Graphical Abstract
Abstract
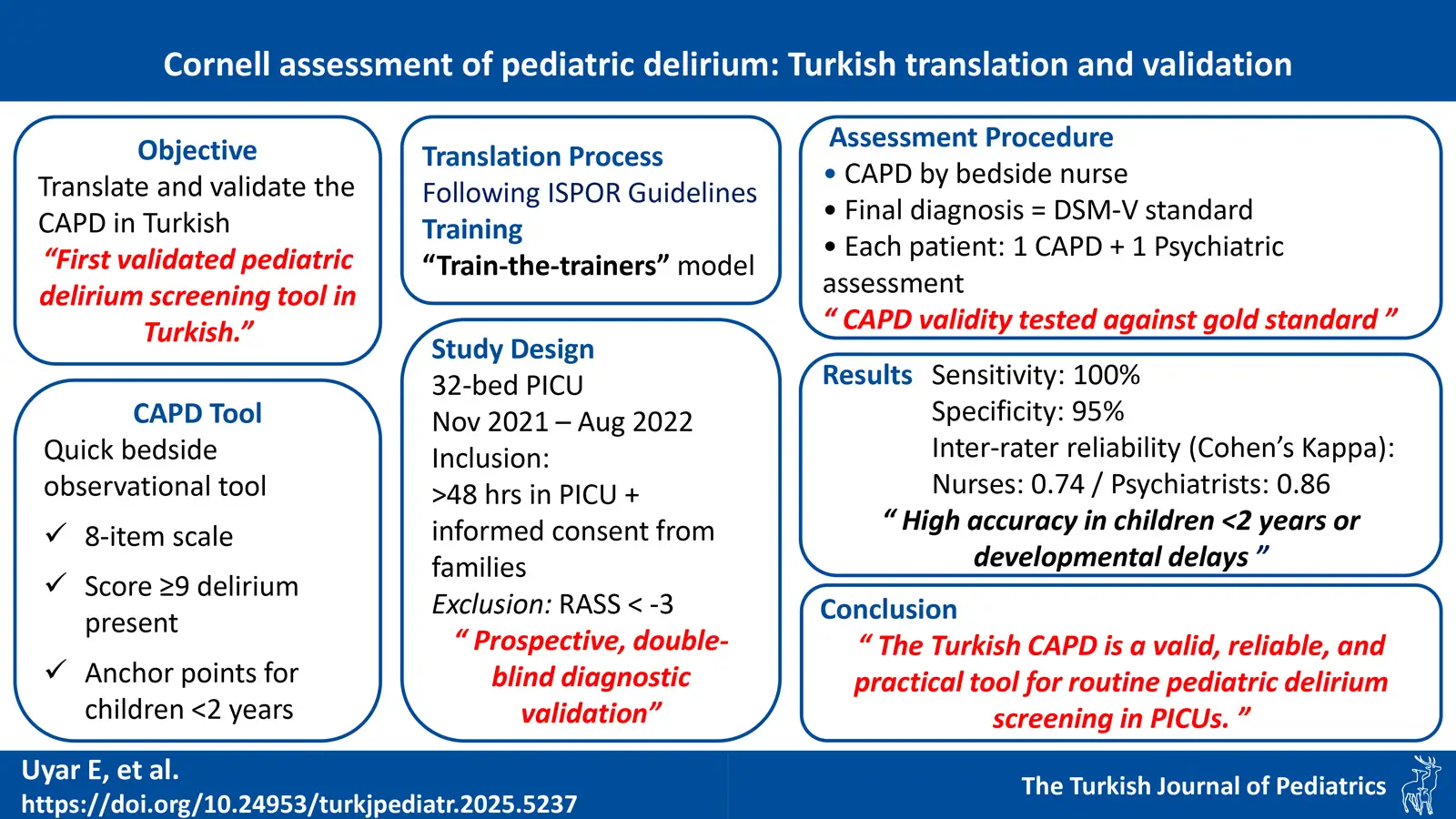
Background: Hypoactive delirium may go unrecognized unless routinely screened. At present, there is no valid screening tool for delirium in the Turkish language. This study was conducted to translate the Cornell Assessment of Pediatric Delirium (CAPD) into Turkish and to evaluate its validity and reliability.
Methods: In this is validation study, CAPD assessments were conducted by pediatric intensive care unit nurses and compared with assessments by a child psychiatrist.
