Graphical Abstract
Abstract
Background. Child sexual abuse (CSA) is a severe problem with physical, emotional, social, moral, cultural, and legal dimensions, which is estimated to be quite common worldwide.
Methods. In this retrospective study including 262 CSA cases admitted to our outpatient clinic between 2013 and 2022, we examine the characteristics of the victim and the abuse and examination findings in cases of CSA.
Results. In our study, most of the victims were females over the age of 12, and most of the suspects were known to the child. Approximately half of the incidents (50.1%) occurred in a home. These data are essential in determining the risk factors of CSA cases and in terms of early detection and timely prevention. Vaginal penetration (40.8%) and anal penetration (32.4%) are frequently present in the history of CSA victims. A history of vaginal penetration was associated with acute and healed laceration findings in the hymen (p<0.05). Similarly, a history of anal penetration was associated with decreased sphincter tone, ecchymosis and abrasion in the anal mucosa, reflex anal dilatation, and acute anal fissure findings (p<0.05). As the time between the abuse and the examination increased, examination findings decreased in the anogenital region, which can heal quite quickly and without leaving a trace.
Conclusions. Preventing CSA is possible by analyzing risk factors well and reaching at-risk cases as early as possible. Acute and non-acute hymeneal lacerations that may be associated with vaginal penetration, anal fissure and other traumatic findings that may be associated with anal penetration should be carefully reviewed. However, it should be kept in mind that anogenital injuries with rapid regeneration ability may heal without leaving any symptoms and abuse may occur without leaving any symptoms.
Keywords: child sexual abuse, anogenital examination
Introduction
Child sexual abuse (CSA) is a worldwide severe problem with physical, emotional, social, moral, cultural, and legal dimensions.1,2 The prevalence of CSA varies according to the characteristics of the population and the definition used. Since it is widespread that many victims of sexual abuse never report the abuse, it is not possible to obtain precise statistical data on the prevalence of CSA.3,4
Determining the risk factors of child sexual abuse and taking measures in this direction is very important in terms of preventing the recurrence of the abuses that have occurred and preventing the abuses that are likely to occur. In a meta-analysis conducted by Assink et al.5 on risk factors for CSA victimization, it was reported that the child being of the female gender, the child and family members being victims of forensic cases (sexual assault or other), parental problems such as mental health problems and intimate partner violence, low parental competence, poor quality parent-child relationship, non-nuclear family structure, family problems, and child problems were closely related to CSA.
The findings to be detected in the examination of CSA cases, which require experience and meticulousness from the social and pediatric-gynecological history of the child to anogenital examination, play an essential role in revealing sexual abuse. These findings include concrete medical findings such as ecchymosis, abrasions, acute lacerations, healed (non-acute) lacerations (transection) and decreased anal sphincter tone.6-9 Adams et al.10-12 published a series of articles that serve as a guideline for evaluating anogenital findings, which was last updated by Kellogg et al.13 in 2023. Distinguishing these traumatic findings from normal anatomy and anatomical variations and evaluating them as concrete findings of sexual abuse is of utmost importance for the protection of the victim from possible repeated sexual abuse and more severe physical and psychological consequences and a fair trial process. Factors that may increase the incidence of concrete findings of sexual abuse, such as the time between sexual contact and examination, type of sexual contact (with or without penetration), pain, and bleeding symptoms, have been frequently researched in the literature. In addition, it should be kept in mind that sexual abuse may occur without leaving any traumatic findings. Since it is known that the perianal region heals rapidly without leaving any findings, the anogenital examination may not reveal any findings to support sexual abuse, especially in cases where time has elapsed.14-16
In our study, we analyzed the socio-demographic characteristics of the cases that were admitted to our outpatient clinic and the characteristics of sexual abuse. We compared and discussed the medical history and examination findings of the children with the literature data. One of the aims of our study is to prevent CSA by contributing to the early detection of children at risk of CSA. In addition, there are some sexual abuse examination findings in the literature that do not have an expert consensus. This study, in which we present the history and examination findings of CSA, will contribute to the literature in developing these controversial findings. An important hypothesis of our study is to emphasize how useful examinations performed on time and by well-equipped physicians in accordance with the literature information are in revealing children who are victims of sexual abuse.
Materials and Methods
Our study was initiated with the approval of Pamukkale University Non-Interventional Clinical Research Ethics Committee dated 31.05.2023 and numbered E-60116787-020-374178.
