Abstract
Background: The treatment modalities for testicular appendage torsion in children are classified as conservative or surgical, and the choice is controversial.
Objectives: This study aimed to identify ultrasound-based indicators influencing the outcome of conservative treatment in children with testicular appendage torsion to divide the boundaries between conservative and surgical management.
Methods: A retrospective analysis was conducted on testicular appendage torsion data of children from November 2022 and November 2023 in the Children’s Hospital of Zhejiang University School of Medicine to compare the conservatively successful and conservatively unsuccessful groups’ clinical and ultrasound characteristics. Furthermore, we constructed a logistic regression model and evaluated its predictive ability.
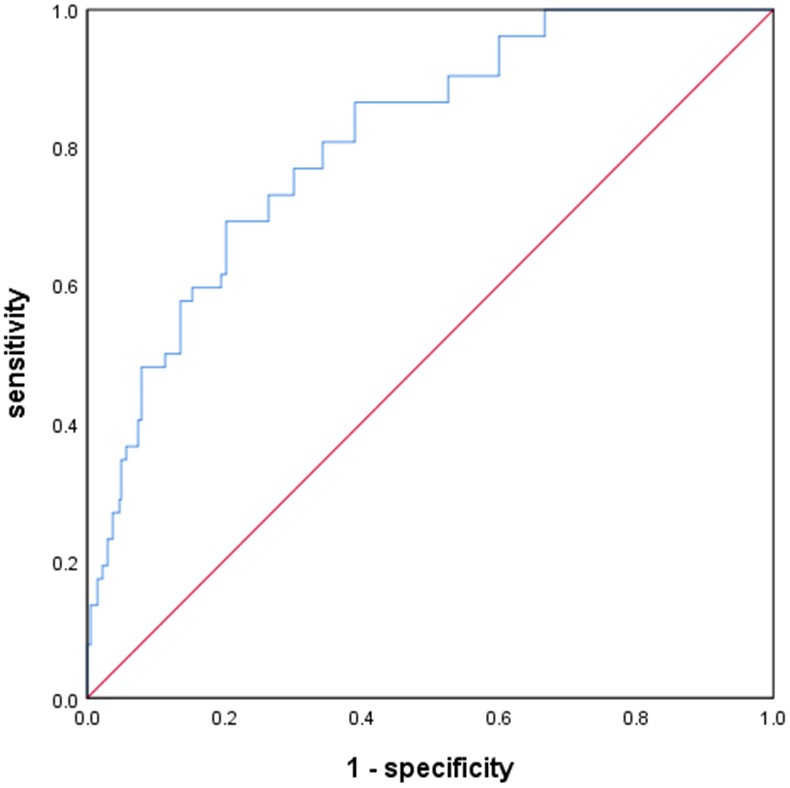
Results: We observed 405 (88.62%) and 52 (11.38%) cases of conservative success and failure, respectively. Univariate analysis indicated significant differences between these groups in testicular appendage torsion nodule size, terminology for hydrocele, scrotal wall edema, and increased epididymal blood flow (p<0.05). Additionally, binary logistic regression analysis indicated that the testicular appendage torsion nodule size was an independent risk factor influencing conservative treatment outcomes. There was a 12.3% rise in the incidence ratio of conservative failure (Odds ratio [OR] 1.123, 95% confidence interval [CI] 1.055-1.195, p<0.05) for every 1 mm2 increase in nodule size. The receiver operating characteristic (ROC) curve revealed an optimal critical value of 23.56 mm2, corresponding to an area under the curve (AUC) of 0.810, a sensitivity of 0.692, and a specificity of 0.798 (95% CI 0.752-0.867, p<0.05).
Conclusions: When the size of the testicular appendage torsion node measured by ultrasound exceeds 23.56 mm2, conservative treatment is predicted to fail, and surgical treatment may be considered. This result has certain clinical application potential and can be used as one of the important indicators to assist decision-making.
