Abstract
Background. The prevalence of acute suppurative appendicitis (ASA) is the highest among pediatric cases of acute abdominal conditions. This research examined the stress response linked to surgical techniques and identified potential biomarkers that could predict postoperative complications to enhance clinical treatment strategies.
Methods. This study involved a selection of 166 ASA patients who underwent laparoscopic appendectomy (LA), and 150 patients who underwent open appendectomy (OA), based on data collected from 2020 to 2023. Comprehensive documentation of clinical and pathological characteristics, as well as postoperative complications, was conducted following patient enrollment. Quantitative polymerase chain reaction (qPCR), enzyme-linked immunosorbent assay (ELISA), and blood smear techniques were employed to assess the levels of microRNA (miR)-155-5p, C-reactive protein (CRP), interleukin-6 (IL-6), tumor necrosis factor-α (TNF-α), superoxide dismutase (SOD), and malondialdehyde (MDA), as well as changes in leukocytes, neutrophils, and lymphocytes at preoperative and postoperative 0 h, and 24 h. A logistic regression model was utilized to identify risk factors associated with the development of complications. Furthermore, receiver operating characteristic (ROC) curve analysis was performed to assess the predictive capacity of miR-155-5p for the occurrence of complications.
Results. The study revealed that the levels of miR-155-5p postoperatively in patients undergoing OA was significantly greater than that observed in patients undergoing LA (P<0.001). The expression levels of miR-155-5p exhibited a significant positive correlation with inflammatory markers (CRP, r=0.546; IL-6, r=0.628; TNF-α, r=0.808; leukocytes, r=0.778; neutrophils, r=0.718; and lymphocytes, r=0.820), indicators of oxidative stress (SOD, r=0.671; and MDA, r=0.489), and visual analog scale (VAS, r=0.671) scores (P<0.001). Furthermore, miR-155-5p might influence the concentrations of inflammatory and oxidative stress markers in the serum of patients both preoperatively and postoperatively (P<0.05). Notably, miR-155-5p was identified as risk factors for the development of postoperative complications (OR=8.331, P=0.008) and had a high predictive value for the occurrence of postoperative complications (area under the curve=0.926, P<0.001).
Conclusion. miR-155-5p might play a role in modulating the body’s stress response, subsequently impacting the postoperative complications incidence of ASA patients.
Keywords: acute suppurative appendicitis, laparoscopic appendectomy, open appendectomy, miRNA, complication
Introduction
Acute suppurative appendicitis (ASA) in children represents the most prevalent acute abdominal condition among children in China.1 The disease is characterized by atypical clinical presentations, rapid progression, and severe manifestations.2 Open appendectomy (OA) remains a conventional treatment approach for ASA in pediatric patients; however, this surgical method is associated with considerable physical trauma, excessive intraoperative bleeding, and prolonged recovery periods.3 In light of advancements in laparoscopic and minimally invasive surgical techniques, laparoscopic appendectomy (LA) is gaining traction due to its advantages, including smaller incisions, enhanced safety, and expedited postoperative recovery.4 Nonetheless, postoperative complications following ASA in children are not infrequent.5 Consequently, the pursuit of specific biomarkers capable of predicting the occurrence of complications is essential for facilitating timely management, thus reducing the risk of postoperative complications.
MicroRNA (miRNA, miR) represents a class of multifunctional non-coding RNA.6 It is estimated that over 30% of human genes are modulated by miRNAs.7 Recent investigations have identified miRNA as a pivotal component in the mechanisms of oxidative stress and inflammatory responses across a range of diseases.8,9 Previous research has demonstrated that miR-155-5p is instrumental in macrophage polarization and plays a critical role in the regulation of inflammatory responses.10 miR-155-5p exhibits diverse functions and is implicated in numerous biological processes.11 For instance, in individuals with rheumatoid arthritis, elevated levels of miR-155-5p can trigger the expression of inflammatory mediators, and serve as a crucial predictor of disease onset.12 Furthermore, increased expression of miR-155-5p in the serum of patients with sepsis and tuberculosis has been identified as a diagnostic, prognostic, and predictive infection occurrence biomarker.13,14 Given the broad applicability of gene function, it is speculated that miR-155-5p may also contribute to the promotion of pediatric ASA. However, there is a paucity of research regarding miR-155-5p in this disease.
This study focuses on miR-155-5p as the primary subject of investigation to assess its expression variations and its association with clinical pathological characteristics in pediatric patients diagnosed with ASA who are undergoing either OA or LA. The study examines the relationship between the incidence of postoperative complications and various clinical parameters, aiming to identify independent factors that may influence the risk of postoperative infections. Ultimately, the study seeks to elucidate the predictive value of miR-155-5p concerning postoperative complications.
Materials and Methods
Study participants
A total of 316 pediatric patients who were diagnosed with ASA and underwent surgical intervention at Xingtai People’s Hospital between 2020 and 2023 were selected for this study. Among these patients, 150 underwent OA, while 166 underwent LA. A comparative analysis was conducted between the two patient groups. The inclusion criteria for this study were as follows: (a) patients aged 14 years or younger; (b) patients diagnosed with ASA and fulfill the criteria for surgical intervention; (c) patients possessing clear consciousness, with consent from both themselves and their guardians to participate in the study, and completion of the informed consent form; and (d) ability to cooperate in completing the visual analog scale (VAS) assessment.