CSA suspected cases are referred to our outpatient clinic for CSA examination with an official document by the prosecutor’s office or the criminal courts. CSA examinations are performed in cases referred to the outpatient clinic of Pamukkale University Faculty of Medicine, Department of Forensic Medicine after obtaining the consent of the children and the written informed consents of the parents or children’s guardians. All archive records in our archive between 2013 and 2022 were retrospectively reviewed. By analyzing the archive files, 262 cases were referred for CSA examination, and the number of cases examined and reported was determined from a total of 1991 cases under the age of 18. Age, gender, degree of closeness of the suspect (intra-familial; father, sibling, husband, relative, extra-familial; boyfriend, engaged, neighbor, friend, stranger), location of the incident, repeated sexual abuse, duration of application to forensic units (0-5 days, 6-10 days, 11-30 days, 1-3 months, 4-12 months and >1 years), type of sexual abuse (including oral, anal and vaginal penetration, not including penetration) and acute (including bleeding, edema or inflammation) or non-acute (healed trauma findings) anogenital examination findings were categorized. Sample size was calculated using G*Power 3.1.9.7. Using a large effect size (w = 0.50), alpha of 0.05, 95% power and a 5% margin of error, a sample of 119 participants was calculated.
Statistical evaluations were performed using the SPSS (Statistical Package for the Social Sciences) version 21.0 package program. Continuous variables were expressed as mean ± standard deviation (SD), and categorical variables as number and percentage. Shapiro Wilk test was used to examine the suitability of the data for normal distribution. Mann Whitney U test was used for the data for which parametric test assumptions were not met. The chi-square test was used for categorical variables. The significance value was accepted as p<0.05 at a 95% confidence interval in the analyses.
Results
Of the 262 CSA cases included in our study, 23.7% (n=62) were male and 76.3% (n=200) were female. The mean age of males was 11.68 years (SD=3.458), and the mean age of females was 13.73 years (SD=3.273). A significant difference was found between the ages of male and female cases (U=3735.50, p<0.001). When the cases were categorized as 0-2 years, 3-6 years, 7-11 years, and 12-17 years according to their ages, it was seen that the 12-17 age group, which constituted the majority of the cases (77.5%), was the most frequently admitted.
When the cases were analyzed in terms of recurrent sexual abuse and the degree of closeness of the suspects recorded in the history, it was found that 43.1% (n=113) of 262 sexual abuse cases had a history of recurrent sexual abuse. It was observed that 81.8% (n=9) of 11 cases who were alleged to have been sexually abused by their fathers had a history of recurrent sexual abuse. It was found that 83.3% (n=10) of 12 cases who were alleged to have been sexually abused by a stranger had a history of non-recurrent sexual abuse, and these findings were statistically significant (p<0.05, Table I).
|
In some cases, there is more than one suspect. Row percentages are given. *neighbor, friend etc. ** boyfriend, engaged ***p<0.05 |
||||