Results: A total of 76 patients were included, 37 participants (48.6%) were younger than 24 months, and 22 participants (28.9%) had developmental disabilities. Prevalence of delirium was 25.0% (n=19). Inter-rater agreement for the identification of delirium by psychiatrists was strong and reliable, with a Cohen’s kappa value of 0.86 (95% confidence interval [CI]: 0.72-0.99). Inter-rater reliability for nurses was also significant, with a Cohen’s kappa of 0.74 (95% CI, 0.57-0.91). Inter-rater reliability ranged from 0.64 to 0.84 for each CAPD item except item 6, indicating reliable scoring. Sensitivity and specificity improved when the CAPD cut-off score was increased from 9 (100% and 95%, respectively) to 11 (100% and 98.02%, respectively). Subgroup analyses showed high sensitivity and specificity in patients with developmental delay (96%) and in patients under 2 years of age (96%) when the CAPD cut-off score was 9. However, specificity decreased slightly to 93% in patients under 6 months of age.
Conclusion: The Turkish CAPD, the first delirium screening scale translated into Turkish, has demonstrated validity and reliability in screening for delirium in children of all ages, including those with developmental disabilities.
Keywords: delirium, critical care, child, infant, language
Introduction
According to DSM-V criteria, delirium refers to an acute onset and fluctuating neurological disturbance involving consciousness and cognition over a brief period of time, and occurs in the presence of an underlying medical condition.1 The gold standard diagnosis of delirium is psychiatric evaluation. However, psychiatric evaluation is not feasible for routine monitoring of delirium in the pediatric intensive care unit (PICU) setting. Therefore, standardized and validated screening tools that enable rapid and reliable screening of patients in real-time are of the utmost importance.
Delirium occurs frequently in critically ill children. Although the prevalence of delirium in PICUs varies with regional and disease variations, an international large-sample study reported that one in four critically ill children had delirium.2 Studies have shown that pediatric delirium is associated with longer intensive care unit (ICU) stay3-5, increase in costs, prolonged mechanical ventilation and higher odds of death.2-9 Therefore, rapid recognition of delirium is important to allow for effective intervention. In recent years, several screening tools have been proposed for children admitted to the PICU, including the Pediatric Confusion Assessment Method for Intensive Care Unit (pCAM-ICU)10, the Sophia Observation Withdrawal Symptoms-Pediatric Delirium (SOS-PD) scale11 and the Cornell Assessment for Pediatric Delirium (CAPD).12 The CAPD is a quick and easy bedside tool based on the nurses’ observational assessments during care.3,13,14 It is designed to recognize all types of delirium for any pediatric age2,5,15,16, regardless of the presence of developmental disabilities.5,12,17 Since 2016, the European Society of Pediatric and Neonatal Intensive Care (ESPNIC) has recommended the CAPD as the assessment tool to diagnose delirium among children and infants (grade of recommendation: A).6 The CAPD has been internationally translated, adapted, and validated into Chinese, Japanese, Portuguese, Spanish, Italian and Danish.14,18-23 In a nationwide study, 57.9% of PICUs in Türkiye did not use any delirium screening tool and the number of centers where delirium screening was routinely and regularly performed was only three (15.8%).24
Currently, there is no validated Turkish screening tool for the diagnosis of pediatric delirium. The primary objectives of this study were to translate the CAPD from English to Turkish, ensure its cross-cultural adaptation, and to analyze the validity and reliability of the Turkish version. The secondary aim was to test the screening efficacy of the Turkish CAPD in specific subgroups, including developmental status and age categories.
