Graphical Abstract
Abstract
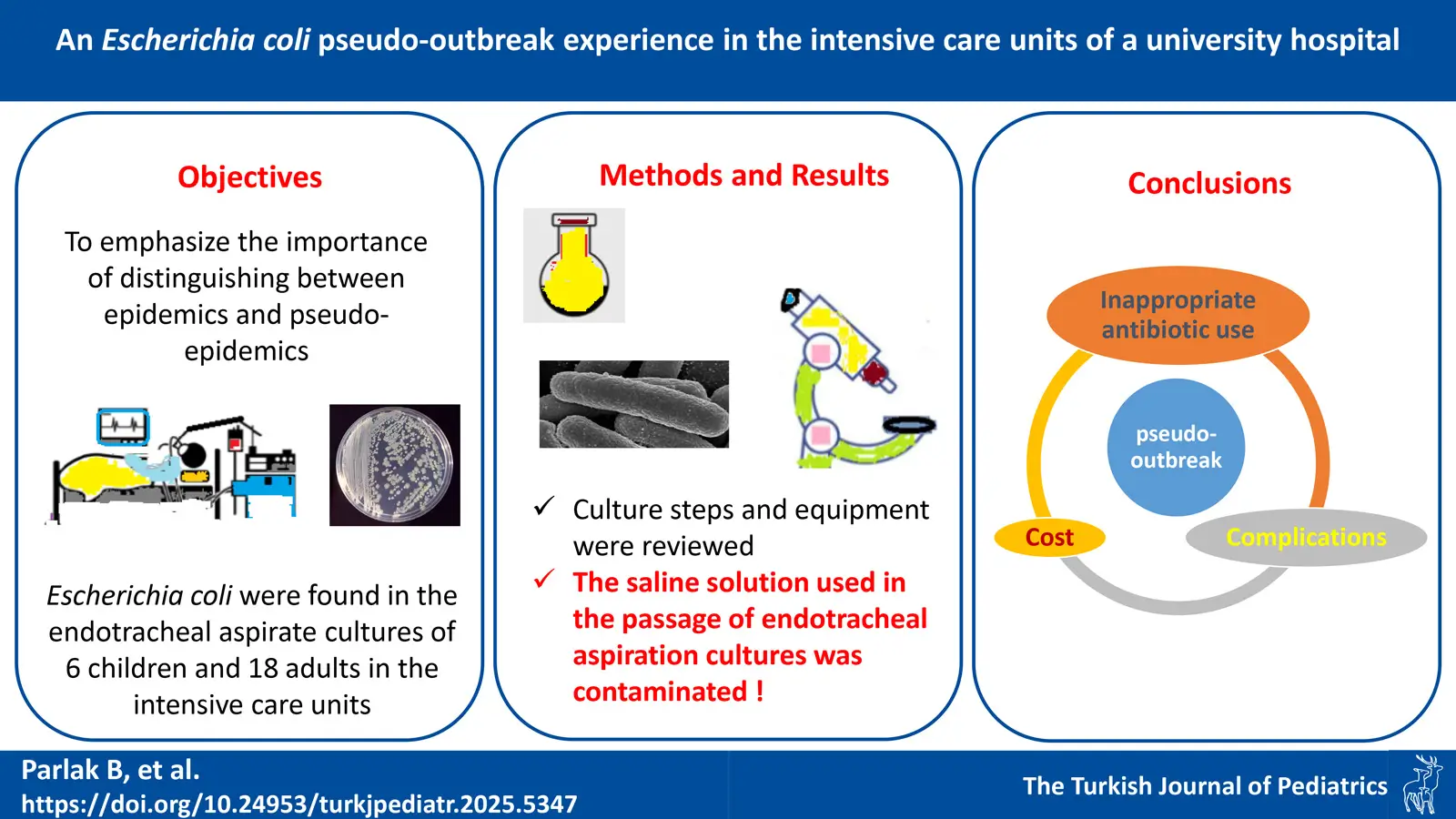
Background. The term ‘pseudo-outbreak’ refers to a condition in which a microorganism is found in cultures at a greater rate than expected due to contamination of materials that would normally be sterile. This situation cannot be clinically correlated with the infection suggested by the culture results. This can be confusing depending on the patient’s clinical condition, especially in intensive care units (ICU). The pseudo-outbreak with Escherichia coli in patients in ICUs will be discussed in this study to emphasize the importance of strict adherence to microbiology policies and procedures.