| Table I. Distribution of recurrent and non-recurrent sexual abuse cases according to the degree of closeness of the suspects. | ||||
| Suspect | Non-recurrent, n (%) | Recurrent n (%) | No information, n (%) | Total |
| Person known by the victim* | 54 (48.6) | 51 (45.9) | 6 (5.4) | 111 |
| Intimate partner ** | 29 (55.8) | 22 (42.3) | 1 (1.9) | 52 |
| Officially married husband | - | 1 (100) | - | 1 |
| Traditionally married husband | - | 2 (100) | - | 2 |
| Father | - | 9 (81.8)*** | 2 (18.2) | 11 |
| Sibling | 6 (40) | 8 (53.3) | 1 (6.7) | 15 |
| Relative | 13 (50) | 13 (50) | - | 26 |
| Stranger | 10 (83.3)*** | 2 (16.7) | 0 | 12 |
| Stepfather | 1 (16.7) | 5 (83.3) | 0 | 6 |
| No knowledge | 6 (19.4) | 3 (9.7) | 22 (71) | 31 |
| Total | 117 (44.7) | 113 (43.1) | 32 (12.2) | 262 |
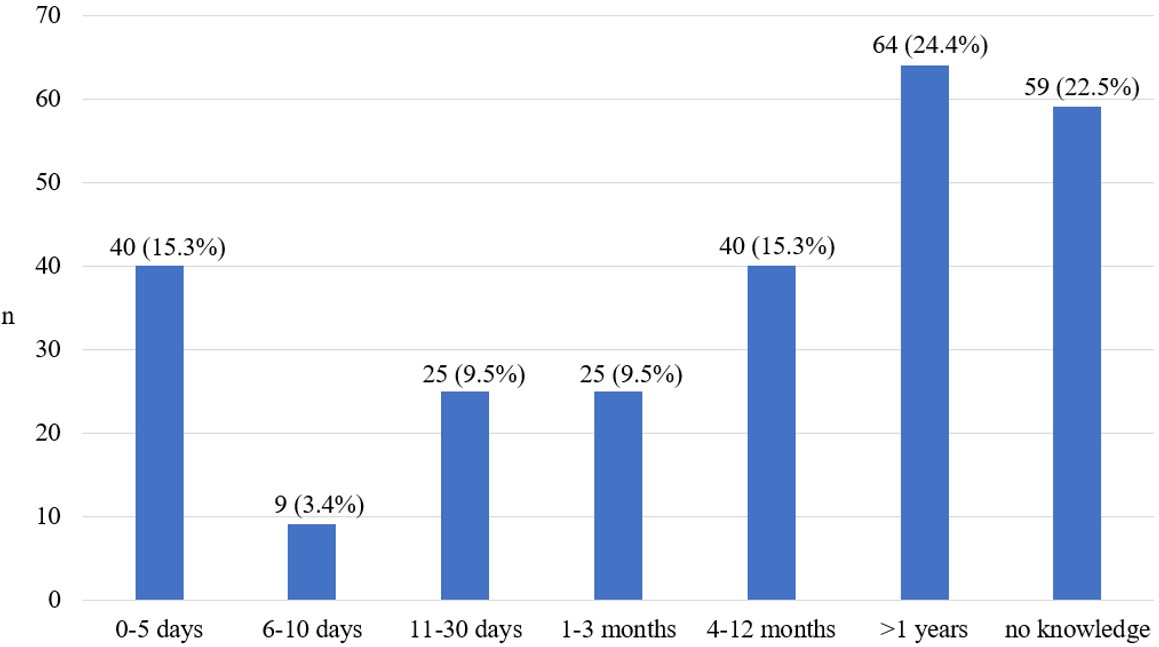
When the presentation times of the cases were analysed, it was observed that 49.2% (n=129) of the cases were presented more than 1 month later (Fig. 1).
When the relationship between intra-familial (father, sibling, husband, relative) and extra-familial (boyfriend, engaged, neighbor, friend, stranger) sexual abuse suspects and the duration of presentation of the cases was examined, it was found that 55.7% (n=34) of the intra-familial sexual abuse cases presented to health institutions for sexual abuse examination more than one year later and it was statistically significant (p<0.05, Table I).
In the histories obtained from the sexual abuse cases, it was observed that 20.2% (n=56) of the incidents occurred in the suspect’s home, 12.6% (n=35) in the homes of friends or acquaintances, 9.7% (n=27) in the joint home of the victim and the suspect, and 7.6% (n=21) in the victim’s home.
The type of alleged abuse was categorized into four groups vaginal penetration, anal penetration, oral penetration, and non-penetrative sexual abuse (touching, showing genital organs, watching videos, rubbing). It was found that 40.8% (n=107) of the cases had vaginal penetration and 32.4% (n=85) had anal penetration (Table II).
|
Percentages are given according to the number of cases. In some cases, there is more than one type of sexual abuse allegation. * One case with a history of anal penetration and two cases with a history of vaginal penetration did not accept the examination. ** Touching, showing genitals, showing videos, rubbing |
|
| Table II. Types of alleged abuse. | |
| n (%) | |
| Vaginal penetration* | 107 (40.8) |
| Anal penetration* | 85 (32.4) |
| Oral penetration | 9 (3.4) |
| Non-penetrative sexual abuse ** | 56 (21.4) |
| No knowledge | 38 (14.5) |
Vaginal examination findings
In our study, 195 cases who underwent vaginal examination were identified (Table III). When the cases were evaluated according to the presence or absence of vaginal penetration in the history, 59.04% (n=62) of 105 cases with a history of vaginal penetration had lacerations in the hymens (52 complete and incomplete healed lacerations, 10 acute lacerations). In 97% (n=65) of 67 patients without a history of vaginal penetration, there was no sign of injury to the hymen (Table III). 67.9% (n=36) of 53 cases with non-acute lacerations extending to the base of the hymen were below 3-9 o’clock, 15% (n=8) were at 3-9 o’clock, and 16.9% (n=9) were above 3-9 o’clock. All of the incomplete lacerations were below 3-9 o’clock.