Materials and Methods
Description of the CAPD
The CAPD is a screening tool for identifying symptoms of delirium. It consists of eight questions, each scored on a scale of 0 to 4, with responses ranging from ‘never’ to ‘always’. The total score ranges from 0 to 32, with a CAPD score of 9 or higher indicating the presence of delirium. Patients with a score of 9 or higher are categorized as “delirium present,” while those with a score below 9 are categorized as “delirium absent.” There are anchor points available to be used as a point of reference when scoring the CAPD in children under two years of age.15
Translation
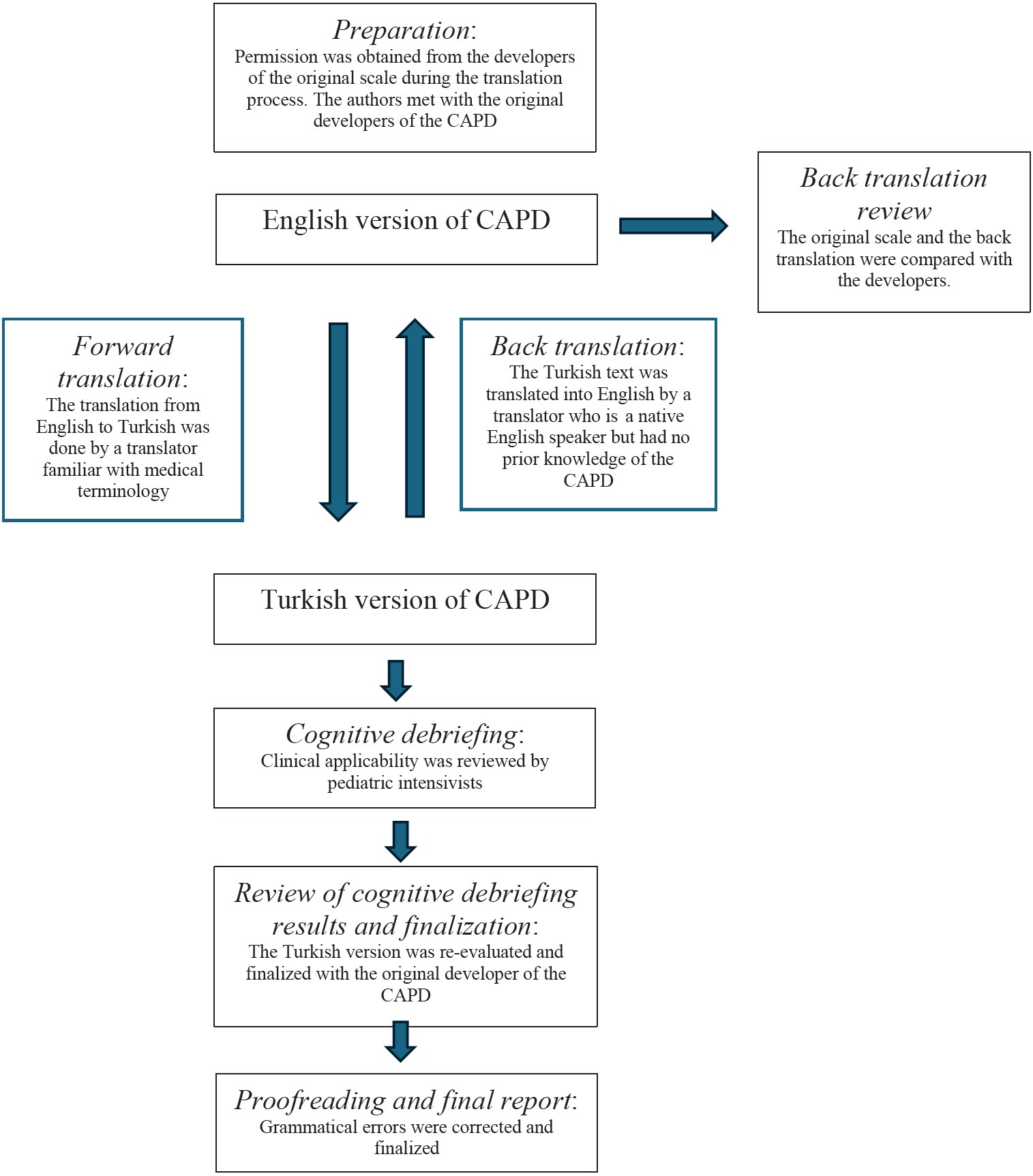
The CAPD was translated following the International Society for Pharmacoeconomics and Outcomes Research’s (ISPOR) good practice guidelines25 for translation and cross-cultural adaptation (Fig. 1). The following steps were followed in the process: 1. Preparation: Permission was obtained from the developers of the original scale during the translation process. The authors met with the original developers of the CAPD to understand the background and theory and to ensure the correct use and interpretation of the assessment tool. 2. Forward translation: The translation from English to Turkish was conducted by a translator familiar with medical terminology. 3. Back translation: The Turkish text was translated into English by a translator who is a native English speaker but had no prior knowledge of the CAPD. 4. Back translation review and harmonization: The original scale and back translation were compared by the developers. 5. Cognitive debriefing: Clinical applicability was reviewed by pediatric intensivists. 6. Review of cognitive debriefing results and finalization: The Turkish version was re-evaluated with the original author to ensure that it retained its original meaning. 7. Proofreading and final report: Grammatical errors were corrected and finalized.