The exclusion criteria included: (a) complicated cases, such as necrosis or perforation; (b) occurrence of concurrent infections in other body regions post-surgery; (c) pre-existing infections prior to surgery or inflammatory disease in the patient’s history; (d) patients with congenital conditions such as congenital heart disease or trisomy 21; (e) individuals with blood, immune system, or neurological disorders; and (f) patients exhibiting severe liver and kidney dysfunction or malignant tumors.
Preoperative clinical baseline characteristics were collected for all patients, encompassing age, gender, and course of the disease. Perioperative data such as duration of surgery, anal exhaust time, and length of stay, as well as status of complications were recorded. The total intraoperative blood loss is measured by subtracting the total weight of gauze from the combined weight of gauze with blood and adding the volume of blood in the suction bottle. A VAS score was used to assess the level of pain in the children preoperatively and postoperatively. The score of which ranged between 0–10, with higher scores indicating more severe pain. The final VAS score was assessed by the patient in conjunction with two medical workers, and the mean value was subsequently calculated to exclude evaluation bias. This study received approval from the Ethics Committee of Xingtai People’s Hospital and adhered strictly to the principles outlined in the Helsinki Declaration.
Serum collection
2.5-3.5 mL of peripheral venous blood was obtained from participants at three time points: prior to surgery (following the patient’s admission and enrollment in the study), immediately post-surgery, and 24 hours post-surgery. The samples were subjected to centrifugation using a low-temperature ultracentrifuge. Subsequently, the supernatant serum was preserved in a -80 °C freezer for subsequent analysis.
RNA extraction and complementary DNA synthesis
The RNAeasy™ Blood RNA Isolation Kit with Spin Column (Beyotime, China) was employed to extract total RNA. The purity and concentration of the extracted RNA was assessed using a NanoDrop 2000 spectrophotometer (Thermo Fisher Scientific, USA). A total of 1 μg of the extracted RNA was utilized as a template for the synthesis of the first strand of complementary DNA (cDNA) using the BeyRT™ III First Strand cDNA Synthesis Kit (Beyond, China).
Quantitative polymerase chain reaction (qPCR)
The HRbio™ miRNA qPCR gene expression detection kit (HeRui, China) was employed to assess the expression levels of miR-155-5p. The primer sequences (5’-3’) utilized for miR-155-5p were as follows: GCGGCTCCTACTATTAGATTAAC (forward) and CAGTGCAGGGTCCGAGGTAT (reverse). Detection was performed using a LightCycler 480 real-time fluorescence qPCR instrument (Roche Applied Science, Switzerland). The primers were synthesized by Genscript Biotechnology Co., Ltd. in Nanjing, China.
Enzyme-linked immunosorbent assay (ELISA) and blood smear
The human interleukin-6 (IL-6) and tumor necrosis factor-α (TNF-α) detection kits were from Nanjing Jiancheng Bioengineering Institute, the human C-reactive protein (CRP) detection kit from Wuhan Yunclonal Technology Co., Ltd., and the human malondialdehyde (MDA) and superoxide dismutase (SOD) detection kits from Shanghai Coibo Biotechnology Co., Ltd. Following the cessation of color development, the blank well was calibrated to zero, and the optical density (OD) value was measured using an ELISA reader at a wavelength of 450 nm, with each well being measured in triplicate.
Additionally, leukocyte, neutrophil, and lymphocyte counts were performed using the blood smear method. A drop of blood from the patient was placed on a glass slide, which was then tilted at a 45° angle to ensure an even distribution of the specimen across the slide. After allowing the slide to air dry, Wright’s staining was applied. The staining solution was allowed to cover the blood film completely and was left to stand for 5 min. Subsequently, a phosphate buffer solution was added, and the slide was maintained for 10 min. The slide was then rinsed with sterile double-distilled water, air-dried, and examined under a microscope. Each field of view was counted in triplicate to ensure accuracy.
Statistical analysis
This research employed SPSS 23.0 and GraphPad Prism 9.0 for the statistical analysis. Measurement data were presented as mean ± standard deviation (SD), with independent sample t-tests utilized for between group comparisons. Categorical data were expressed as percentages (%), and chi-square tests were applied for group comparisons. The comparison of VAS scores, serum miR-155-5p expression levels, levels of inflammatory factors, and oxidative stress indices between the laparotomy and laparoscopy groups at specific time points, and comparisons across different time points within the laparotomy and laparoscopy groups were performed using two-way analysis of variance. The correlation between preoperative miR-155-5p expression levels and various indicators measured 24 h post-surgery was assessed using Pearson correlation analysis. Independent sample t-tests and chi-square tests were employed to examine the relationship between it and preoperative clinical and pathological characteristics. Multiple logistic regression analysis was utilized to identify risk factors for postoperative complications, calculating the odds ratio (OR) and corresponding 95% confidence interval (CI) for each factor. The predictive efficacy of miR-155-5p for postoperative complications was evaluated through receiver operating characteristic (ROC) curves, with specificity and sensitivity of the detection indicators calculated.