|
Some cases have more than one finding. *p<0.05 |
|||||
| Table III. Relationship between vaginal penetration history and examination findings. | |||||
| History of vaginal penetration | Total | ||||
| Yes | No | No information | |||
| Hymen with no signs of injury | n | 43 | 65* | 21 | 129 |
| Row% | 33.3 | 50.4 | 16.3 | ||
| Column% | 41 | 97.0 | 91.3 | 66.2 | |
| Acute laceration | n | 10* | - | - | 10 |
| Row% | 100.0 | - | - | ||
| Column% | 9.5 | - | - | 5.1 | |
| Non-acute (healed) complete laceration | n | 50* | 1 | 2 | 53 |
| Row% | 94.3 | 1.9 | 3.8 | ||
| Column% | 47.6 | 1.5 | 8.7 | 27.2 | |
| Non-acute (healed incomplete laceration | n | 2 | - | - | 2 |
| Row% | 100.0 | - | - | ||
| Column% | 1.9 | - | - | 1 | |
| Ecchymosis, abrasion | n | 3 | 2 | - | 5 |
| Row% | 60.0 | 40.0 | - | ||
| Column% | 2.9 | 3.0 | - | 2.6 | |
| Total | n | 105 | 67 | 23 | 195 |
| % | 53.8 | 34.4 | 11.8 | 100.0 | |
Anal examination findings
It was observed that 75.8% (n=179) of 236 patients who underwent anal examination did not have anal sexual abuse findings (Table IV). When anal examination was analyzed according to the presence or absence of anal penetration history, it was found that 54.8% (n=46) of 84 cases with anal penetration history did not have any findings that could be related to sexual abuse (Table IV). The most common anal finding was ‘decreased sphincter tone’ seen in 10.6% (n=25) of the cases, followed by ‘ecchymosis/abrasion of anal mucosa’ seen in 7.2% (n=17) of the cases. While 57.1% (n=8) of 14 patients who had a history of anal penetration and underwent anogenital examination within the first 5 days, 42.3% (n=30) of 71 patients who presented more than 5 days later had findings.
|
Some cases have more than one finding. *p<0.05 |
|||||
| Table IV. The relationship between anal penetration history and examination findings. | |||||
| History of anal penetration | No knowledge | Total | |||
| Yes | No | ||||
| Decreased sphincter tone | n | 20* | 4 | 1 | 25 |
| Row% | 80.0 | 16.0 | 4.0 | ||
| Column% | 23.8 | 3.4 | 2.9 | 10.6 | |
| Ecchymosis, abrasion of anal mucosa | n | 12* | 3 | 2 | 17 |
| Row% | 70.6 | 17.6 | 11.8 | ||
| Column% | 14.3 | 2.5 | 5.9 | 7.2 | |
| Healed anal fissure | n | 9 | 5 | 1 | 15 |
| Row% | 60.0 | 33.3 | 6.7 | ||
| Column% | 10.7 | 4.2 | 2.9 | 6.4 | |
| Reflex anal dilatation | n | 12* | 3 | - | 15 |
| Row% | 80.0 | 20.0 | - | ||
| Column% | 14.3 | 2.5 | - | 6.4 | |
| Acute anal fissure | n | 8* | 2 | - | 10 |
| Row% | 80.0 | 20.0 | - | ||
| Column% | 9.5 | 1.7 | - | 4.2 | |
| Anal dilatation | n | 2 | - | 1 | 3 |
| Row% | 66.7 | - | 33.3 | ||
| Column% | 2.4 | - | 2.9 | 1.3 | |
| Erasure of pili | n | 3 | - | - | 3 |
| Row% | 100.0 | - | - | ||
| Column% | 3.6 | - | - | 1.3 | |
| No anal findings | n | 46 | 103* | 30 | 179 |
| Row% | 25.7 | 57.5 | 16.8 | ||
| Column% | 54.8 | 87.3 | 88.2 | 75.8 | |
| Total | n | 84 | 118 | 34 | 236 |
| % | 35.6 | 50.0 | 14.4 | 100 | |
Discussion
The prevention of CSA cases depends on the identification of risk factors and accurate diagnosis of CSA on examination. In this direction, we discussed the sociodemographic characteristics and anogenital examination findings of CSA cases in comparison with the findings in the literature.
It is reported that CSA is significantly more common in women and that women in childhood are 2 to 3 times more at risk of sexual abuse than men. In addition, in a WHO meta-analysis including 65 studies from 22 countries, the prevalence of CSA was reported to be 19.7% in females and 7.9% in males.17 In our study, 76.3% of the victims of sexual abuse were female, and this result is consistent with the literature.
It is estimated that the majority of children exposed to sexual abuse were between 12 and 17 years old at the time of the first abuse and that 32.8-63.8% of CSA victims were between 12-17 years of age at the time of the abuse.18-20 In our study, the most common age range of the cases who presented for sexual abuse examination was 12-17 years (77.5%). Studies show that sexual abuse is more common in children over the age of 12.19,20
Most CSA cases are performed by a male who knows the child. In various studies, the rate of CSA performed by a person who knows the children was found to be between 78% and 96%.21-24 In the present study, 95.5% of the victims stated that they were sexually abused by a person they knew.