Training
Training was provided by the original author of the CAPD to the PICU specialist leading the study. This specialist then organized training sessions for nurse leaders (a ‘train-the-trainers’ model). The nurses on the ward were then trained according to the original developer’s guidelines, with a maximum of three nurses attending each session. Thereafter, each PICU nurse had to complete three accurate CAPD assessments at the bedside in the presence of the supervisors, in order to be approved for independent delirium screening. Difficulties and questions in the assessment were clarified. Separately, the Child Psychiatry team organized a consensus session. A standardized psychiatric assessment form was created by consensus in accordance with the gold standard DSM-V criteria for pediatric delirium.
Assessing CAPD performance
This validation study was executed in a 32-bed medical-surgical PICU in a major urban academic medical center between November 2021 and August 2022. The study protocol was approved by the Institutional Review Board of Ankara City Hospital (No: E2-21-731, Date: 14.07.2021).
All patients who were admitted to the PICU for any reason and who had been in hospital for more than 48 hours were included in the study. Informed consent forms were obtained from the families during hospitalization. Patients without informed consent were excluded from the study. Thirty-two beds were numbered and a ’True Random Number Generator(’ tool (Randomness and Integrity Services LTD., Dublin, Ireland, www.random.org) was used to assign four bed numbers for each scheduled study day. If the same participant was part of the random selection, the participant had a maximum of four assessments. The definition of “significant clinical developmental delay” is on the basis of clinical evaluation and/or parental report of developmental problems affecting the child’s behavior or communication capability. Children with a history of mild or transient developmental problems (e.g., needing occupational therapy or having motor or speech delays) were not included in this category.12 Demographic and clinical data were recorded on each subject. The patient’s level of sedation was assessed with the Richmond Agitation and Sedation Scale (RASS)26 every four hours. If any of the selected beds had a patient with a RASS score less than -3 for the entire shift (i.e.: unarousable to verbal stimulation), CAPD scoring was not performed. Otherwise, the CAPD scores were assessed twice daily by the bedside nurse (Supplementary Tables S1, S2).
A set of double-blind matched nurse assessments were performed. The bedside nurse completed the CAPD as a paper checklist. Then, the supervisor nurse recorded the CAPD assessment. This was followed by an assessment by 2 blinded psychiatrists. If the child was diagnosed with delirium by either psychiatrist, the healthcare team was notified so that appropriate treatment could be given. Once inter-rater reliability was established, for the remainder of the study each patient had one CAPD and one psychiatric assessment. In our study, the DSM-V criteria were used as the gold standard for confirming the diagnosis of delirium, and the CAPD’s validity was evaluated by comparing its results with this diagnostic standard.
Statistics
Patient characteristics including demographics, reasons for admission, and level of sedation were summarized using descriptive statistics. Interrater reliability was quantified using Cohen’s κ coefficient.27,28 The receiver operating characteristic (ROC) analysis was performed to find the optimal CAPD cut-off score; subsequently, sensitivity and specificity were calculated for the overall sample. In addition, in order to explore CAPD performance in subgroups, validity measures were described by age groups and developmental status. All confidence intervals (CI) were adjusted for the possible correlation between observations within subjects using a ratio estimator method.29,30 Analyses were performed in R version 4.4.3 (R Foundation for Statistical Computing, Vienna, Austria).
Results
A total of 77 patients were enrolled in the study and 120 paired CAPD and psychiatric assessments were completed. One patient did not complete any study assessments. The remaining 76 patients completed at least one paired assessment (CAPD plus psychiatric evaluation). Thirty-eight nurses and three psychiatrists participated in study assessments.