Keywords: child, scrotum, testicular appendage torsion, ultrasonography, surgery
Introduction
Testicular appendages are the remnants of the mesonephric or paramedian ducts, typically ovoid and pedunculated, commonly located at the upper pole of the testis or adjacent to the epididymis. Testicular appendage torsion is a common cause of scrotal emergencies in children.1 Children and adolescents tend to present with sudden scrotal pain, while infants present with crying and refusal to be touched on one side of the scrotum. Physical examination may reveal tenderness and a palpable nodule above the testicle.2 Since it lacks specific clinical manifestations, ultrasonography is the preferred diagnostic tool, offering non-invasive, rapid and accurate results.3-5 Typical ultrasound findings include a torsion nodule and absent blood flow on color Doppler ultrasound.6 The treatment modalities for testicular appendage torsion are classified as conservative or surgical.7 Historically, conservative treatment was favored, as the condition was considered self-limiting. However, recent studies have demonstrated the advantages of surgical treatment, particularly in cases with severe inflammatory manifestations, intractable pain, or recurrent pain after remission, and that surgical treatment can ensure that the testicular appendage torsion on that side will not recur and shorten the time for pain relief and disappearance of edema.7 The study of Shi et al.8 made a small scrotal incision for testicular appendage resection after precise positioning of testicular appendage torsion, which shortened the operation time and reduced intraoperative bleeding and postoperative pain compared with traditional surgery. Although surgery is a good solution to the problem, there are currently no objective screening indicators to use as an indication for surgery, which may lead to questions about the existence of over-surgery. Furthermore, a report by Horiike et al.9 suggested that if the testicular appendage torsion is more than 10 mm in diameter, it may wrap around the testis or epididymis, resulting in necrosis due to obstruction of blood flow to the testis. Although the importance of ultrasound in the diagnosis of testicular appendage torsion is widely recognized, there is a relative lack of studies on the relationship between ultrasound characteristics and treatment decisions, which makes it difficult for specialists to derive more clues from the ultrasound report when determining treatment options. In practice, ultrasound can clearly reveal not only the testicular appendage nodules but also the morphology and blood flow in the testis and its surrounding structures. Therefore, based on the above studies, we hypothesized that the existence of certain ultrasound indices, such as size and blood flow, can be used as a basis for surgery.
In this study, we aimed to identify ultrasound-based indicators influencing the outcome of conservative treatment in children with testicular appendage torsion to divide the boundaries between conservative and surgical management.
Materials and Methods
Patients
Subjects: The study was approved by the Ethics Committee of the Affiliated Children’s Hospital of Zhejiang University School of Medicine, and the requirement for informed consent was waived (Ethics No. 2024-IRB-0167-P-01). We retrospectively analyzed 457 patients clinically diagnosed with testicular appendage torsion from November 2022 to November 2023 at the Affiliated Children’s Hospital of Zhejiang University School of Medicine.
The inclusion criteria were: 1. Patients with the clinical diagnosis of testicular appendage torsion; 2. Those with complete medical records, and all patients received conservative treatment after diagnosis, including oral or intravenous antibiotics; 3. Patients with clear ultrasound images. The exclusion criteria were: 1. Patients with congenital genitourinary anomalies; 2. Those with other grave systemic diseases; 3. Patients with scrotal disease requiring urgent surgery such as suspected or combined testicular torsion.
The patient’s age, height, weight, time of examination (time from the initial onset of symptoms to the time of ultrasound examination), and treatment modality were collected from the electronic case system. Treatment modalities were categorized as conservative success or conservative failure, with the latter defined as the need for conversion to surgery (hereafter referred to as conservative failure). Patients were assessed by specialists on the first day and every two days thereafter. The criteria for determining the failure of conservative treatment include persistent or worsening pain following conservative management, necessitating surgical intervention for resolution. Conversely, pain alleviation after conservative treatment was considered the criterion for the success of conservative management. The pathological diagnosis of the operated patients was confirmed.
Equipment
We used a Logiq E9 ultrasound machine (GE, USA), and the line array probe’s frequency was 10 MHz.4 The ultrasound parameters were set to small organ mode, and the grey scale image scanning depth, gain, and focus point were adjusted until the scrotal structures were distinct and uniformly indicated. While the mechanical and thermal indexes were <0.4, the color Doppler ultrasound flow velocity was 3-6 cm/s.