Intra-familial abuse is notable in terms of its onset at a younger age, its continuity, and the delay and difficulties in reporting the abuse by the child.25 In the present study, when the mean ages of intra-familial and extra-familial CSA cases (12.59 ± 3.5 and 13.77 ± 2.9, respectively) were compared, it was found that intra-familial CSA victims were younger (U=4021.5, p<0.017) and 57.6% of intra-familial cases were reported more than one year after the abuse. In comparison, this rate was 16.9% in extra-familial cases (p<0.05). Magalhães et al.25 in their study comparing intra-familial and extra-familial CSA cases, reported that intra-familial CSA cases were more likely to be perpetrated at a younger age, usually at home, by abusers with more predominant emotional violence and with a history of sexual offenses; in addition, there was more time between the date of the last abuse and the forensic examination and physical findings were less likely to be detected.
There is a widespread consensus in the literature that children who are sexually abused delay disclosure significantly or do not disclose at all until adulthood, whereas children who are sexually abused intra-familial delay disclosure for a longer period.4,26-28 In the two surveys conducted, 47-59.5% of those who stated that they had been subjected to sexual abuse disclosed the abuse for the first time during the survey.29,30 In our study, in the majority of the cases (24.4%), it was observed that more than one year had elapsed between the application to forensic medicine and the onset of sexual abuse. Studies show that a significant number of CSA do not disclose their exposure until adulthood, and even a significant number of adults never disclose the abuse.4 Educating children who have been victims of sexual abuse and making them feel that they have a safe and supportive environment behind them will facilitate the disclosure of these cases and prevent their recurrence. In addition, late disclosure of sexual abuse may mean the disappearance of concrete findings that can be detected during examination in the anogenital area, which is known to heal quickly and without leaving scars.7,8,31
Recurrent CSAs are associated with comorbid illnesses, acute psychotic problems, suicide attempts, and low school achievement in children.2 In addition, a child who is a victim of sexual abuse is more likely to be sexually abused again.2 Studies report that 35.2-47.9% of sexual abuse victims are exposed to sexual abuse again.2,32 In addition, no relationship was found between recurrent sexual abuse and gender.32 In our study, similar to the literature, the rate of patients who stated that they had been subjected to recurrent sexual abuse was 43.1%, and it was not found to be related to gender (p=0.86). In addition, recurrent sexual abuse was found to be significantly higher in cases of intra-familial CSA. These findings support the idea that children who are subjected to intra-familial sexual abuse hesitate to disclose the abuses and experience recurrent victimization due to reasons such as fear for their safety, shame, self-blame, and loyalty to the perpetrator.33 These findings makes it imperative for the authorities to take social and legal measures to prevent this abuse from recurring.
In cases of CSA, examination findings are not obtained sufficiently and the fact that the abuse involves penetration does not mean that examination findings will be detected. The reason for this is considered to be delays in disclosing the abuse and the disappearance of physical injuries caused by abuse over time due to the rapid and almost complete regeneration ability of the anogenital region.6,9,14,34 In a study by Kellogg et al.13 in which CSA findings were evaluated, it was reported that examination findings were found in 14.2-85% of the studies in which acute cases were evaluated. In contrast, the rate of detection of findings was less than 12% in studies in which non-acute cases were evaluated. It has been reported that healing of the majority of the hymen tissue is possible except for deep lacerations, and genital trauma findings are found more rarely in non-acute cases.34,35 Anderst et al.36 found diagnostic examination findings in only 12.6% of the cases in a study consisting almost entirely of cases with a history of non-acute penetration. Gallion et al.35 did not find genital trauma in the examination of 79% of the penetration histories reported by children. In our study, no traumatic findings were found in the genital examination of 41% of the cases with a history of vaginal penetration and the majority of these cases (72.1%; 31 of 43 cases) presented more than 5 days later.
In our study, it was found that all of the cases with acute laceration of the hymen had a history of vaginal penetration, while 94.3% of the cases with healed laceration had a history of penetration, and it was statistically significant (p<0.05). In addition, there was no sign of injury to the hymen in 94% of the cases without a history of penetration (p<0.05). Similar to our study, Gallion et al.35 reported that 91% of the cases with findings on examination had a history of vaginal penetration, and the most common finding of sexual abuse was healed laceration (32% n=32) in the hymen. According to the literature, the location of non-acute lacerations in the hymen is essential in evaluating the findings.Non-acute laceration extending to the hymen base at the 3 and 9 o’clock positions, which was evaluated among the non-consensus findings in the 2023 update by Kellogg et al.13, was found in 8 cases in our study, and a history of vaginal penetration was obtained in 87.5%. The finding of non-acute laceration below the 3 and 9 o’clock position, which was evaluated among trauma-related findings, was found in 36 cases, and 94.4% (n=34) had a history of vaginal penetration. All 9 cases with non-acute lacerations above the 3 and 9 o’clock positions had a history of vaginal penetration. According to Kellogg et al.13 in the reports submitted to the forensic authorities in 9 cases in which non-acute laceration was found at 3-9 o’clock, which was considered as a variant of normal, it was reported that this finding could not be accepted as a finding of penetration alone because of the absence of acute examination findings and the abuse should be clarified by forensic investigation.