Results
General characteristics of the study groups
The analysis revealed no statistically significant differences in terms of age distribution, gender ratio, and course of the disease between the two groups (P>0.05). However, the laparoscopy group exhibited significantly reduced duration of surgery, intraoperative bleeding, anal exhaust time, and length of stay when compared to the laparotomy group (P<0.001, Table I).
| P<0.05 indicates a significant difference. Data are presented as mean ± standard deviation, except for gender. | |||
| Table I. Participant characteristics. | |||
| Factors | Laparotomy group (n=150) | Laparoscopy group (n=166) | P value |
| Age, years | 8.12 ± 3.31 | 8.18 ± 3.36 | 0.872 |
| Gender, n (%) | 0.404 | ||
| Male | 73 (48.67%) | 73 (43.98%) | |
| Female | 77 (51.33%) | 93 (56.02%) | |
| Course of the disease, days | 1.20 ± 0.61 | 1.27 ± 0.69 | 0.367 |
| Duration of surgery, min | 62.36 ± 7.21 | 48.89 ± 7.17 | <0.001 |
| Intraoperative bleeding, mL | 27.01 ± 3.51 | 11.78 ± 3.35 | <0.001 |
| Anal exhaust time, hours | 3.79 ± 0.66 | 2.45 ± 0.72 | <0.001 |
| Length of stay, days | 8.59 ± 2.65 | 6.91 ± 2.60 | <0.001 |
Relative expression levels of miR-155-5p and VAS score
The results of the qPCR analysis indicated that there was no statistically significant difference in the expression levels of miR-155-5p in preoperative serum between the laparotomy and laparoscopy groups (P>0.05). The postoperative expression levels of miR-155-5p in the serum of the laparoscopy group were found to be significantly lower than those in the laparotomy group (P<0.001, Fig. 1A). Notably, the expression levels of miR-155-5p in the serum of patients in both groups exhibited a significant increase immediately following surgery (P<0.001), followed by a significant decrease 24 h post-surgery (P<0.001), although these levels remained significantly elevated compared to preoperative values (P<0.01, Fig. 1A).
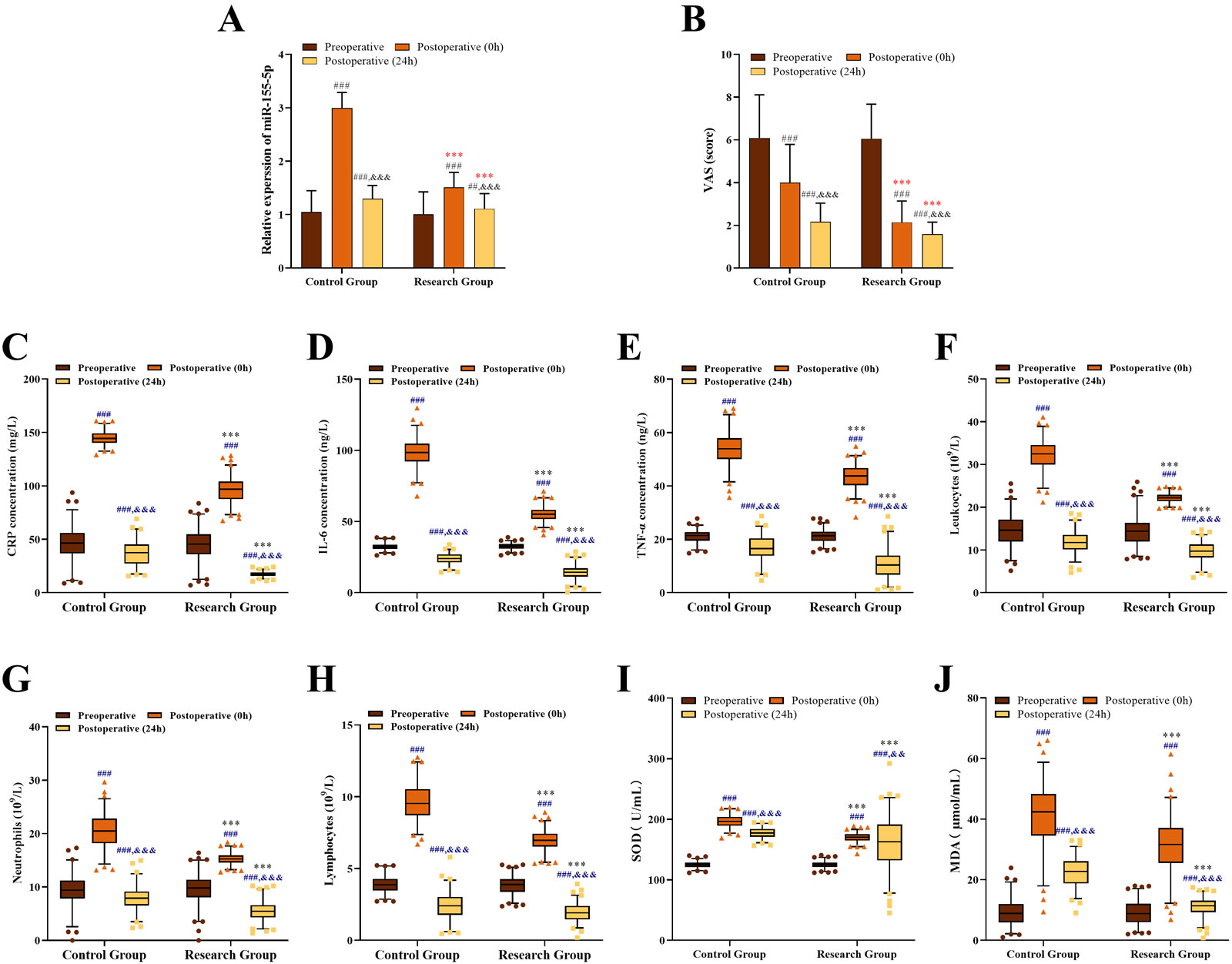
CRP, C-reactive protein; IL-6, interleukin-6; MDA, malondialdehyde; SOD, superoxide dismutase; TNF-α, tumor necrosis factor-α; VAS, visual analog scale.
