Graphical Abstract
Abstract
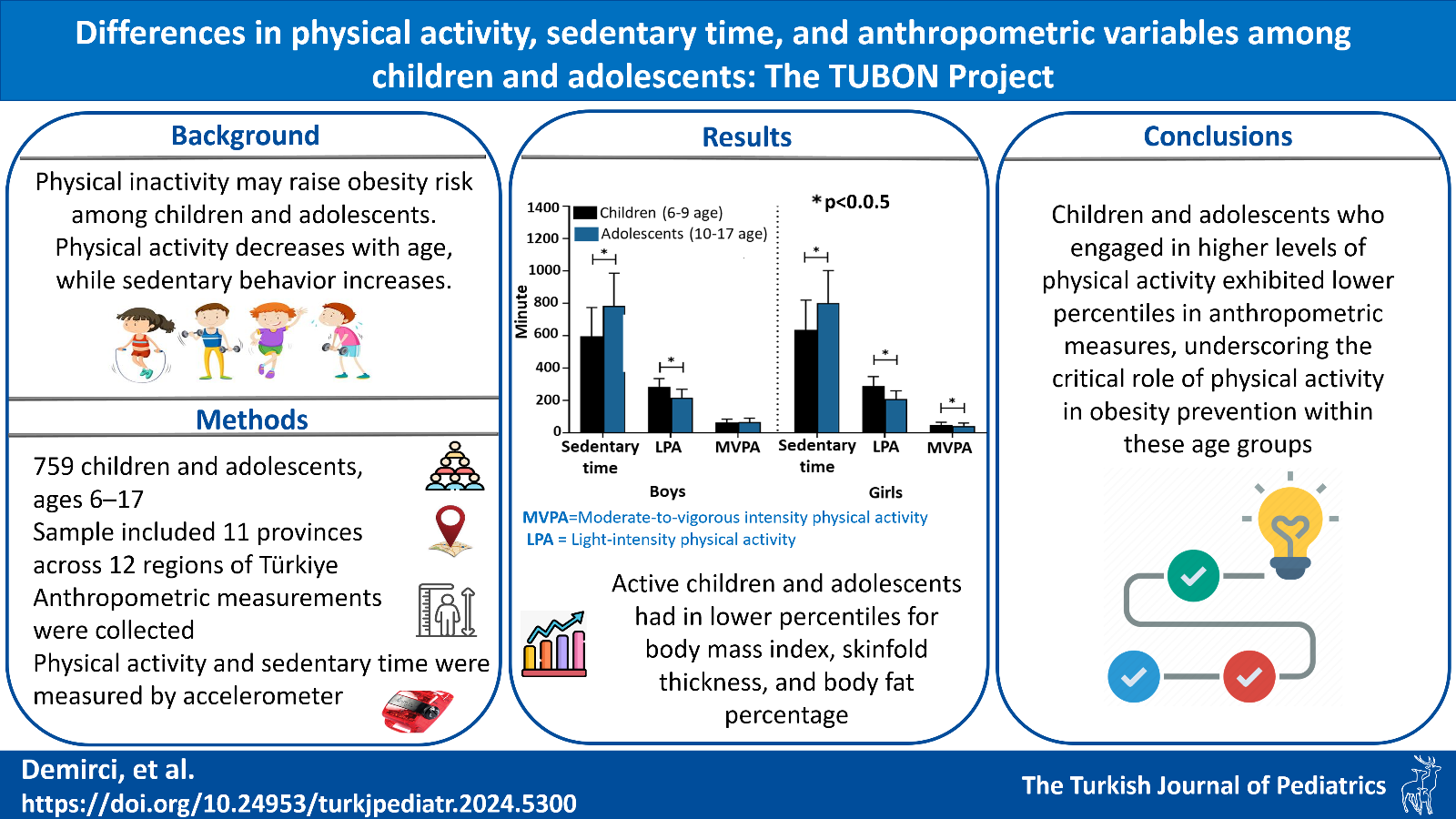
Background. Although physical inactivity may lead to increasing obesity prevalence, research on anthropometric variables changes based on physical activity (PA) in children and adolescents is limited. PA decreases with age, while sedentary behavior increases. The study aimed to examine differences in objectively measured sedentary time, light-intensity physical activity (LPA), and moderate-to-vigorous intensity physical activity (MVPA) between children and adolescents, and the differences in the percentiles of anthropometric variables between physically active and inactive groups according to World Health Organization PA recommendations.