Methods. In September 2022, growths of Escherichia coli were found in the endotracheal aspirate cultures of six children and eighteen adults in the ICU.
Results. The identification of the same microbial agent in 24 patients prompted an investigation into a potential outbreak. The infection control committee compiled a comprehensive patient list to facilitate the assessment. Given that the healthcare personnel and infrastructure of each ICU were distinct and functioned independently, the possibility of cross-contamination within these units was deemed unlikely. Consequently, attention was directed toward the microbiology laboratory as a potential source of the outbreak. A thorough review of culture processing steps and laboratory equipment was conducted. This investigation revealed that the saline solution used for the passage of endotracheal aspiration cultures was contaminated, suggesting a laboratory-associated contamination event as the probable cause.
Conclusions. By strictly adhering to the latest protocols, the disinfection and sterilization chain can ensure the safe use of both invasive and non-invasive medical equipment. This manuscript aims to raise awareness among pediatricians and pediatric infectious disease specialists regarding the occurrence of pseudo-outbreaks. A pseudo-outbreak is indicative of a disruption in the sterilization chain.
Keywords: pseudo-outbreak, Escherichia coli, contamination
Introduction
An increase in hospital infections, typically from a single species, that is mistakenly interpreted as a true epidemic is known as a pseudo-epidemic of nosocomial infections, and they can be very challenging to identify.1
Infectious diseases that spread rapidly within a community are central to most dictionary definitions of an ‘outbreak.2 An outbreak is defined as occurring when the number of reported cases exceeds the expected number for a specific time frame and the cases are connected by epidemiological or microbiological characteristics.3 However, two or more epidemiologically linked cases with outbreak potential, or even a single case of a newly emerging or previously eradicated disease, can also be considered an outbreak.4 In some diseases, such as smallpox and poliomyelitis due to wild poliovirus, even a single case is considered an outbreak.4 The term ‘pseudo-outbreak’ refers to a situation in which a microorganism is detected in cultures at a higher rate than expected and that cannot be clinical correlated with the infection suggested by the culture results due to contamination of materials that would normally be sterile.5 ICU’s, transplant units, oncology, and endoscopy units are areas that have risks for both outbreaks and pseudo-outbreaks.6,7Potential sources of bacterial contamination include bulk diluents, saline bottles, patient beds, ventilators, switches, door handles, sinks, blood collection tubes, liquid hand soaps, soap dispensers, disinfectants, in solutions with nutrients, anesthetics and, laboratory personnel.8 Contamination and pseudo-outbreaks result in wasted time, and labor and can also invalidate experiments. Early detection of a pseudo-outbreak significantly reduces inappropriate antibiotic use, associated complications, healthcare and laboratory costs, mortality, and hospitalizations.6-8 Therefore, distinguishing between true outbreaks and pseudo-outbreaks at an early stage is crucial to mitigating these negative consequences.6
The first and most important step in combating any infectious disease is prompt identification and recognition of the condition. The importance of a hospital surveillance system that enables rapid and extensive information sharing as well as opinion sharing, and collaborative risk assessment and management, is emphasized. The key elements of a first hospital response include isolation protocols, laboratory capability, and case identification. Sample collection, transportation, and management procedures adhere to protocols established by the World Health Organization and The Centers for Disease Control and Prevention.3 Healthcare environments need to be an environment where people can report errors without fear of condemnation or punishment.8 All healthcare personnel involved in patient care should be aware of and receive training in infection control.8
Healthcare institutions should actively review processes in high-risk areas to identify potential sources of contamination. It is imperative to designate experts to oversee infection prevention and control at the facility and subsequent administrative levels in order to facilitate a programmatic approach that prioritizes responsibility, supervision, and coordination through ongoing monitoring and assessment. The advent of numerous newly identified or unique infectious agents as well as the reappearance of infectious illnesses that affect the entire world have been the hallmarks of the past few decades. This study aims to provide an overview of the hospital response framework for the early detection and timely treatment of patients with infectious illnesses. The fundamental components of hospital preparedness in the event of a cluster of infectious diseases are discussed. Additionally, the study seeks to determine whether an observed increase in cases represents a true outbreak or a pseudo-outbreak and outlines the necessary steps for appropriate intervention.