Furthermore, there was no significant difference in preoperative VAS scores between the laparotomy and laparoscopy groups (P>0.05). The VAS scores for the laparoscopy group were significantly lower than those of the laparotomy group at both 0 and 24 h post- surgery (P<0.001, Fig. 1B). In comparison to preoperative levels, VAS scores for patients in both groups demonstrated a significant reduction following surgery (P<0.001), with the scores at 24 h post-surgery being significantly lower than those recorded at 0 hours post-surgery (P<0.001, Fig. 1B).
Levels of inflammatory factors and oxidative stress indexes
The results of the analysis conducted using ELISA and blood smear techniques indicated comparable alterations in the levels of CRP (Fig. 1C), IL-6 (Fig. 1D), TNF-α (Fig. 1E), as well as the counts of leukocytes (Fig. 1F), neutrophils (Fig. 1G), and lymphocytes (Fig. 1H) in the serum of both patient groups. No statistically significant difference was observed in the concentration of inflammatory markers in the preoperative serum between the laparotomy and laparoscopy groups (P>0.05). However, the levels of inflammatory markers in the serum of the laparoscopy group were significantly lower than those in the laparotomy group at both 0 and 24 h post-surgery (P<0.001). In comparison to preoperative levels, the serum concentrations of inflammatory markers in both the laparotomy and laparoscopy groups exhibited a significant increase immediately following surgery (P<0.001), followed by a significant decrease at 24 h post-surgery (P<0.001), ultimately significantly lower than preoperative levels (P<0.001).
The results of the ELISA analysis indicated that there was no statistically significant difference in the levels of SOD and MDA in the preoperative serum between the laparotomy and laparoscopy group patients (P>0.05). The serum levels of SOD and MDA in the laparoscopy group patients were found to be significantly lower than those in the laparotomy group at both 0 and 24 h post-surgery (P<0.001, Fig. 1I and Fig. 1J). In comparison to preoperative levels, both groups patients exhibited a significant increase in SOD and MDA levels immediately following surgery (P<0.001), followed by a significant decrease at 24 h post-surgery (P<0.01). Nevertheless, the levels at this time point remained significantly elevated compared to preoperative measurements (P<0.001, Fig. 1I and Fig. 1J).
Relationship of miR-155-5p expression level with inflammatory factors, oxidative stress indexes, and VAS score
The results of the Pearson correlation analysis are presented in Table II. The expression levels of miR-155-5p in the preoperative serum of the two patient groups demonstrated significant positive correlations with various inflammatory factors measured 24 h post-surgery, including CRP (r=0.546, P<0.001), IL-6 (r=0.628, P<0.001), TNF-α (r=0.808, P<0.001), leukocytes (r=0.778, P<0.001), neutrophils (r=0.718, P<0.001), and lymphocytes (r=0.820, P<0.001). Additionally, significant positive correlations were also observed with oxidative stress markers, specifically SOD (r=0.671, P<0.001) and MDA (r=0.489, P<0.001), as well as with VAS scores (r=0.671, P<0.001). Therefore, the expression level of miR-155-5p in serum might serve as a crucial predictive parameter for preoperative inflammatory factors, oxidative stress indicators, and VAS scores.
|
P<0.05 indicates a significant difference. CRP, C-reactive protein; IL, interleukin; MDA, malondialdehyde; SOD, superoxide dismutase; TNF, tumor necrosis factor; VAS, visual analog scale. |
||
| Table II. Correlations between miR-155-5p and various inflammatory markers, oxidative stress indexes, and VAS score. | ||
| Factors | Correlation coefficient (r) | P value |
| CRP (mg/L) | 0.546 | <0.001 |
| IL-6 (ng/L) | 0.628 | <0.001 |
| TNF-α (ng/L) | 0.808 | <0.001 |
| Leukocytes (×109/L) | 0.778 | <0.001 |
| Neutrophils (×109/L) | 0.718 | <0.001 |
| Lymphocytes (×109/L) | 0.820 | <0.001 |
| SOD (U/mL) | 0.671 | <0.001 |
| MDA (µmol/mL) | 0.489 | <0.001 |
| VAS (score) | 0.366 | <0.001 |
Relationship between miR-155-5p expression level and complication occurrence
A total of 16 patients experienced complications, with 13 from the laparotomy group and 3 from the laparoscopy group (Table III). The occurrence of postoperative complications was higher in patients who underwent OA (P<0.01). The predominant complications identified in the laparotomy group included mesenteric adhesions and bowel obstruction. Further analysis using the chi-square test indicated demographic and clinical characteristics—such as age, gender, course of the disease, intraoperative bleeding, length of stay, and VAS scores between the two groups concerning the incidence of complications were not significantly different (P>0.05). Notably, the duration of surgery, anal exhaust time, levels of inflammatory markers (including CRP, IL-6, TNF-α, leukocytes, neutrophils, and lymphocytes), and indicators of oxidative stress (SOD and MDA) demonstrated a significant correlation with the occurrence of complications (P<0.01, Table IV). Patients who developed complications exhibited prolonged surgery and anal exhaust times, elevated levels of inflammatory cytokines and MDA, and reduced levels of SOD.