Methods. A total of 759 participants aged 6-17 years (boys, n=358; girls, n=401) were included in the study. The ActiGraph wGT3x-BT accelerometer was used to measure sedentary time, LPA, and MVPA. Height, weight, waist circumference (WC), triceps skinfold thickness (T-SFT), and medial-calf skinfold thickness (M-SFT) were measured. Body fat percentage (BF%) and body mass index (BMI) were calculated, and the percentiles of anthropometric variables were categorized.
Results. The findings showed that children had less sedentary time and a higher LPA than adolescents for both genders (p<0.05). Children had a higher MVPA than adolescents in girls (p<0.05), but the difference was insignificant in boys (p>0.05). In boys, physically active children were in lower percentiles for T-SFT and BF% than those who did not (p<0.05). In boys, adolescents who were physically inactive were in higher percentiles for BMI, T-SFT, M-SFT, and BF% (p<0.05). In addition, in girls, adolescents who were physically active were in lower percentiles of BMI, M-SFT, and BF%, whereas children who were physically active were in lower percentiles of M-SFT and BF% (p<0.05).
Conclusion. Sedentary time increases while PA decreases with age. Children and adolescents who met the WHO PA recommendation had lower percentiles of anthropometric variables, indicating the importance of PA in preventing obesity in these age groups.
Keywords: physical activity, sedentary time, anthropometry, children, adolescents
References
- World Health Organization (WHO). WHO guidelines on physical activity and sedentary behaviour. 2020. Available at: https://www.who.int/publications/i/item/9789240015128 (Accessed on May 22, 2022).
- Tan VP, Macdonald HM, Kim S, et al. Influence of physical activity on bone strength in children and adolescents: a systematic review and narrative synthesis. J Bone Miner Res 2014; 29: 2161-2181. https://doi.org/10.1002/jbmr.2254
- Hills AP, Andersen LB, Byrne NM. Physical activity and obesity in children. Br J Sports Med 2011; 45: 866-870. https://doi.org/10.1136/bjsports-2011-090199
- Farooq A, Martin A, Janssen X, et al. Longitudinal changes in moderate-to-vigorous-intensity physical activity in children and adolescents: a systematic review and meta-analysis. Obes Rev 2020; 21: e12953. https://doi.org/10.1111/obr.12953
- Marques A, Minderico C, Martins S, Palmeira A, Ekelund U, Sardinha LB. Cross-sectional and prospective associations between moderate to vigorous physical activity and sedentary time with adiposity in children. Int J Obes (Lond) 2016; 40: 28-33. https://doi.org/10.1038/ijo.2015.168
- Riso EM, Kull M, Mooses K, Hannus A, Jürimäe J. Objectively measured physical activity levels and sedentary time in 7-9-year-old Estonian schoolchildren: independent associations with body composition parameters. BMC Public Health 2016; 16: 346. https://doi.org/10.1186/s12889-016-3000-6
- Steele RM, van Sluijs EM, Cassidy A, Griffin SJ, Ekelund U. Targeting sedentary time or moderate- and vigorous-intensity activity: independent relations with adiposity in a population-based sample of 10-y-old British children. Am J Clin Nutr 2009; 90: 1185-1192. https://doi.org/10.3945/ajcn.2009.28153
- Loprinzi PD, Cardinal BJ, Lee H, Tudor-Locke C. Markers of adiposity among children and adolescents: implications of the isotemporal substitution paradigm with sedentary behavior and physical activity patterns. J Diabetes Metab Disord 2015; 14: 46. https://doi.org/10.1186/s40200-015-0175-9