Materials and Methods
The list of patients with Escherichia coli growth in endotracheal aspirate (ETA) cultures from September 2022 was obtained from the Infection Control Committee of Marmara University Pendik Training and Research Hospital. Escherichia coli growth was observed in the ETA cultures of 18 adult patients in the ICU and 6 pediatric patients in the pediatric ICU (PICU) in September 2022. The adult patients were hospitalized in the Anesthesia and Reanimation ICU, Internal Medicine ICU, General ICU, Cardiovascular Surgery ICU, and Organ Transplantation ICU
Results
Pediatric patients are presented in Table I. A 3.5-year-old boy with pneumonia, a 6-month-old boy with acute respiratory distress syndrome (ARDS), a 6.5-year-old girl diagnosed with a craniocervical mass who had a surgical wound infection, an 8-month-old girl with bronchopulmonary dysplasia and respiratory failure, a 2.5-month-old girl with diarrhea, a 3-year-old boy with aspiration pneumonia, pleural effusion and pneumothorax and a 3.9 month old male with a thorax tube, a Glasgow coma score of seven, fever, and hypotension were admitted to the PICU.
|
*Tracheostomized patients. ARDS, acute respiratory distress syndrome; ETA, endotracheal aspirate. |
||||
| Table I. Characteristics of patients in the pediatric intensive care unit. | ||||
| Case | Age (month) | Sex | Primary diagnosis | Timing of bacterial growth in ETA culture (days post-intubation) |
| 1 | 42 | Male | Pneumonia | 13* |
| 2 | 6 | Male | ARDS | 9 |
| 3 | 78 | Female | Craniocervical mass, wound infection | 13 |
| 4 | 8 | Female | Bronchopulmonary dysplasia and respiratory failure | 1 |
| 5 | 2.5 | Female | Diarrhea | 1 |
| 6 | 35 | Male | Aspiration pneumonia, empyema and pneumothorax | 1* |
Escherichia coli was isolated from the ETA cultures of 24 patients across all intensive care units (ICUs). The interpretation of these findings was challenging, as some patients exhibited clinical signs suggestive of pneumonia, including increased respiratory secretions, respiratory acidosis, and an elevated requirement for ventilator support. Due to institutional limitations, bacterial sequencing could not be performed; however, antibiogram results were identical across all cases, raising concerns regarding potential contamination or a pseudo-outbreak.. In other words, bacterial susceptibility and resistance were the same in all isolates. This isolate was determined to be sensitive to penicillins, aminoglycosides, and sulfonamides, and moderately sensitive to cephalosporins. Therefore, it was thought to be the same strain. Different staff members and different units were providing treatment for the patients. Additionally, on the day of their ICU admission, three patients had positive cultures (Table I). These results implied that the infection originated outside of the ICUs and at a common place like laboratory.
Upon observing an unusually high frequency of isolations of the same microorganism, with bacteria exhibiting identical susceptibility profiles across multiple ICUs within a single week, the Hospital Infection Control Committee was notified. It was determined that the Hospital Infection Control Committee had also identified the situation, prompting the initiation of an outbreak investigation. A comprehensive patient list was compiled. Given that the affected patients were located in different ICUs throughout the hospital, under the care of distinct medical teams, and not in direct proximity to one another, the investigation shifted focus to the microbiology laboratory—the common point connecting these disparate units. It was determined that a 250 mL bag of 0.9% sodium chloride (normal saline), used for the passage of cultures, had been accessed with a syringe multiple times over a period of 5–6 days, leading to contamination of the saline. To confirm this hypothesis, a sample from the saline bag was cultured, and the same bacterial strain was identified. The recognition of the pseudo-outbreak took approximately two weeks.
To address this issue, the saline bag was replaced with single-use 10 mL disposable physiological serum, which is now used for a maximum of 5–6 patients before being discarded. Additionally, disposable syringes are now utilized to prevent contamination.
The laboratory manager, infection prevention specialists, and relevant personnel conducted a comprehensive process assessment, developed improvement action plans, and provided retraining on established policies and procedures. Furthermore, emphasis was placed on reinforcing fundamental infection prevention and control measures, including proper hand hygiene, thorough cleaning and disinfection of workstations, and sanitation of commonly handled objects and surfaces.