| P<0.05 indicates a significant difference. | ||||
| Table III. Complications after resection in pediatric patients with acute suppurative appendicitis based on group. | ||||
| Factors | Total (N=316) | Laparotomy group (n=150) | Laparoscopy group (n=166) | P value |
| Incision infection, n (%) | 5 (1.58%) | 3 (2.00%) | 2 (1.20%) | 0.572 |
| Mesenteric adhesions, n (%) | 5 (1.58%) | 5 (3.33%) | 0 (0.00%) | 0.018 |
| Bowel obstruction, n (%) | 6 (1.90%) | 5 (3.33%) | 1 (0.60%) | 0.076 |
| All complications, n (%) | 16 (5.06%) | 13 (8.66%) | 3 (1.80%) | 0.005 |
|
P<0.05 indicates a significant difference. Data are presented as mean ± standard deviation, except for gender. CRP, C-reactive protein; IL, interleukin; MDA, malondialdehyde; SOD, superoxide dismutase; TNF, tumor necrosis factor; VAS, visual analog scale. |
|||
| Table IV. Relationship between complications and clinicopathological variables. | |||
| Factors | Complications | P value | |
| Yes (n=16) | No (n=300) | ||
| Age, years | 9.06 ± 2.64 | 8.10 ± 3.36 | 0.262 |
| Gender, n (%) | 0.304 | ||
| Male | 5 (31.25%) | 141 (47.00%) | |
| Female | 11 (68.75%) | 159 (53.00%) | |
| Course of the disease, days | 1.35 ± 0.45 | 1.23 ± 0.66 | 0.443 |
| Duration of surgery, min | 62.68 ± 6.68 | 54.89 ± 9.84 | 0.002 |
| Intraoperative bleeding, mL | 21.88 ± 9.91 | 18.86 ± 8.25 | 0.160 |
| Anal exhaust time, h | 3.69 ± 0.72 | 3.05 ± 0.97 | 0.009 |
| Length of stay, days | 8.27 ± 2.10 | 7.67 ± 2.78 | 0.395 |
| CRP, mg/L | 76.55 ± 6.89 | 44.04 ± 13.65 | <0.001 |
| IL-6, ng/L | 37.41 ± 0.94 | 32.23 ± 2.03 | <0.001 |
| TNF-α, ng/L | 26.09 ± 0.98 | 20.90 ± 2.15 | <0.001 |
| Leukocytes, ×109/L | 22.58 ± 1.64 | 14.10 ± 3.11 | <0.001 |
| Neutrophils, ×109/L | 15.06 ± 1.01 | 9.26 ± 2.60 | <0.001 |
| Lymphocytes, ×109/L | 5.07 ± 0.13 | 3.80 ± 0.55 | <0.001 |
| SOD, U/mL | 114.18 ±1.41 | 125.47 ± 4.95 | <0.001 |
| MDA, µmol/mL | 18.22 ± 1.91 | 8.72 ± 3.81 | <0.001 |
| VAS score | 6.06 ± 1.95 | 6.11 ± 2.03 | 0.237 |
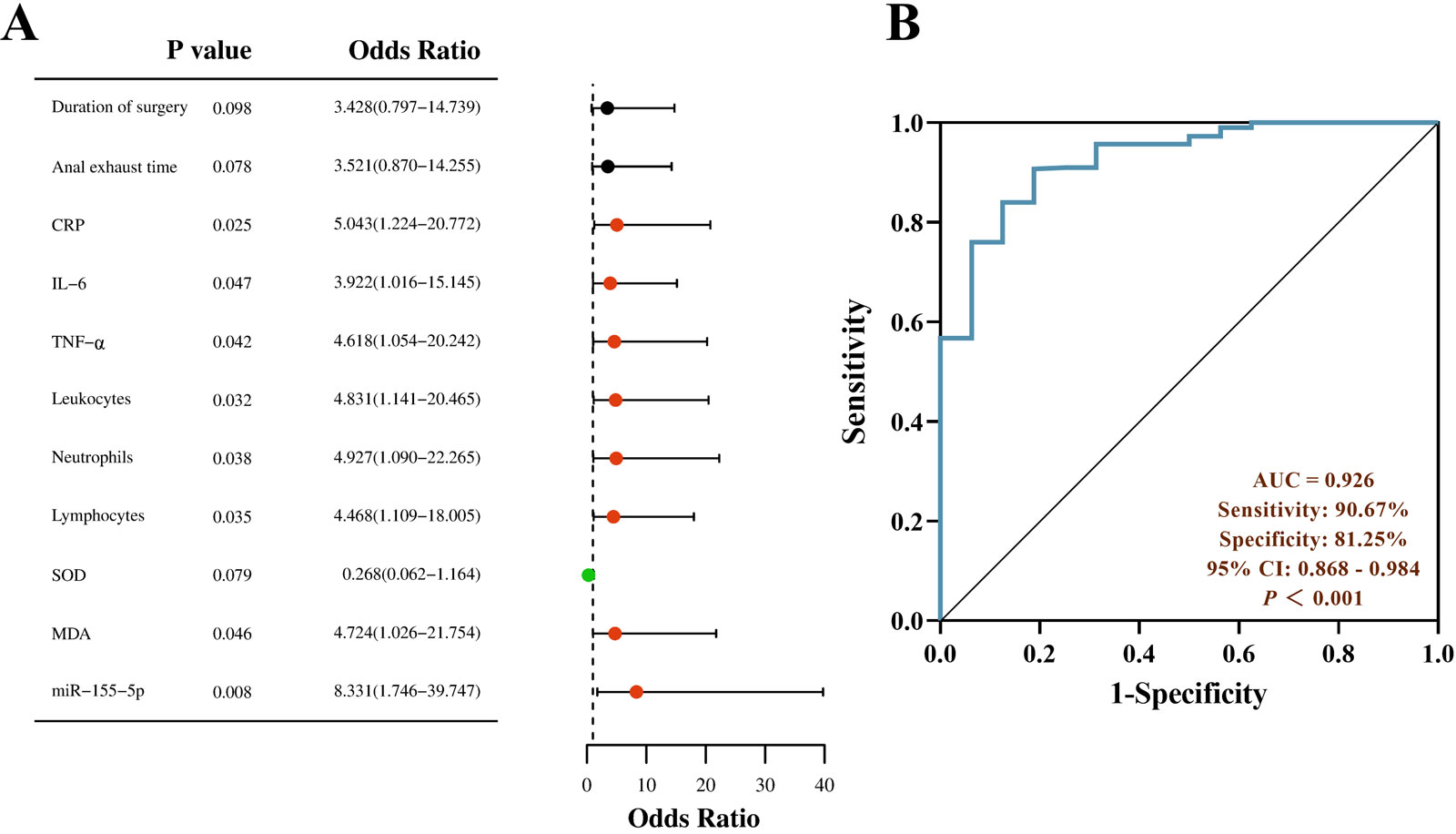
Logistic regression analysis revealed that several indicators were significant risk factors for postoperative complications in patients. Specifically, CRP exhibited an OR of 5.043 (95% CI: 1.224-20.772, P=0.025), IL-6 had an OR of 3.922 (95% CI: 1.016-15.145, P=0.047), and TNF-α demonstrated an OR of 4.618 (95% CI: 1.054-20.242, P=0.042). Additionally, leukocytes (OR=4.831, 95% CI: 1.141-20.465, P=0.032), neutrophils (OR=4.927, 95% CI: 1.090-22.265, P=0.038), lymphocytes (OR=4.468, 95% CI: 1.109-18.005, P=0.035), and MDA levels (OR=4.724, 95% CI: 1.026-21.754, P=0.046) were also identified as significant risk factors. Conversely, SOD was found to be a protective factor, with an OR of 0.268 (95% CI: 0.062-1.164, P=0.079). Notably, miR-155-5p emerged as the most influential factor regarding the occurrence of complications (OR=8.331, 95% CI: 1.746-39.747, P=0.008, Fig. 2A). Further analysis using ROC curves indicated that the area under the curve (AUC) for miR-155-5p in predicting complications occurrence was 0.926 (95% CI: 0.868-0.984), demonstrating high sensitivity (90.67%) and specificity (81.25%, Fig. 2B).