Characteristics of the participants
Among the participants, 42 (55.3%) were male, and 37 (48.6%) were younger than 24 months. The age distribution of the participants is reported in Table I. Additionally, 22 participants (28.9%) had developmental delay. The diagnoses at the time of admission to the PICU and the underlying conditions can also be seen in Table I. Thirty-four participants (44.7%) received noninvasive ventilation, 23 participants (30.3%) received invasive mechanical ventilation, and 4 participants (5.3%) received supplemental oxygen. Fifteen participants (19.7%) were not receiving any form of respiratory support. In addition, 35 participants (46.1%) received sedation, 18 of whom (51.4%) received dexmedetomidine. The incidence of delirium was 25.0% (n=19 patients) according to the gold standard psychiatric assessment for the diagnosis of delirium. Of these cases, 10 (52.6%) patients had hyperactive delirium, 8 (42.1%) patients had hypoactive delirium, and 1 (5.3%) patient had a mixed type of delirium.
| a See text for description of categories. b Including all primary and secondary diagnoses | |
| Table I. Biological and clinical characteristics of the study cohort. | |
| Characteristic |
|
| Gender | |
| Male |
|
| Female |
|
| Age | |
| 0-24 mo |
|
| 2-5 yr |
|
| 6-12 yr |
|
| 13-18 yr |
|
| Developmental disabilitya | |
| No |
|
| Yes |
|
| Respiratory support | |
| Oxygen |
|
| Noninvasive mechanical ventilation |
|
| Ventilator |
|
| None |
|
| Diagnosesb | |
| Cardiac |
|
| Genetic disorder |
|
| Hematologic/oncologic |
|
| Infectious/Pneumonia |
|
| Bronchiolitis |
|
| Metabolic |
|
| Neurologic |
|
| Postoperative/other |
|
Criterion Standard and CAPD Performance
Inter-rater Reliability
The first 33 psychiatric assessments were performed independently by two psychiatrists, each blinded as to the other’s assessment. The concordance between the psychiatrist assessments was excellent, with a strong and reliable agreement (Cohen’s Kappa = 0.86, 95% CI: 0.72-0.99). The first 64 CAPD scores were performed independently by two nurses, each blinded as to the other’s assessment. The inter-rater reliability of nurses was 0.74 overall (Cohen’s Kappa = 0.74, 95% CI, 0.57-0.91). When each CAPD item was assessed individually, the inter-rater reliability ranged from 0.76 to 0.84 (indicating substantial to near-perfect agreement), except for item 6 (Cohen’s Kappa = 0.58, 95% CI: 0.39-0.77; Table II).
|
*Note for interpretability purposes that a Cohen’s Kappa of 0.41-0.60 denotes moderate agreement, 0.61-0.8 denotes substantial agreement, and 0.81-0.99 denotes near perfect agreement.34 CAPD: Cornell Assessment of Pediatric Delirium, CI: confidence interval. |
|
| Table II. Inter-rater reliability of individual CAPD items. | |
| Item |
|
| 1. Does the child make eye contact with the caregiver? |
|
| 2. Are the child’s actions purposeful? |
|
| 3. Is the child aware of his/her surroundings? |
|
| 4. Does the child communicate needs and wants? |
|
| 5. Is the child restless? |
|
| 6. Is the child inconsolable? / Is it difficult to calm the child? |
|
| 7. Is the child underactive -very little movement while awake? |
|
| 8. Does it take the child a long time to respond to interactions? |
|
The sensitivity and specificity for the 120 CAPD assessments were 100% and 95%, respectively, using a cut-off point of 9 or higher, consistent with the original CAPD validation study. In our study, the optimal cut-off that maximizes sensitivity and specificity is a CAPD score of 11. Using this cut-off, sensitivity is 100% and specificity is 98.02% (Supplementary Figure S1).
The gold standard psychiatric diagnosis showed a 96% agreement with the CAPD screening test. Among the participants, there were five false positives (children with a CAPD score of 9 or higher in whom the psychiatrist did not diagnose delirium).
Subgroup analyses of CAPD performance against the gold standard of psychiatric diagnosis showed high sensitivity (100%) and specificity (96%) for patients with developmental delay. CAPD performance showed high sensitivity (100%) and specificity (96%) in participants aged less than 2 years. In infants <6 months of age, sensitivity remained at 100% and specificity decreased slightly (93%).
Discussion
Without routine screening, the diagnosis of delirium – especially in children – is often missed. The absence of a pediatric delirium screening tool in the native language complicates the recognition, prevention, and appropriate treatment of pediatric delirium. Therefore, it is imperative to have a linguistically and culturally appropriate delirium screening tool available for use in Turkish PICUs.
