-00516.1
- Folt J, Lam P, Miller J, Goyal N. There’s an app for that: a mobile procedure logging application using quick response codes. West J Emerg Med 2020; 22: 71-73. https://doi.org/10.5811/westjem.2020.10.48724
- Mels A, Lemmenes D, Liston C, Cowling P. Use of QR codes to deliver evidence-based care to maternal and neonatal patients in emergency departments. Journal of Obstetric, Gynecologic & Neonatal Nursing (JOGGN) 2022; 51(Suppl. 4): S15. https://doi.org/10.1016/j.jogn.2022.06.024
- Miller J, Costa SG, Taylor DA, Buntine P. Rethinking consent processes for research in emergency departments. Emerg Med Australas 2021; 33: 753-755. https://doi.org/10.1111/1742-6723.13775
- Bousquet J, Samolinski B, Kaidashev I, et al. UCRAID (Ukrainian Citizen and refugee electronic support in Respiratory diseases, Allergy, Immunology and Dermatology) action plan. Allergy 2023; 78: 2581-2595. https://doi.org/10.1111/all.15855
- The Melbourne Vaccine Education Centre (MVEC). Guidance for differentiating anaphylaxis from acute stress response for vaccine providers and Emergency Departments. Available at: https://mvec.mcri.edu.au/guidance-for-differentiating-anaphylaxis-from-acute-stress-response-for-vaccine-providers-and-emergency-departments (Accessed on July 20, 2024).
- Bu F, Sun H, Li L, et al. Artificial intelligence-based internet hospital pharmacy services in China: perspective based on a case study. Front Pharmacol 2022; 13: 1027808. https://doi.org/10.3389/fphar.2022.1027808
- Baugh JJ, Oran R, Roberts T, Hankin M, Moore K, White BA. The QR code: a treatment for COVID-19 information overload. Am J Emerg Med 2021; 45: 613-614. https://doi.org/10.1016/j.ajem.2020.11.065
- Abualnadı D, Al-salaymeh A, Yousef F, Al Sukkar G. Hawa M. Using QR codes for improving the educational process of students with hearing loss. The Eurasia Proceedings of Educational and Social Sciences 2018; 11: 116-122.
- Koç N, Cömert TK. Knowledge and awareness level of healthcare professional candidate students on inherited metabolic diseases: a cross-sectional study. BMC Med Educ 2023; 23: 562. https://doi.org/10.1186/s12909-023-04548-y
- Bösch F, Landolt MA, Baumgartner MR, et al. Caregiver burden, and parents’ perception of disease severity determine health-related quality of life in paediatric patients with intoxication-type inborn errors of metabolism. Mol Genet Metab Rep 2022; 31: 100876. https://doi.org/10.1016/j.ymgmr.2022.100876
- Eminoğlu FT, Koç Yekedüz M, Doğulu N, et al. Inherited metabolic disorders in the neonatal intensive care unit: red flags to look out for. Pediatr Int 2022; 64: e14953. https://doi.org/10.1111/ped.14953
- Häberle J, Burlina A, Chakrapani A, et al. Suggested guidelines for the diagnosis and management of urea cycle disorders: first revision. J Inherit Metab Dis 2019; 42: 1192-1230. https://doi.org/10.1002/jimd.12100
- The Royal College of Paediatrics and Child Health (RCPCH). Management of children and young people with an acute decrease in conscious level - clinical guideline. Available at: https://www.rcpch.ac.uk/resources/management-children-young-people-acute-decrease-conscious-level-clinical-guideline (Accessed on June 15, 2024).
- British Inherited Metabolic Diseases Group (BIMDG). Guidelines. Available at: https://www.bimdg.org.uk/site/guidelines.asp (Accessed on June 14, 2024).
- Metabolic Support. Think Ammonia!. Available at: https://metabolicsupportuk.org/news-and-events/policy-hub/our-campaigns/think-ammonia-campaign (Accessed on June 4, 2024).
- Strauss KA, Puffenberger EG, Carson VJ. Maple syrup urine disease. 2006 Jan 30 [Updated 2020 Apr 23]. In: Adam MP, Feldman J, Mirzaa GM, et al, editors. GeneReviews®. Seattle (WA): University of Washington, Seattle; 1993-2024. Available at: https://www.ncbi.nlm.nih.gov/books/NBK1319 (Accessed on June 13, 2024).