Discussion
Due to the incomplete development of the appendix in children, their ability to limit inflammation is poor. In instances where the appendix becomes inflamed and is not addressed promptly, there is a risk of developing significant lymphedema in the lymph nodes, as well as the rapid onset of purulent appendicitis.15 Open appendectomy, a traditional and well-established procedure, is associated with considerable trauma and physical damage.16 Conversely, laparoscopic appendectomy, characterized as a minimally invasive technique that integrates contemporary surgical and endoscopic methods, offers a broader surgical field of view, as well as less trauma and damage.17 This study indicated that patients undergoing LA experienced shorter operation times, and reduced intraoperative blood loss than OA, was consistent with previously reported data.18 The surgical process can lead to significant alterations in gene expression levels post-surgery, which might play a role in the body’s inflammatory response and immune regulation. These genes influence the release of inflammatory mediators and immune processes by modulating the activation or inhibition of associated pathways and the expression of target genes.19 Numerous studies have identified a variety of abnormally expressed miRNAs in organisms or cells undergoing inflammatory responses.20 As mentioned earlier, miR-155-5p has been implicated in the regulation inflammatory responses in various diseases.12-14 Furthermore, research utilizing a rat model of inflammation has demonstrated that miR-155-5p functions as a pro-inflammatory factor, inhibiting the nuclear factor kappa-B (NF-Κb) signaling pathway, which in turn exacerbates inflammatory damage.21 This study found similar results, revealing that the expression of miR-155-5p was pronounced fluctuation observed in patients undergoing OA relative to those undergoing LA. Additionally, inflammatory markers, indicators of oxidative stress, and VAS scores exhibited a significant positive correlation with miR-155-5p. Therefore, we preliminary speculated that the variations in these indicators during the perioperative period in patients with appendicitis might not solely be attributable to the smaller incision associated with LA, but might also be influenced by the activity of miR-155-5p.
Inflammatory indexes such as CRP, TNF-α, and IL-6 are both pro-inflammatory cytokines, and their elevated levels serve as indicators of inflammation within the body.22 Leukocytes, neutrophils, and lymphocytes play crucial roles in the inflammatory process, exhibiting phagocytic, immune, and tissue-damaging activities.23 The findings of this study indicated that both patient groups experienced an increase in postoperative inflammatory markers; however, patients who underwent LA exhibited a lower change of these markers compared to those who underwent OA. This suggested that LA might mitigate the inflammatory response elicited by surgical intervention.