Imaging analysis
Patients with clear ultrasound images: two-dimensional including testicular appendage torsion nodules, bilateral testes, epididymis, spermatic cord, scrotal wall, and inguinal area, as well as color Doppler ultrasound images of testicular appendage torsion nodules and epididymal blood flow. Two senior ultrasonographers who worked in the hospital for >10 years analyzed the patients. In the event of a disagreement in their conclusions, a third experienced sonographer was invited to participate in the evaluation.
Our observation indexes were: 1. The testicular appendage torsion nodule’s location, echo, size, and blood flow. Since the testicular appendage tended to be ovoid, the oval area was used as a proxy for size. The left and right diameters were measured along with the upper and lower diameters in the section with the largest area of the torsion nodule. Size = π × left and right diameter/2 × upper and lower diameter/2 mm2. 2. Other signs of inflammation, including the presence or absence of enlargement of the affected epididymis compared with the healthy side, enlargement of the testis and spermatic cord, presence or absence of the terminology for hydrocele, edema of the scrotal wall, and increased blood flow to the epididymis.
Statistical analysis
We used SPSS 26.0 software for data analysis. Count and metric data were expressed as rate (n, %) and , respectively. An independent sample t-test was used to compare metric data between the two groups. At the same time, the χ2 test was utilized for count data. All values of p<0.05 were considered