- Vaidyanathan K, Narayanan MP, Vasudevan DM. Organic acidurias: an updated review. Indian J Clin Biochem 2011; 26: 319-325. https://doi.org/10.1007/s12291-011-0134-2
- Merritt JL, Norris M, Kanungo S. Fatty acid oxidation disorders. Ann Transl Med 2018; 6: 473. https://doi.org/10.21037/atm.2018.10.57
- Auron A, Brophy PD. Hyperammonemia in review: pathophysiology, diagnosis, and treatment. Pediatr Nephrol 2012; 27: 207-222. https://doi.org/10.1007/s00467-011-1838-5
- Batshaw ML, Tuchman M, Summar M, Seminara J; Members of the Urea Cycle Disorders Consortium. A longitudinal study of urea cycle disorders. Mol Genet Metab 2014; 113: 127-130. https://doi.org/10.1016/j.ymgme.2014.08.001
- Summar ML, Mew NA. Inborn errors of metabolism with hyperammonemia: urea cycle defects and related disorders. Pediatr Clin North Am 2018; 65: 231-246. https://doi.org/10.1016/j.pcl.2017.11.004
- QR Code Generator. Why did a QR Code or link bring me to the Help Center? Available at: https://support.qr-code-generator.com/hc/en-us/articles/7664232533133-Why-are-there-different-short-URLs-domains (Accessed on June 7, 2024).
- Walkowiak D, Domaradzki J. Are rare diseases overlooked by medical education? Awareness of rare diseases among physicians in Poland: an explanatory study. Orphanet J Rare Dis 2021; 16: 400. https://doi.org/10.1186/s13023-021-02023-9
- EURORDIS. The voice of 12000 patients. Experiences and expectations of rare disease patients on diagnosis and care in Europe. 2009. Available at: https://www.eurordis.org/IMG/pdf/voice_12000_patients/EUROR DISCARE_FULLBOOKr.pdf (Accessed on Aug 10, 2021).
- Schieppati A, Henter JI, Daina E, Aperia A. Why rare diseases are an important medical and social issue. Lancet 2008; 371: 2039-2041. https://doi.org/10.1016/S0140-6736(08)60872-7
- Richter T, Nestler-Parr S, Babela R, et al. Rare disease terminology and definitions-a systematic global review: report of the ISPOR rare disease special interest group. Value Health 2015; 18: 906-914. https://doi.org/10.1016/j.jval.2015.05.008
- Wise J. Rare diseases are overlooked by doctors, policy makers, and guidelines, says think tank. BMJ 2012; 345: e6604. https://doi.org/10.1136/bmj.e6604
- Fernandez N, Maizels M, Farhat W, et al. E-learning teaches attendings “how to” objectively assess pediatric urology trainees’ surgery skills for orchiopexy. J Pediatr Urol 2018; 14: 132.e1-132.e6. https://doi.org/10.1016/j.jpurol.2017.09.026
- Kuiper GA, Meijer OLM, Langereis EJ, Wijburg FA. Failure to shorten the diagnostic delay in two ultra-orphan diseases (mucopolysaccharidosis types I and III): potential causes and implications. Orphanet J Rare Dis 2018; 13: 2. https://doi.org/10.1186/s13023-017-0733-y
- Sreih AG, Cronin K, Shaw DG, et al. Diagnostic delays in vasculitis and factors associated with time to diagnosis. Orphanet J Rare Dis 2021; 16: 184. https://doi.org/10.1186/s13023-021-01794-5
- Nakamura K, Kido J, Mitsubuchi H, Endo F. Diagnosis and treatment of urea cycle disorder in Japan. Pediatr Int 2014; 56: 506-509. https://doi.org/10.1111/ped.12439
- Hediger N, Landolt MA, Diez-Fernandez C, Huemer M, Häberle J. The impact of ammonia levels and dialysis on outcome in 202 patients with neonatal onset urea cycle disorders. J Inherit Metab Dis 2018; 41: 689-698. https://doi.org/10.1007/s10545-018-0157-4
- Kido J, Nakamura K, Mitsubuchi H, et al. Long-term outcome and intervention of urea cycle disorders in Japan. J Inherit Metab Dis 2012; 35: 777-785. https://doi.org/10.1007/s10545-011-9427-0
- Nouri N, Nouri N, Tirgar S, et al. Consanguineous marriages in the genetic counseling centers of Isfahan and the ethical issues of clinical consultations. J Med Ethics Hist Med 2017; 10: 12.
- TUIK. Available at: https://www.tuik.gov.tr/ (Accessed on June 1, 2024).
- Çakmakkaya ÖS, Meydanlı EG, Kafadar AM, et al. Factors affecting medical students’ satisfaction with online learning: a regression analysis of a survey. BMC Med Educ 2024; 24: 11. https://doi.org/10.1186/s12909-023-04995-7
- Frenk J, Chen L, Bhutta ZA, et al. Health professionals for a new century: transforming education to strengthen health systems in an interdependent world. Lancet 2010; 376: 1923-1958. https://doi.org/10.1016/S0140-6736(10)61854-5
- Lucey CR, Davis JA, Green MM. We have no choice but to transform: the future of medical education after the COVID-19 pandemic. Acad Med 2022; 97: S71-S81. https://doi.org/10.1097/ACM.0000000000004526
Copyright and license
Copyright © 2025 The Author(s). This is an open access article distributed under the Creative Commons Attribution License (CC BY), which permits unrestricted use, distribution, and reproduction in any medium or format, provided the original work is properly cited.