Discussion
In critical care settings where rapid clinical decision-making is essential, such as ICUs and transplantation units, or in conditions requiring early intervention, such as sepsis, this situation can be particularly challenging. It may lead to diagnostic confusion, unnecessary distractions, and adverse effects associated with unwarranted treatment. In this study, a pseudo-outbreak of E. coli occurred due to contamination of the saline water used for passage of ETA cultures in the laboratory. Similarly, Mumcuoglu et al.5 isolated S. marcescens strains from blood cultures of 22 patients in two different ICUs. The Hospital Infection Control Committee conducted an environmental investigation and identified the surfaces of blood collection tubes as the source of contamination.5 Since the patients exhibited no clinical signs or symptoms consistent with infection, it was easier to determine that this was a pseudo-outbreak.5 Eldridge et al.8 during the investigation of a B. cepacia pseudo-outbreak, found that laboratory personnel caused cross-contamination through the use of non-sterile saline diluent. The susceptibility patterns of all isolates were found to be the same as in this study.8 The laboratory environment can act as potential sources of contamination, highlighting the need for regular surveillance and training in microbiology laboratories.8
Pseudo-outbreaks with many different organisms have been reported in the literature. Pseudo-outbreak can occur not only with bacteria but also with viruses. Hellinger et al.9 published their work about an adenovirus pseudo-outbreak in the bronchoalveolar lavage (BAL) specimens of seven ICUs patients due to adenovirus DNA on the bronchoscope. In the same month, specimens were taken from all patients and healthcare workers with nasopharyngeal swabs in the ICUs. The bronchoscope lumens were scanned. Inactive adenoviral DNA was detected only in the index case and in the bronchoscope. Adenovirus did not grow in the culture. Sterilization of bronchoscopes with ethylene oxide eliminated the contamination. A previous study reported an unusual finding in which 22 healthcare workers tested positive despite wearing masks due to the COVID-19 pandemic.10 Flipse et al.10 later described a pseudo-outbreak of Bordetella parapertussis, which was traced to swabs contaminated with B. parapertussis DNA. The investigation revealed that the contamination resulted from a manufacturing defect in the swabs, highlighting the potential for diagnostic errors due to faulty laboratory supplies. Additional invasive diagnostic procedures, time and cost may be required to confirm the diagnosis.
Stern et al.11 presented a study about a Rhizobium pseudo-outbreak. Rhizobium was isolated from six surgical tissue cultures and was determined to be due to improper laboratory tissue handling with contaminated saline. Non-sterile saline has been associated with pseudo-outbreaks of pathogens such as Burkholderia cepacia, Rhizobium, Legionella, etc. In the present study, it was related to E. coli. Nagano et al.12 described a pseudo-outbreak of Mycobacterium lentiflavum in their study. Sputum and BAL were both contaminated due to the use of tap water, and in environmental research they had found that tap water was passed through the bronchoscope before each procedure.12 In the latter study, the issue was identified only after three years, leading to the administration of multiple antibiotics to some patients. This resulted in unnecessary antibiotic use, potentially contributing to antimicrobial resistance, adverse effects, and increased healthcare costs. In contrast, in the current study, the issue was detected at an early stage, allowing for timely intervention.
A follow-up period of either one or two months should be carried out, at the very least, to avoid false-positive cultures in lab settings. Continuous communication among clinicians, laboratory technicians, and the Infection Control Committee is essential in interpreting unusual findings resulting from contamination. A pseudo-outbreak of Bacillaceae spp. bloodstream infection resulting from improper use of medical cotton wool during blood culture collection was described in the study by Borcan et al.13
Over a five-month period, Bacillaceae spp.-positive blood cultures were obtained from 60 patients, with two patients receiving treatment. Control measures included the removal of cotton wool contaminated with Bacillaceae spp. and the implementation of periodic training on proper blood culture collection techniques.13
The study had some limitations. For example, DNA sequencing was not performed to confirm whether the E. coli isolates were from the same strain.
In healthcare settings, distinguishing between outbreaks and pseudo-outbreaks can be challenging. Even when utilizing gold-standard diagnostic methods such as cultures, laboratory results should not replace clinical evaluation; physical examination findings must be considered in differentiating a true outbreak from a pseudo-outbreak.