The CAPD is the first screening tool for delirium to be translated into Turkish. This study shows that the Turkish version of the CAPD is both valid and reliable, and results are consistent with the gold-standard psychiatric assessment for delirium. Implementing routine screening for delirium in Turkish PICUs will increase awareness of pediatric delirium, and may reduce morbidity and improve care nationwide.
In many prospective studies, a CAPD score of 9 or above has been used as a definition for delirium.2,6,12,14,17,18,20,22,31-33 Our data were in agreement with these previous reports, with a sensitivity of 100% and specificity of 95% when using the same cut-off. In this study, we found that a cut-off score of 11 further increased specificity (98.02%) without sacrificing specificity (still 100%). Further studies in Turkish PICUs will be necessary to replicate this finding before changing the CAPD cut-off score.
In practice, the diagnosis of delirium is challenging in extremely young and/or developmentally delayed children.15 Similar to the English version of the CAPD12, we demonstrated good validity (100% sensitivity and 96% specificity) in detecting delirium in children younger than 2 years of age, with decreased specificity of the CAPD (93%) in patients younger than 6 months. However, in contrast with the reported literature, we demonstrated excellent specificity (96%) even in children with developmental disabilities. Kaur et al. showed an increase in specificity and positive diagnostic value from 66% to 97% and from 47% to 89%, respectively, when combining CAPD with RASS fluctuations in children with developmental delay compared to CAPD alone.17 We were aware of this finding when planning our current study and added a footnote to the final version of the Turkish CAPD: ’Fluctuation in RASS values (during at least six hours of follow-up) is a typical finding for delirium’, along with a checklist for RASS fluctuation (obvious/occasional/never). During the preparatory training of nurses, we stressed the significance of RASS fluctuations as indicative of changes in the patient’s level of consciousness. We believe that attention to RASS fluctuations when scoring the CAPD may have contributed to the nurses’ ability to identify delirium with high sensitivity and specificity, even in children with developmental disabilities.
The processes of translation and cross-cultural adaptation are complex and challenging. It is important to retain the characteristics of the original version while taking into account the regional use of expressions. The inter-rater reliability of the CAPD scores among nurses was 0.74 (Cohen’s Kappa = 0.74, 95% CI, 0.57-0.91). This indicates substantial agreement among nurses overall. For each individual item in the CAPD, inter-rater reliability ranged from 0.64 to 0.84 (substantial to near-perfect agreement), except for item 6 (“Is the child inconsolable?”), which showed only moderate agreement (Cohen’s Kappa = 0.58, 95% CI: 0.39-0.77). This is consistent with Hoshino et al.’s Japanese study which showed that item 6 had the lowest inter-rater agreement (Cohen’s Kappa 0.67).22 Japanese and Turkish belong to the same language family (Altaic language family) and the Altaic language family has a different sentence structure than the Euro-Indian language family. As a result, this relationship may be indicative of a translation problem. It is also notable that 4 out of the 5 patients who were falsely identified as delirious by the CAPD were of Syrian origin and did not speak Turkish. This language barrier made it difficult to calm the children. This may have led to decreased interrater reliability of item 6, as only some nurses spoke Arabic. To improve agreement for item 6, a discussion was held with the evaluators and it was suggested that wording for this item should be clarified. In our view, the translation of question 6 should be changed to “Çocuğu sakinleştirmek zor mu? (Is it difficult to calm the child?)”. This suggested modification may improve agreement between assessors and make communication more effective. We suggest that future studies in Turkish (and other) PICUs should consider evaluating the interrater reliability of item 6 with this alternate wording. Therefore, it is crucial to translate and validate original screening tools into various native languages according to guidelines.
There are some limitations to this study. It was conducted in a single institution. It needs to be replicated in a multi-institutional study. Patients with significant language barrier had a higher false positive rate, reflecting the difficulty in assessing these individuals. Further research is needed to replicate and address the best diagnostic approaches in this population, and the possibility of a higher CAPD cut-off point needs to be investigated in larger studies.
Conclusion
In conclusion, the Turkish version of the CAPD has high sensitivity and specificity compared to the criterion-standard psychiatric assessment. The Turkish CAPD is a valid and reliable screening tool for detecting and monitoring pediatric delirium in children of all ages and developmental stages.
Ethical approval
The study protocol was approved by the Institutional Review Board of Ankara City Hospital (date: 14.07.2021, number: E2-21-731).