In studies conducted in the pediatric age group in which anogenital examination findings were compared in groups with and without anal penetration history, Myhre et al.37 found total dilatation in 12.1%, anal fissure in 10.7%, anal laceration in 4.6% of children with a history of highly suspected anal penetration and these findings were found to be associated with anal penetration (p=0.000). It has been reported that only external dilatation has a weaker association with soiling in the perianal region (p<0.05).37 In the study of Hobbs et al.38 reflex anal dilatation, anal tonus weakening, redness/erythema, perianal venous congestion, and anal fissure were found to be associated with anal penetration (p<0.001). However, in this study, the rate of those who were examined within the first 7 days after sexual abuse was higher (31.5%) compared to previous studies, and therefore, erythema finding was found to be more common compared to the literature, and venous congestion was also reported to be associated with anal penetration contrary to the literature. However, Kellogg et al.13 in the 2023 update of CSA findings, erythema and venous congestion were evaluated in the ‘Category B’ group (findings that may have more than one cause and are usually caused by medical conditions other than trauma or sexual contact). Another controversial finding, ‘complete anal dilatation,’ was evaluated in ‘category D’ (findings that were associated with a history of sexual abuse in some studies, but there was no consensus among experts about the degree of importance). It is reported that this finding may vary depending on the examination position.37 In our study, anal fissure, reflex anal dilatation, ecchymosis/abrasion in the anal area, decreased sphincter tone and flattening of the anal pleats were found to be associated with anal penetration, similar to the literature (Table IV).13,37,38
The most striking finding in our study was that 54.8% of the children with a history of anal penetration had no findings on anogenital examination. It is known that anal penetration may occur without causing any injury, or the injury may heal without leaving any scar.14-16 Hobbs et al.38 reported that 26% of children with a history of anal penetration had no findings on anal examination. Adams et al.39 did not find any findings in 56% of pediatric cases with a history of anal penetration. In addition, the detection of physical findings of sexual abuse becomes more complex as time passes since the incident. Smith et al.15 and Adams et al.39 reported that more physical findings were found in anogenital examinations performed in the first 72 hours. Studies also indicated more physical findings in examinations performed in the first 7 days.8,38 In our study, in cases with a history of anal penetration, 57.1% (n=8 of 14) of anal examinations performed within the first 5 days and 44.4% (n=24 of 54) of examinations performed after 5 days were positive.
According to the results obtained in our study, it was observed that CSA cases occurred mainly against a child of the female gender and between the ages of 12-17, by a stranger, in a closed place, most frequently in a house. Intra-familial sexual abuse cases, which start at a young age and are reported late or not reported at all, are in a particular position in the detection and prevention of CSA cases. In our study, findings of acute and healed laceration were found to be associated with the history of vaginal penetration, and findings of decreased sphincter tone, ecchymosis, abrasion, reflex anal dilatation, and acute anal fissure were found to be associated with the history of anal penetration. However, late reporting of CSA stands out as the most crucial factor covering the concrete findings of sexual abuse. It is imperative that efforts be made to facilitate the earlier disclosure of victims of CSA in this regard. Among the cases reported later than 5 days, 37.8% of the cases with a history of vaginal penetration and 53.7% of the cases with a history of anal penetration had no examination findings. It should be kept in mind that sexual abuse may occur without leaving any traumatic findings and the anogenital region may heal rapidly without leaving any findings. Preventing CSA will be possible by analyzing the risk factors and reaching the cases at risk as early as possible. However, the victims need to present in the acute period to prevent the loss of anogenital examination findings. Healthcare workers who encounter a case of CSA should notify the competent authorities as soon as possible and refer for an anogenital examination in order to prevent the disappearance of the findings.
Limitations
Although our study covers a large number of cases, the fact that the data were collected retrospectively from existing medical records can be considered a limitation. This methodology is subject to typical limitations associated with recorded patient information, including a high rate of unreported data and possible errors. Today, there is still a need to update CSA findings and, more structured multidisciplinary prospective studies focusing also on parental education, socioeconomic status, alcohol and drug addiction of victims and, psychiatric outcomes with a higher evidence level in larger populations in different regions of our country are needed.
Ethical approval
The study was approved by Pamukkale University Ethics Committee (date: 31.05.2023, number: E-60116787-020-374178).
Source of funding
The authors declare the study received no funding.
Conflict of interest
The authors declare that there is no conflict of interest.