- Moura BP, Rufino RL, Faria RC, Amorim PRS. Effects of isotemporal substitution of sedentary behavior with light-intensity or moderate-to-vigorous physical activity on cardiometabolic markers in male adolescents. PLoS One 2019; 14: e0225856. https://doi.org/10.1371/journal.pone.0225856
- Volpato LA, Fernandes DZ, Correa RC, et al. Light-intensity physical activity patterns and associated factors in adolescents. Mot Rev Educ Fis 2021; 27: e1021020172. https://doi.org/10.1590/s1980-65742021017220
- Jiménez-Pavón D, Fernández-Vázquez A, Alexy U, et al. Association of objectively measured physical activity with body components in European adolescents. BMC Public Health 2013; 13: 667. https://doi.org/10.1186/1471-2458-13-667
- Schwarzfischer P, Weber M, Gruszfeld D, et al. BMI and recommended levels of physical activity in school children. BMC Public Health 2017; 17: 595. https://doi.org/10.1186/s12889-017-4492-4
- Janssen I, Leblanc AG. Systematic review of the health benefits of physical activity and fitness in school-aged children and youth. Int J Behav Nutr Phys Act 2010; 7: 40. https://doi.org/10.1186/1479-5868-7-40
- Füssenich LM, Boddy LM, Green DJ, et al. Physical activity guidelines and cardiovascular risk in children: a cross sectional analysis to determine whether 60 minutes is enough. BMC Public Health 2016; 16: 67. https://doi.org/10.1186/s12889-016-2708-7
- Chaput JP, Willumsen J, Bull F, et al. 2020 WHO guidelines on physical activity and sedentary behaviour for children and adolescents aged 5-17 years: summary of the evidence. Int J Behav Nutr Phys Act 2020; 17: 141. https://doi.org/10.1186/s12966-020-01037-z
- Ortega FB, Konstabel K, Pasquali E, et al. Objectively measured physical activity and sedentary time during childhood, adolescence and young adulthood: a cohort study. PLoS One 2013; 8: e60871. https://doi.org/10.1371/journal.pone.0060871
- Troiano RP, Berrigan D, Dodd KW, Mâsse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc 2008; 40: 181-188. https://doi.org/10.1249/mss.0b013e31815a51b3
- World Health Organization (WHO). Adolescent health. 2024. Available at: https://www.who.int/health-topics/adolescent-health#tab=tab_1 (Accessed on July 5, 2024).
- Sember V, Jurak G, Kovač M, Đurić S, Starc G. Decline of physical activity in early adolescence: a 3-year cohort study. PLoS One 2020; 15: e0229305. https://doi.org/10.1371/journal.pone.0229305
- Gordon CC, Chumlea WC, Roche AF. Stature, recumbent length, and weight. In: Lohman T, Roche A, Martorell R, editors. Measurement Descriptions and Techniques. Anthropometric standardization reference manual. Champaign, IL: Human Kinetics Books; 1988: 3-8.
- Callaway CW, Chumlea WC, Bouchard C, et al. Circumferences. In: Lohman T, Roche A, Martorell R, editors. Anthropometric standardization reference manual. Champaign, IL: Human Kinetics Books; 1988: 39-54.
- Surendar J, Indulekha K, Deepa M, Mohan V, Pradeepa R. Association of adiposity, measured by skinfold thickness, with parental history of diabetes in a South Indian population: data from CURES-114. Postgrad Med J 2016; 92: 379-385. https://doi.org/10.1136/postgradmedj-2015-133363
- Slaughter MH, Lohman TG, Boileau RA, et al. Skinfold equations for estimation of body fatness in children and youth. Hum Biol 1988; 60: 709-723.