Source of funding
The authors declare the study received no funding.
Conflict of interest
The authors declare that there is no conflict of interest.
References
- American Psychiatric Association (APA). Diagnostic and statistical manual of mental disorders: DSM-5. Washington, DC: APA; 2013. https://doi.org/10.1176/appi.books.9780890425596
- Traube C, Silver G, Reeder RW, et al. Delirium in critically ill children: an international point prevalence study. Crit Care Med 2017; 45: 584-590. https://doi.org/10.1097/CCM.0000000000002250
- Traube C, Silver G, Gerber LM, et al. Delirium and mortality in critically ill children: epidemiology and outcomes of pediatric delirium. Crit Care Med 2017; 45: 891-898. https://doi.org/10.1097/CCM.0000000000002324
- Traube C, Mauer EA, Gerber LM, et al. Cost associated with pediatric delirium in the ICU. Crit Care Med 2016; 44: e1175-e1179. https://doi.org/10.1097/CCM.0000000000002004
- Liviskie C, McPherson C, Luecke C. Assessment and management of delirium in the pediatric intensive care unit: a review. J Pediatr Intensive Care 2021; 12: 94-105. https://doi.org/10.1055/s-0041-1730918
- Harris J, Ramelet AS, van Dijk M, et al. Clinical recommendations for pain, sedation, withdrawal and delirium assessment in critically ill infants and children: an ESPNIC position statement for healthcare professionals. Intensive Care Med 2016; 42: 972-986. https://doi.org/10.1007/s00134-016-4344-1
- Alvarez RV, Palmer C, Czaja AS, et al. Delirium is a common and early finding in patients in the pediatric cardiac intensive care unit. J Pediatr 2018; 195: 206-212. https://doi.org/10.1016/j.jpeds.2017.11.064
- Patel AK, Biagas KV, Clarke EC, et al. Delirium in children after cardiac bypass surgery. Pediatr Crit Care Med 2017; 18: 165-171. https://doi.org/10.1097/PCC.0000000000001032
- Simone S, Edwards S, Lardieri A, et al. Implementation of an ICU bundle: an interprofessional quality improvement project to enhance delirium management and monitor delirium prevalence in a single PICU. Pediatr Crit Care Med 2017; 18: 531-540. https://doi.org/10.1097/PCC.0000000000001127
- Smith HA, Boyd J, Fuchs DC, et al. Diagnosing delirium in critically ill children: validity and reliability of the pediatric confusion assessment method for the intensive care unit. Crit Care Med 2011; 39: 150-157. https://doi.org/10.1097/CCM.0b013e3181feb489
- Ista E, van Beusekom B, van Rosmalen J, et al. Validation of the SOS-PD scale for assessment of pediatric delirium: a multicenter study. Crit Care 2018; 22: 309. https://doi.org/10.1186/s13054-018-2238-z
- Traube C, Silver G, Kearney J, et al. Cornell assessment of pediatric delirium: a valid, rapid, observational tool for screening delirium in the PICU. Crit Care Med 2014; 42: 656-663. https://doi.org/10.1097/CCM.0b013e3182a66b76
- Valdivia HR, Carlin KE. Determining interrater reliability of the cornell assessment of pediatric delirium screening tool among PICU nurses. Pediatr Crit Care Med 2019; 20: e216-e220. https://doi.org/10.1097/PCC.0000000000001896
- Simonsen BY, Lisby M, Traube C, Skovby P. The Cornell assessment of pediatric delirium: translation and inter-rater reliability in a Danish pediatric intensive care unit. Acta Anaesthesiol Scand 2019; 63: 900-904. https://doi.org/10.1111/aas.13369
- Silver G, Kearney J, Traube C, Hertzig M. Delirium screening anchored in child development: the Cornell assessment for pediatric delirium. Palliat Support Care 2015; 13: 1005-1011. https://doi.org/10.1017/S1478951514000947
- Siegel EJ, Groves AM, Silver G, Hojsak J, Lim CA, Traube C. Delirium in the NICU: a point prevalence study. Hosp Pediatr 2021; 11: e321-e326. https://doi.org/10.1542/hpeds.2020-005736
- Kaur S, Silver G, Samuels S, et al. Delirium and developmental disability: improving specificity of a pediatric delirium screen. Pediatr Crit Care Med 2020; 21: 409-414. https://doi.org/10.1097/PCC.0000000000002248