References
- Johnson CF. Child sexual abuse. Lancet 2004; 364: 462-470. https://doi.org/10.1016/S0140-6736(04)16771-8
- Hu MH, Huang GS, Huang JL, et al. Clinical characteristic and risk factors of recurrent sexual abuse and delayed reported sexual abuse in childhood. Medicine (Baltimore) 2018; 97: e0236. https://doi.org/10.1097/MD.0000000000010236
- Banvard-Fox C, Linger M, Paulson DJ, Cottrell L, Davidov DM. Sexual assault in adolescents. Prim Care 2020; 47: 331-349. https://doi.org/10.1016/j.pop.2020.02.010
- McElvaney R. Disclosure of child sexual abuse: delays, non-disclosure and partial disclosure. What the research tells us and implications for practice. Child Abuse Rev 2015; 24: 159-169. https://doi.org/10.1002/car.2280
- Assink M, van der Put CE, Meeuwsen MWCM, et al. Risk factors for child sexual abuse victimization: a meta-analytic review. Psychol Bull 2019; 145: 459-489. https://doi.org/10.1037/bul0000188
- Herrmann B, Banaschak S, Csorba R, Navratil F, Dettmeyer R. Physical examination in child sexual abuse: approaches and current evidence. Dtsch Arztebl Int 2014; 111: 692–703. https://doi.org/10.3238/arztebl.2014.0692
- Heger A, Ticson L, Velasquez O, Bernier R. Children referred for possible sexual abuse: medical findings in 2384 children. Child Abuse Negl 2002; 26: 645-659. https://doi.org/10.1016/s0145-2134(02)00339-3
- Watkeys JM, Price LD, Upton PM, Maddocks A. The timing of medical examination following an allegation of sexual abuse: is this an emergency? Arch Dis Child 2008; 93: 851-856. https://doi.org/10.1136/adc.2007.123604
- Heppenstall-Heger A, McConnell G, Ticson L, Guerra L, Lister J, Zaragoza T. Healing patterns in anogenital injuries: a longitudinal study of injuries associated with sexual abuse, accidental injuries, or genital surgery in the preadolescent child. Pediatrics 2003; 112: 829-837. https://doi.org/10.1542/peds.112.4.829
- Adams JA. Medical evaluation of suspected child sexual abuse: 2011 update. J Child Sex Abus 2011; 20: 588-605. https://doi.org/10.1080/10538712.2011.606107
- Adams JA, Farst KJ, Kellogg ND. Interpretation of medical findings in suspected child sexual abuse: an update for 2018. J Pediatr Adolesc Gynecol 2018; 31: 225-231. https://doi.org/10.1016/j.jpag.2017.12.011
- Adams JA. Approach to the interpretation of medical and laboratory findings in suspected child sexual abuse: a 2005 revision. APSAC Advisor 2005; 17: 7-13.
- Kellogg ND, Farst KJ, Adams JA. Interpretation of medical findings in suspected child sexual abuse: an update for 2023. Child Abuse Negl 2023; 145: 106283. https://doi.org/10.1016/j.chiabu.2023.106283
- Berkowitz CD. Healing of genital injuries. J Child Sex Abus 2011; 20: 537-547. https://doi.org/10.1080/10538712.2011.607752
- Smith TD, Raman SR, Madigan S, Waldman J, Shouldice M. Anogenital findings in 3569 pediatric examinations for sexual abuse/assault. J Pediatr Adolesc Gynecol 2018; 31: 79-83. https://doi.org/10.1016/j.jpag.2017.10.006
- Pierce AM. Anal fissures and anal scars in anal abuse-are they significant? Pediatr Surg Int 2004; 20: 334-338. https://doi.org/10.1007/s00383-004-1193-8
- World Health Organization (WHO). Child maltreatment. 2024. Available at: https://www.who.int/news-room/fact-sheets/detail/child-maltreatment (Accessed on Feb 21, 2024).
- US Department of Justice; Office of Justice Programs; Bureau of Justice Statistics. Sexual assault of young children as reported to law enforcement: victim, incident, and offender characteristics. 2000. Available at: https://bjs.ojp.gov/library/publications/sexual-assault-young-children-reported-law-enforcement-victim-incident-and (Accessed on Feb 21, 2024).
- Davies EA, Jones AC. Risk factors in child sexual abuse. J Forensic Leg Med 2013; 20: 146-150. https://doi.org/10.1016/j.jflm.2012.06.005
- Whitelock CF, Lamb ME, Rentfrow PJ. Overcoming trauma: psychological and demographic characteristics of child sexual abuse survivors in adulthood. Clin Psychol Sci 2013; 1: 351-362. https://doi.org/10.1177/2167702613480136
- Hassan MA, Gary F, Killion C, Lewin L, Totten V. Patterns of sexual abuse among children: victims’ and perpetrators’ characteristics. J Aggress Maltreatment Trauma 2015; 24: 400-418. https://doi.org/10.1080/10926771.2015.1022289
- Yektaş Ç, Tufan A, Büken B, Çetin N, Yazıcı M. Evaluation of abuse and abuser’s features and risk factors associated with psychopathology in children and adolescents victimized by sexual abuse. Anatol J Psychiatry 2018; 19: 501-509. https://doi.org/10.5455/apd.291908
- Erdogan A, Tufan E, Karaman MG. Characteristic features of perpetrators of sexual abuse on children and adolescents in four different regions of Turkey. Anatol J Psychiatry 2011; 12: 55-61.