Superoxide dismutase, an active compound in biological systems, is secreted in substantial amounts to safeguard cells in response to injury or damage.24 Malondialdehyde is a widely recognized indicator of stress response. An increase in MDA levels signifies the oxidative stress state of cells.25 On the first postoperative day, SOD levels in LA patients exhibited significant yet relatively minor fluctuations compared to their immediate postoperative levels, whereas SOD levels in OA patients demonstrated considerable variability. MDA levels in LA patients in postoperative 24 h were significantly lower than immediately after surgery. Although MDA levels in patients undergoing OA also showed a significant decrease, they remained markedly elevated compared to those in LA patients, indicating that OA exerts a more pronounced effect on oxidative stress in pediatric patients, while LA appears to promote stabilization.
Surgical interventions inherently involve a certain level of trauma, which can potentially lead to various complications.26 The LA mitigates the drawbacks associated with manual exploration and extensive incisions typical of traditional OA.27 The use of laparoscopy decreases the duration of appendectomy procedures, helps prevent infections.28 The findings of this study indicate that the incidence of short-term complications among patients undergoing LA was significantly lower compared to those undergoing OA, which is consistent with previous research findings. This study affirmed that LA was superior to OA concerning perioperative and postoperative complications. Furthermore, our findings indicated that inflammatory factors, MDA, and miR-155-5p served as risk factors for the development of complications, whereas SOD functioned as a protective factor. miR-155-5p possessed significant predictive capability regarding the occurrence of complications, suggesting that preoperative levels of miR-155-5p could aid in determining the appropriate surgical approach for patients. Elevated levels of miR-155-5p could facilitate the secretion of inflammatory mediators, augment the organism’s inflammatory and stress responses, and impede the healing processes of tissues and blood vessels in the vicinity of surgical incisions. Consequently, this might elevate the likelihood of bleeding complications in patients. Furthermore, if preoperative levels of miR-155-5p are markedly elevated, these patients may be better suited for LA, as this approach may mitigate substantial fluctuations in miR-155-5p during the perioperative period, thereby reducing inflammation, oxidative stress, and the associated complications that contribute to patient discomfort. This approach offers a more straightforward, scientifically grounded, and cost-effective method for selecting surgical techniques.
This research also has certain limitations, while it encompasses various aspects and indicators, including clinical, preoperative, and postoperative comparisons, it represents merely an initial exploration into the relationship between miR-155-5p and the methods and complications associated with appendectomy. The findings indicated that the expression of miR-155-5p correlated with levels of inflammation and oxidative stress in patients with ASA, as well as the onset of complications. This also suggests that clinical samples could be further expanded to explore the potential molecular mechanisms of miR-155-5p regulation through the integration of in vitro cellular experiments and in vivo animal models.
In conclusion, miR-155-5p played a role in modulating the body’s stress response, which in turn influenced the levels of inflammation and oxidative stress markers. The variability in miR-155-5p expression levels of patients undergoing OA was significantly greater than LA. Furthermore, miR-155-5p demonstrated considerable predictive value regarding the likelihood of complications and might serve as a reference indicator for determining appropriate surgical approaches for patients.
Ethical approval
This study received approval from the Ethics Committee of Xingtai People’s Hospital and adhered to the principles outlined in the Helsinki Declaration.
Source of funding
This study was funded by Medical Science Research Project of Hebei (20201585).
Conflict of interest
The authors declare that there is no conflict of interest.
References
- Duan C, Li Y, Ma J, Song Y, Zhou L. The impact of laparoscopic appendectomy and open appendectomy on B7-H3-mediated intrinsic immune response in children with acute suppurative appendicitis. J Inflamm Res 2024; 17: 1577-1587. https://doi.org/10.2147/JIR.S446199
- Nishimura K, Terui K, Mise N, et al. Larger physique as a risk factor for infantile appendicitis: a retrospective study. Pediatr Rep 2022; 14: 20-25. https://doi.org/10.3390/pediatric14010004
- Snyder MJ, Guthrie M, Cagle S. Acute appendicitis: efficient diagnosis and management. Am Fam Physician 2018; 98: 25-33.
- Fujishiro J, Watanabe E, Hirahara N, et al. Laparoscopic versus open appendectomy for acute appendicitis in children: a nationwide retrospective study on postoperative outcomes. J Gastrointest Surg 2021; 25: 1036-1044. https://doi.org/10.1007/s11605-020-04544-3
- Grijalva Estrada OB, Garrido Pérez JI, Murcia Pascual FJ, Ibarra Rodríguez MR, Paredes Esteban RM. Clavien-Dindo classification: a tool to assess complications following surgical treatment in children with acute appendicitis. Cir Pediatr 2022; 35: 18-24. https://doi.org/10.54847/cp.2022.01.14
- Lu TX, Rothenberg ME. MicroRNA. J Allergy Clin Immunol 2018; 141: 1202-1207. https://doi.org/10.1016/j.jaci.2017.08.034
- Ho PTB, Clark IM, Le LTT. MicroRNA-based diagnosis and therapy. Int J Mol Sci 2022; 23: 7167. https://doi.org/10.3390/ijms23137167
- Ginckels P, Holvoet P. Oxidative stress and inflammation in cardiovascular diseases and cancer: role of non-coding RNAs. Yale J Biol Med 2022; 95: 129-152.