- Barbosa M, Duarte M, Bastos VCS, Andrade LB. Translation and cross-cultural adaptation of the Cornell assessment of pediatric delirium scale for the Portuguese language. Rev Bras Ter Intensiva 2018; 30: 195-200. https://doi.org/10.5935/0103-507X.20180033
- Fazio PC, Daverio M, Masola M, et al. Italian version of the Cornell assessment of pediatric delirium: evaluation of the scale reliability and ability to detect delirium compared to pediatric intensive care unit physicians clinical evaluation. Front Pediatr 2022; 10: 894589. https://doi.org/10.3389/fped.2022.894589
- Fernández-Carrión F, González-Salas E, Silver G, Traube C. Translation and cultural adaptation of Cornell assessment of pediatric delirium to Spanish. Pediatr Crit Care Med 2019; 20: 400-402. https://doi.org/10.1097/PCC.0000000000001853
- He S, Wang YL, Zuo ZL. Clinical application of the Chinese version of Cornell assessment of pediatric delirium: a pilot study. Zhonghua Er Ke Za Zhi 2019; 57: 344-349. https://doi.org/10.3760/cma.j.issn.0578-1310.2019.05.006
- Hoshino H, Matsuishi Y, Enomoto Y, et al. The validity and reliability of the Japanese version of the Cornell assessment of pediatric delirium. Pediatr Crit Care Med 2020; 21: e267-e273. https://doi.org/10.1097/PCC.0000000000002274
- Paterson RS, Kenardy JA, Dow BL, et al. Accuracy of delirium assessments in critically ill children: a prospective, observational study during routine care. Aust Crit Care 2021; 34: 226-234. https://doi.org/10.1016/j.aucc.2020.07.012
- Konca C, Anil AB, Küllüoglu EP, Luleyap D, Anil M, Tekin M. Evaluation of pediatric delirium awareness and management in pediatric intensive care units in Turkey. J Pediatr Intensive Care 2020; 11: 130-137. https://doi.org/10.1055/s-0040-1721507
- Wild D, Grove A, Martin M, et al. Principles of good practice for the translation and cultural adaptation process for Patient-Reported Outcomes (PRO) Measures: report of the ISPOR task force for translation and cultural adaptation. Value Health 2005; 8: 94-104. https://doi.org/10.1111/j.1524-4733.2005.04054.x
- Kerson AG, DeMaria R, Mauer E, et al. Validity of the Richmond Agitation-Sedation Scale (RASS) in critically ill children. J Intensive Care 2016; 4: 65. https://doi.org/10.1186/s40560-016-0189-5
- Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977; 33: 159-174.
- Pérez J, Díaz J, Garcia-Martin J, Tabuenca B. Systematic literature reviews in software engineering-enhancement of the study selection process using Cohen’s Kappa statistic. Journal of Systems and Software 2020; 168: 110657. https://doi.org/10.1016/j.jss.2020.110657
- Rao JN, Scott AJ. A simple method for the analysis of clustered binary data. Biometrics 1992; 48: 577-585.
- Zhou X, Obuchowski, NA., McClish, DK. Diagnostic medicine. New York: Wiley; 2002.
- Hong H, Guo C, Liu ZH, et al. The diagnostic threshold of Cornell assessment of pediatric delirium in detection of postoperative delirium in pediatric surgical patients. BMC Pediatr 2021; 21: 87. https://doi.org/10.1186/s12887-021-02538-x
- Mao D, Fu L, Zhang W. Construction and validation of an early prediction model of delirium in children after congenital heart surgery. Transl Pediatr 2022; 11: 954-964. https://doi.org/10.21037/tp-22-187
- Simeone S, Rea T, Gargiulo G, et al. Cornell assessment of pediatric delirium: Italian cultural validation and preliminary testing. Prof Inferm 2019; 72: 25-33. https://doi.org/10.7429/pi.2019.720125
- McHugh ML. Interrater reliability: the kappa statistic. Biochem Med (Zagreb) 2012; 22: 276-282. Available at: https://hrcak.srce.hr/file/132393 (Accessed on August 29, 2024).
Copyright and license
Copyright © 2025 The Author(s). This is an open access article distributed under the Creative Commons Attribution License (CC BY), which permits unrestricted use, distribution, and reproduction in any medium or format, provided the original work is properly cited.