- Dezenberg CV, Nagy TR, Gower BA, Johnson R, Goran MI. Predicting body composition from anthropometry in pre-adolescent children. Int J Obes Relat Metab Disord 1999; 23: 253-259. https://doi.org/10.1038/sj.ijo.0800802
- Fryar CD, Carroll MD, Gu Q, Afful J, Ogden CL. Anthropometric reference data for children and adults: United States, 2015-2018. Vital Health Stat 3 2021; 36: 1-44.
- Çiçek B, Öztürk A, Mazıcıoğlu MM, Kurtoğlu S. Arm anthropometry indices in Turkish children and adolescents: changes over a three-year period. J Clin Res Pediatr Endocrinol 2014; 6: 216-226. https://doi.org/10.4274/Jcrpe.1574
- Kuhle S, Ashley-Martin J, Maguire B, Hamilton DC. Percentile curves for skinfold thickness for Canadian children and youth. PeerJ 2016; 4: e2247. https://doi.org/10.7717/peerj.2247
- Soylu M, Şensoy N, Doğan İ, Doğan N, Mazıcıoğlu MM, Öztürk A. Four-site skinfolds thickness percentiles of schoolchildren and adolescents in Turkey. Public Health Nutr 2021; 24: 5414-5425. https://doi.org/10.1017/S1368980021003323
- Centers for Disease Control and Prevention (CDC). Child and teen BMI categories. 2024. Available at: https://www.cdc.gov/bmi/child-teen-calculator/bmi-categories.html (Accessed on May 25, 2024).
- Cain KL, Sallis JF, Conway TL, Van Dyck D, Calhoon L. Using accelerometers in youth physical activity studies: a review of methods. J Phys Act Health 2013; 10: 437-450. https://doi.org/10.1123/jpah.10.3.437
- Colley R, Connor Gorber S, Tremblay MS. Quality control and data reduction procedures for accelerometry-derived measures of physical activity. Health Rep 2010; 21: 63-69.
- Evenson KR, Catellier DJ, Gill K, Ondrak KS, McMurray RG. Calibration of two objective measures of physical activity for children. J Sports Sci 2008; 26: 1557-1565. https://doi.org/10.1080/02640410802334196
- World Health Organization (WHO). The Global Action for Measurement of Adolescent health (GAMA). 2024. Available at: https://www.who.int/groups/the-global-action-for-measurement-of-adolescent-health (Accessed on July 8, 2024).
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988.
- Pearson N, Haycraft E, P Johnston J, Atkin AJ. Sedentary behaviour across the primary-secondary school transition: a systematic review. Prev Med 2017; 94: 40-47. https://doi.org/10.1016/j.ypmed.2016.11.010
- Colley RC, Garriguet D, Janssen I, et al. The association between accelerometer-measured patterns of sedentary time and health risk in children and youth: results from the Canadian Health Measures Survey. BMC Public Health 2013; 13: 200. https://doi.org/10.1186/1471-2458-13-200
- Cooper AR, Goodman A, Page AS, et al. Objectively measured physical activity and sedentary time in youth: the International Children’s Accelerometry Database (ICAD). Int J Behav Nutr Phys Act 2015; 12: 113. https://doi.org/10.1186/s12966-015-0274-5
- Spittaels H, Van Cauwenberghe E, Verbestel V, et al. Objectively measured sedentary time and physical activity time across the lifespan: a cross-sectional study in four age groups. Int J Behav Nutr Phys Act 2012; 9: 149. https://doi.org/10.1186/1479-5868-9-149
- Corder K, Sharp SJ, Atkin AJ, et al. Change in objectively measured physical activity during the transition to adolescence. Br J Sports Med 2015; 49: 730-736. https://doi.org/10.1136/bjsports-2013-093190
- Young DR, Cohen D, Koebnick C, et al. Longitudinal associations of physical activity among females from adolescence to young adulthood. J Adolesc Health 2018; 63: 466-473. https://doi.org/10.1016/j.jadohealth.2018.05.023