- Saad N, Duroux-Richard I, Touitou I, Jeziorski E, Apparailly F. MicroRNAs in inflammasomopathies. Immunol Lett 2023; 256-257: 48-54. https://doi.org/10.1016/j.imlet.2023.04.001
- Essandoh K, Li Y, Huo J, Fan GC. MiRNA-mediated macrophage polarization and its potential role in the regulation of inflammatory response. Shock 2016; 46: 122-131. https://doi.org/10.1097/SHK.0000000000000604
- Jafarzadeh A, Naseri A, Shojaie L, et al. MicroRNA-155 and antiviral immune responses. Int Immunopharmacol 2021; 101: 108188. https://doi.org/10.1016/j.intimp.2021.108188
- Singh A, Patro PS, Aggarwal A. MicroRNA-132, miR-146a, and miR-155 as potential biomarkers of methotrexate response in patients with rheumatoid arthritis. Clin Rheumatol 2019; 38: 877-884. https://doi.org/10.1007/s10067-018-4380-z
- Ndzi EN, Nkenfou CN, Mekue LM, et al. MicroRNA hsa-miR-29a-3p is a plasma biomarker for the differential diagnosis and monitoring of tuberculosis. Tuberculosis (Edinb) 2019; 114: 69-76. https://doi.org/10.1016/j.tube.2018.12.001
- Petejova N, Martinek A, Zadrazil J, et al. Acute kidney injury in septic patients treated by selected nephrotoxic antibiotic agents-pathophysiology and biomarkers-a review. Int J Mol Sci 2020; 21: 7115. https://doi.org/10.3390/ijms21197115
- Fall F, Berman L. Antibiotic use in gangrenous, suppurative, or exudative appendicitis. JAMA Surg 2024; 159: 517-518. https://doi.org/10.1001/jamasurg.2023.7776
- Del Pino C, Muñoz R, Rada G. Laparoscopic versus open appendectomy for complicated appendicitis. Medwave 2018; 18: e7370. https://doi.org/10.5867/medwave.2018.08.7369
- Köhler F, Hendricks A, Kastner C, et al. Laparoscopic appendectomy versus antibiotic treatment for acute appendicitis-a systematic review. Int J Colorectal Dis 2021; 36: 2283-2286. https://doi.org/10.1007/s00384-021-03927-5
- Liu T, Jiang K, Bi Y. Endoscopic retrograde appendicitis therapy in a pregnant patient with acute septic appendicitis. Asian J Surg 2022; 45: 2070-2071. https://doi.org/10.1016/j.asjsur.2022.04.098
- Furák J, Paróczai D, Burián K, Szabó Z, Zombori T. Oncological advantage of nonintubated thoracic surgery: better compliance of adjuvant treatment after lung lobectomy. Thorac Cancer 2020; 11: 3309-3316. https://doi.org/10.1111/1759-7714.13672
- Noonin C, Thongboonkerd V. Exosome-inflammasome crosstalk and their roles in inflammatory responses. Theranostics 2021; 11: 4436-4451. https://doi.org/10.7150/thno.54004
- Shao Y, Li Y, Jiang Y, Li H, Wang J, Zhang D. Circulating exosomal miR-155-5p contributes to severe acute pancreatitis-associated intestinal barrier injury by targeting SOCS1 to activate NLRP3 inflammasome-mediated pyroptosis. FASEB J 2023; 37: e23003. https://doi.org/10.1096/fj.202300237R
- Wojdasiewicz P, Poniatowski ŁA, Szukiewicz D. The role of inflammatory and anti-inflammatory cytokines in the pathogenesis of osteoarthritis. Mediators Inflamm 2014; 2014: 561459. https://doi.org/10.1155/2014/561459
- Zahorec R. Neutrophil-to-lymphocyte ratio, past, present and future perspectives. Bratisl Lek Listy 2021; 122: 474-488. https://doi.org/10.4149/BLL_2021_078
- Li C, Che LH, Ji TF, Shi L, Yu JL. Effects of the TLR4 signaling pathway on apoptosis of neuronal cells in diabetes mellitus complicated with cerebral infarction in a rat model. Sci Rep 2017; 7: 43834. https://doi.org/10.1038/srep43834
- Jin G, Zheng J, Zhang Y, Yang Z, Chen Y, Huang C. LncRNA UCA1 epigenetically suppresses APAF1 expression to mediate the protective effect of sevoflurane against myocardial ischemia-reperfusion injury. Funct Integr Genomics 2022; 22: 965-975. https://doi.org/10.1007/s10142-022-00874-4
- Blanco Verdú MD, Peláez Mata DJ, Gómez Sánchez A, et al. Re-interventions following appendectomy in children: a multicenter study. Cir Pediatr 2022; 35: 70-74. https://doi.org/10.54847/cp.2022.02.14
- Fadgyas B, Garai GI, Ringwald Z, Őri D, Vajda P. Laparoscopic appendectomy in children evaluation of the learning curve. Orv Hetil 2022; 163: 1001-1004. https://doi.org/10.1556/650.2022.32485
- Güler Y, Karabulut Z, Çaliş H, Şengül S. Comparison of laparoscopic and open appendectomy on wound infection and healing in complicated appendicitis. Int Wound J 2020; 17: 957-965. https://doi.org/10.1111/iwj.13347
Copyright and license
Copyright © 2025 The Author(s). This is an open access article distributed under the Creative Commons Attribution License (CC BY), which permits unrestricted use, distribution, and reproduction in any medium or format, provided the original work is properly cited.