Laboratory processing errors, such as deviating from standard disposable sterile transport media to a larger, contaminated saline distribution source or using non-sterile syringes, have been linked to pseudo-outbreaks. Effective infection control requires timely collaboration and communication, particularly in the prevention of pseudo-outbreaks.
This article highlights potential weaknesses in infection control protocols and provides practical recommendations for improving the standard of care and patient safety in healthcare settings. Identifying the source of an outbreak as early as possible is crucial, along with investigating discrepancies in infection control measures and microbiological processing protocols.
Source of funding
The authors declare the study received no funding.
Conflict of interest
The authors declare that there is no conflict of interest.
References
- Fan X, Dai RC, Kudinha T, Gu L. A pseudo-outbreak of Cyberlindnera fabianii funguria: implication from whole genome sequencing assay. Front Cell Infect Microbiol 2023; 13: 1130645. https://doi.org/10.3389/fcimb.2023.1130645
- Metcalfe S. History lessons. Aust Fam Physician 2013; 42: 519.
- Petrosillo N, Puro V, Di Caro A, Ippolito G. The initial hospital response to an epidemic. Arch Med Res 2005; 36: 706-712. https://doi.org/10.1016/j.arcmed.2005.05.003
- Republic of Türkiye Ministry of Health, General Directorate of Public Health. Guide to prevent infectious diseases. 2017. Available at: https://hsgm.saglik.gov.tr/depo/birimler/bulasici-hastaliklar-ve-erken-uyari-db/Birimler/Saha_Epidemiyolojisi_ve_Erken_Uyari/Bulasici_Hastaliklar_ile_Mucadele_Rehberi_Ustyazi.pdf (Accessed on September 29, 2024).
- Mumcuoglu I, Kanyilmaz D, Yetkin MA, et al. Serratia marcescens bacteremia cases: a pseudo-outbreak experience. Am J Infect Control 2016; 44: 852-853. https://doi.org/10.1016/j.ajic.2016.01.029
- Sood G, Perl TM. Outbreaks in health care settings. Infect Dis Clin North Am 2021; 35: 631-666. https://doi.org/10.1016/j.idc.2021.04.006
- Rutala WA, Weber DJ. Guideline for disinfection and sterilization in healthcare facilities. 2008 [updated May 2019]. Available at: https://www.cdc.gov/infection-control/media/pdfs/Guideline-Disinfection-H.pdf (Accessed on September 29, 2024).
- Eldridge CC, Flinchum AH, Thoroughman D, Spicer KB. A pseudo-outbreak of Burkholderia cepacia complex in a Kentucky hospital. Am J Infect Control 2022; 50: 342-344. https://doi.org/10.1016/j.ajic.2021.10.028
- Hellinger WC, Parth HC, Smith BT, et al. Adenovirus pseudo-outbreak associated with bronchoscopy. Infect Control Hosp Epidemiol 2019; 40: 1305-1308. https://doi.org/10.1017/ice.2019.235
- Flipse J, Tromp AT, Bosman J, et al. Pseudo-outbreak of Bordetella parapertussis caused by contaminated swabs in the Netherlands. Emerg Infect Dis 2022; 28: 890-892. https://doi.org/10.3201/eid2804.212097
- Stern RA, Byrge KC, Talbot TR. Rhizobium radiobacter pseudo-outbreak linked to tissue-processing contamination. Antimicrob Steward Healthc Epidemiol 2023; 3: e178. https://doi.org/10.1017/ash.2023.456
- Nagano Y, Kuronuma K, Kitamura Y, et al. Pseudo-outbreak of Mycobacterium lentiflavum at a general hospital in Japan. Infect Control Hosp Epidemiol 2023; 44: 1809-1815. https://doi.org/10.1017/ice.2023.68
- Borcan AM, Vasile CC, Popa AI, Badea CA, Popescu GA, Tălăpan D. Pseudo-outbreak of Bacillaceae species associated with poor compliance with blood culture collection recommendations. Eur J Clin Microbiol Infect Dis 2024; 43: 2335-2340. https://doi.org/10.1007/s10096-024-04925-5
Copyright and license
Copyright © 2025 The Author(s). This is an open access article distributed under the Creative Commons Attribution License (CC BY), which permits unrestricted use, distribution, and reproduction in any medium or format, provided the original work is properly cited.