statistically significant. After constructing the binary logistic regression model, the Wald χ2 test was used to estimate the regression parameters, whereas the likelihood ratio test evaluated the model’s fit. The receiver operating characteristic (ROC) curve was employed to evaluate the logistic regression model’s forecasting ability.
Results
Comparison of general data
We included 457 cases, of which 425 (93.00%) had no obvious causative factors, and 32 (7.00%) were associated with sports, trauma, or surgical injury. Age at onset was 0.5-17.0 years (8.99±2.51 years), height and weight were 102.0-164.0 cm (139.32±15.22 cm) and 8.0-95.5 kg (35.10±12.77 kg), respectively. The examination time was 0-14 days (2.60±2.49 days), and the left-sided onset was seen in 229 (50.11%) cases. Moreover, right-sided lesions were found in 228 (49.89%) cases. There were 405 (88.62%) and 52 (11.38%) cases of conservative success and failure, respectively.
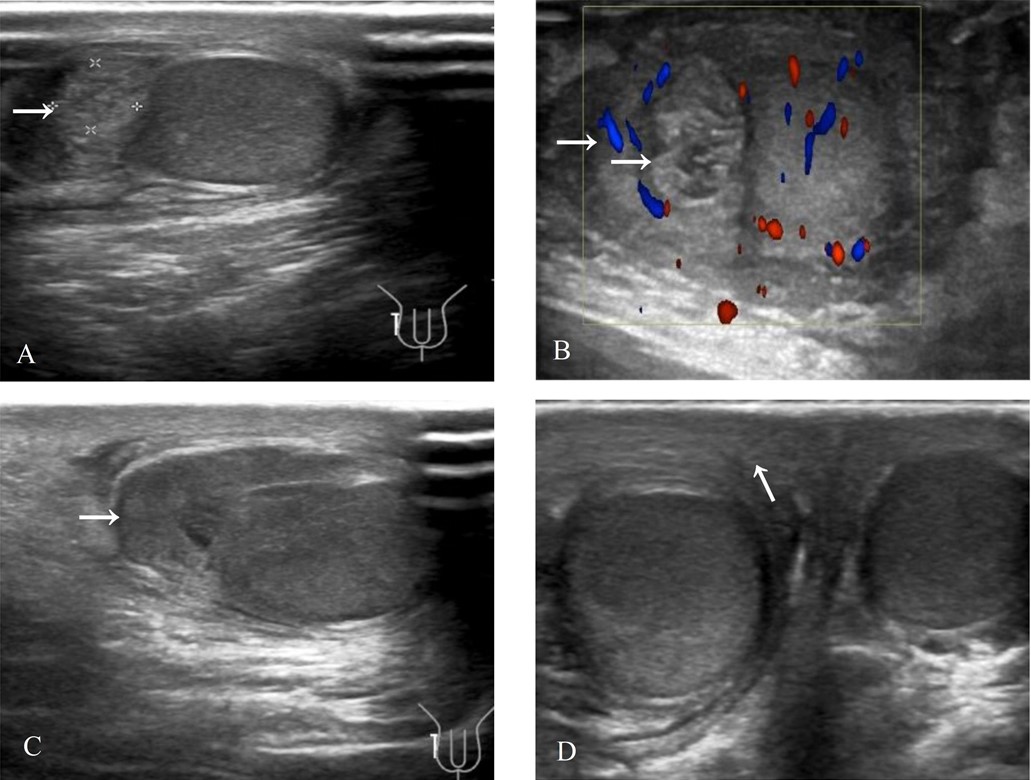
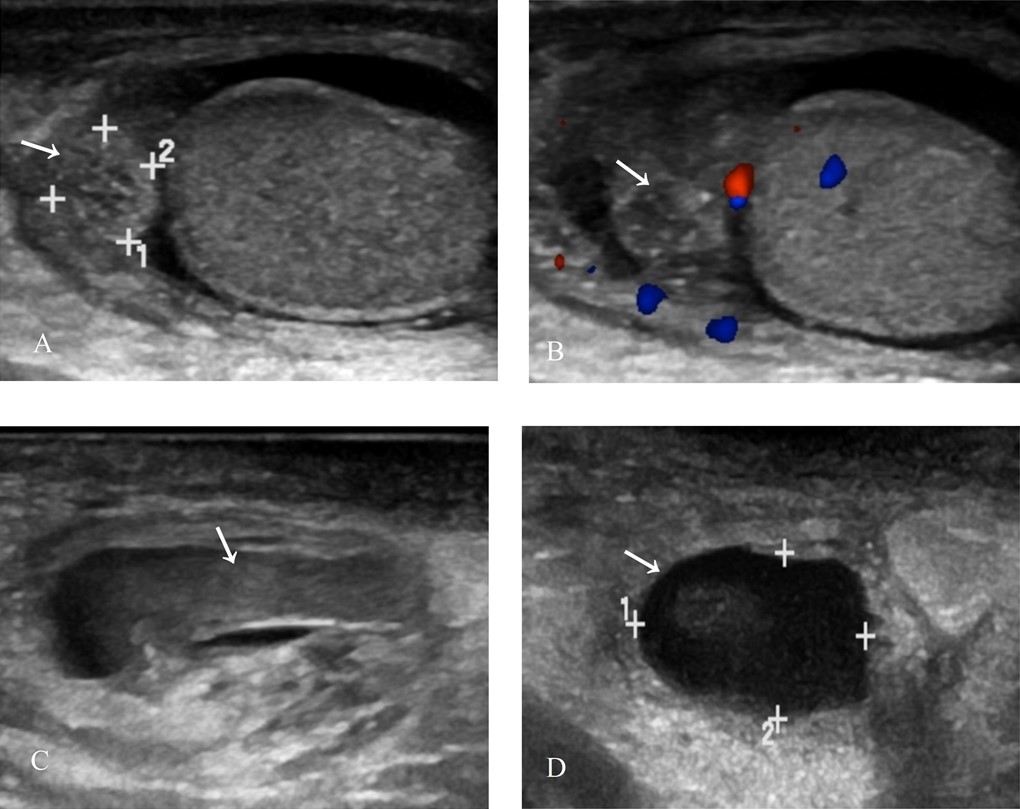
In pediatric testicular appendage torsion patients, ultrasound images revealed a testicular appendage torsion nodule in the affected scrotum, frequently accompanied by enlarged epididymis on the affected side, terminology for hydrocele, and edema of the affected or bilateral scrotal walls; the echogenicity, size, and position of the testes and spermatic cords were not visibly altered. The color Doppler ultrasound revealed absent blood flow in the torsion nodules and increased blood flow in some epididymis, respectively (Fig. 1 and Fig. 2).