- Cengel-Kültür E, Cuhadaroğlu-Cetin F, Gökler B. Demographic and clinical features of child abuse and neglect cases. Turk J Pediatr 2007; 49: 256-262.
- Magalhães T, Taveira F, Jardim P, Santos L, Matos E, Santos A. Sexual abuse of children. A comparative study of intra and extra-familial cases. J Forensic Leg Med 2009; 16: 455-459. https://doi.org/10.1016/j.jflm.2009.05.007
- Goodman-Brown TB, Edelstein RS, Goodman GS, Jones DPH, Gordon DS. Why children tell: a model of children’s disclosure of sexual abuse. Child Abuse Negl 2003; 27: 525-540. https://doi.org/10.1016/s0145-2134(03)00037-1
- Hershkowitz I, Horowitz D, Lamb ME. Trends in children’s disclosure of abuse in Israel: a national study. Child Abuse Negl 2005; 29: 1203-1214. https://doi.org/10.1016/j.chiabu.2005.04.008
- Smith DW, Letourneau EJ, Saunders BE, Kilpatrick DG, Resnick HS, Best CL. Delay in disclosure of childhood rape: results from a national survey. Child Abuse Negl 2000; 24: 273-287. https://doi.org/10.1016/s0145-2134(99)00130-1
- Priebe G, Svedin CG. Child sexual abuse is largely hidden from the adult society. An epidemiological study of adolescents’ disclosures. Child Abuse Negl 2008; 32: 1095-1108. https://doi.org/10.1016/j.chiabu.2008.04.001
- Mc Gee H, Garavan R, de Barra M, Byrne J, Conroy R. The SAVI report: sexual abuse and violence in Ireland. Ireland: Royal College of Surgeons in Ireland; 2002. https://doi.org/10.25419/rcsi.10770797.v2
- Barth J, Bermetz L, Heim E, Trelle S, Tonia T. The current prevalence of child sexual abuse worldwide: a systematic review and meta-analysis. Int J Public Health 2013; 58: 469-483. https://doi.org/10.1007/s00038-012-0426-1
- Walker HE, Freud JS, Ellis RA, Fraine SM, Wilson LC. The Prevalence of sexual revictimization: a meta-analytic review. Trauma Violence Abuse 2019; 20: 67-80. https://doi.org/10.1177/1524838017692364
- Gekoski A, Davidson JC, Horvath MAH. The prevalence, nature, and impact of intrafamilial child sexual abuse: findings from a rapid evidence assessment. J Criminol Res Policy Pract 2016; 2: 231-243. https://doi.org/10.1108/JCRPP-05-2016-0008
- McCann J, Miyamoto S, Boyle C, Rogers K. Healing of hymenal injuries in prepubertal and adolescent girls: a descriptive study. Pediatrics 2007; 119: e1094-e1106. https://doi.org/10.1542/peds.2006-0964
- Gallion HR, Milam LJ, Littrell LL. Genital findings in cases of child sexual abuse: genital vs vaginal penetration. J Pediatr Adolesc Gynecol 2016; 29: 604-611. https://doi.org/10.1016/j.jpag.2016.05.001
- Anderst J, Kellogg N, Jung I. Reports of repetitive penile-genital penetration often have no definitive evidence of penetration. Pediatrics 2009; 124: e403-e409. https://doi.org/10.1542/peds.2008-3053
- Myhre AK, Adams JA, Kaufhold M, Davis JL, Suresh P, Kuelbs CL. Anal findings in children with and without probable anal penetration: a retrospective study of 1115 children referred for suspected sexual abuse. Child Abuse Negl 2013; 37: 465-474. https://doi.org/10.1016/j.chiabu.2013.03.011
- Hobbs CJ, Wright CM. Anal signs of child sexual abuse: a case-control study. BMC Pediatr 2014; 14: 128. https://doi.org/10.1186/1471-2431-14-128
- Adams JA, Harper K, Knudson S, Revilla J. Examination findings in legally confirmed child sexual abuse: it’s normal to be normal. Pediatrics 1994; 94: 310-317.
Copyright and license
Copyright © 2025 The Author(s). This is an open access article distributed under the Creative Commons Attribution License (CC BY), which permits unrestricted use, distribution, and reproduction in any medium or format, provided the original work is properly cited.