- Adami F, Benedet J, Takahashi LAR, da Silva Lopes A, da Silva Paiva L, de Vasconcelos FAG. Association between pubertal development stages and body adiposity in children and adolescents. Health Qual Life Outcomes 2020; 18: 93. https://doi.org/10.1186/s12955-020-01342-y
- Mateo-Orcajada A, González-Gálvez N, Abenza-Cano L, Vaquero-Cristóbal R. Differences in physical fitness and body composition between active and sedentary adolescents: a systematic review and meta-analysis. J Youth Adolesc 2022; 51: 177-192. https://doi.org/10.1007/s10964-021-01552-7
- Sivrikaya K, Ziyagil MA, Çebi M. Relationship between body mass index and skinfold thickness in exercised and sedentary boys and girls. Univers J Educ Res 2019; 7: 48-54. https://doi.org/10.13189/ujer.2019.070107
- Agata K, Monyeki MA. Association between sport participation, body composition, physical fitness, and social correlates among adolescents: the PAHL study. Int J Environ Res Public Health 2018; 15: 2793. https://doi.org/10.3390/ijerph15122793
- Chaput JP, Lambert M, Mathieu ME, Tremblay MS, O’ Loughlin J, Tremblay A. Physical activity vs. sedentary time: independent associations with adiposity in children. Pediatr Obes 2012; 7: 251-258. https://doi.org/10.1111/j.2047-6310.2011.00028.x
- Gába A, Mitáš J, Jakubec L. Associations between accelerometer-measured physical activity and body fatness in school-aged children. Environ Health Prev Med 2017; 22: 43. https://doi.org/10.1186/s12199-017-0629-4
- Velde GT, Plasqui G, Willeboordse M, Winkens B, Vreugdenhil A. Associations between physical activity, sedentary time and cardiovascular risk factors among Dutch children. PLoS One 2021; 16: e0256448. https://doi.org/10.1371/journal.pone.0256448
- Mitchell JA, Dowda M, Pate RR, et al. Physical activity and pediatric obesity: a quantile regression analysis. Med Sci Sports Exerc 2017; 49: 466-473. https://doi.org/10.1249/MSS.0000000000001129
- Dencker M, Thorsson O, Karlsson MK, Lindén C, Wollmer P, Andersen LB. Daily physical activity related to aerobic fitness and body fat in an urban sample of children. Scand J Med Sci Sports 2008; 18: 728-735. https://doi.org/10.1111/j.1600-0838.2007.00741.x
- Zheng Y, Liang J, Zeng D, et al. Association of body composition with pubertal timing in children and adolescents from Guangzhou, China. Front Public Health 2022; 10: 943886. https://doi.org/10.3389/fpubh.2022.943886
- Reid RE, Fillon A, Thivel D, et al. Can anthropometry and physical fitness testing explain physical activity levels in children and adolescents with obesity? J Sci Med Sport 2020; 23: 580-585. https://doi.org/10.1016/j.jsams.2019.12.005
- Stierman B, Ogden CL, Yanovski JA, Martin CB, Sarafrazi N, Hales CM. Changes in adiposity among children and adolescents in the United States, 1999-2006 to 2011-2018. Am J Clin Nutr 2021; 114: 1495-1504. https://doi.org/10.1093/ajcn/nqab237
- Basterfield L, Reilly JK, Pearce MS, et al. Longitudinal associations between sports participation, body composition and physical activity from childhood to adolescence. J Sci Med Sport 2015; 18: 178-182. https://doi.org/10.1016/j.jsams.2014.03.005
Copyright and license
Copyright © 2024 The Author(s). This is an open access article distributed under the Creative Commons Attribution License (CC BY), which permits unrestricted use, distribution, and reproduction in any medium or format, provided the original work is properly cited.