Comparison of general information and ultrasound image characteristics in conservative Success and Failure Groups
The patients’ general information in the two conservative success and conservative failure groups included age, height, weight, and examination time, without any significant differences between the groups (p>0.05, Table I). The ultrasound image characteristics showed the torsion nodule’s location, echo, and epididymal enlargement, without any significant differences between the groups (p>0.05, Table II). However, the differences in the four ultrasound features, i.e., testicular appendage torsion nodule’s size, terminology for hydrocele, scrotal wall edema, and increased blood flow in the epididymis, respectively, were statistically significant between the groups (p<0.05, Table II).
| Data presented as mean ± standard deviation. All values of p<0.05 were considered statistically significant. | ||||
| Table I. Comparison of general information between conservative success and failure groups in testicular appendage torsion. | ||||
| Group | Conservative success (n=405) | Conservative failure (n=52) | T value | P value |
| Age (years) | 8.97±2.53 | 9.15±2.29 | 1.505 | 0.221 |
| Height (cm) | 138.94±14.64 | 139.52±15.66 | 0.217 | 0.643 |
| Weight (kg) | 34.83±12.91 | 37.21±11.60 | 0.686 | 0.408 |
| Inspection time (days) | 2.60±2.44 | 2.63±2.23 | 1.220 | 0.270 |
| Torsion of nodule size (mm2) | 17.21±11.52 | 33.83±19.37 | 22.438 | <0.001 |
| χ², chi-square. Data presented as counts and percentages. All values of p<0.05 were considered statistically significant. | |||||||
| Table II. Comparison of ultrasound characteristics between conservative success and failure groups in testicular appendage torsion. | |||||||
| Group | Conservative success (n=405) | Conservative failure (n=52) |
χ2 value | P value | |||
| n | % | n | % | ||||
| Position of torsion of nodule | Left | 201 | 49.6 | 28 | 53.8 | 0.328 | 0.567 |
| Right | 204 | 50.4 | 24 | 46.2 | |||
| Torsion nodule echo | High | 231 | 57.0 | 37 | 71.2 | 3.787 | 0.052 |
| Low | 174 | 43.0 | 15 | 28.8 | |||
| Epididymal swelling | Yes | 334 | 82.5 | 48 | 92.3 | 3.252 | 0.075 |
| No | 71 | 17.5 | 4 | 7.7 | |||
| Terminology for hydrocele | Yes | 166 | 41.0 | 34 | 65.4 | 11.145 | 0.001 |
| No | 239 | 59.0 | 18 | 34.6 | |||
| Edema of the scrotal wall | Yes | 182 | 44.9 | 38 | 73.1 | 14.615 | <0.001 |
| No | 223 | 55.1 | 14 | 26.9 | |||
| Increased blood flow in epididymis | Yes | 234 | 57.8 | 46 | 88.5 | 18.284 | <0.001 |
| No | 171 | 42.2 | 6 | 11.5 | |||
Logistic regression analysis of factors influencing the failure of conservative testicular appendage torsion treatment
With the failure of conservative treatment as the dependent variable and statistically significant variables in the univariate analysis as independent variables, including testicular appendage torsion nodule size (mm2), terminology for hydrocele, scrotal wall edema, and increased epididymal blood flow, the stepwise regression was used to incorporate all four of these indicators, and the results revealed that testicular appendage torsion nodule size had an independent predictive value for conservative failure (χ2=24.436, p<0.05, Table III). The incidence ratio of conservative failure increased by 12.3 percent ((e0.116-1)*100%) for each 1 mm2 increase in the size of the testicular appendage torsion nodule.
| B value, Beta value; SE, standard error; OR, odds ratio; CI, confidence interval. | ||||
| Table III. Multifactorial stepwise regression analysis of ultrasound-related indicators with regards to conservative failure of testicular appendage torsion | ||||
| Variant | Β value | SE | P value | OR (95% CI) |
| Torsion of nodule size (mm2) | 0.116 | 0.032 | <0.001 | 1.123 (1.055-1.195) |
| Constant | -1.843 | 0.662 | 0.005 | - |
ROC analysis of testicular appendage torsion nodule size as a diagnostic indicator
Fig. 3 reveals that the ROC curve was plotted using the testicular appendage torsion nodule size as the diagnostic outcome value and the conservative outcome as the ‘gold standard’. The Jordon’s index (J = Sensitivity + Specificity - 1) was calculated to be 0.49, which corresponded to an optimal threshold for the size of testicular appendage torsion nodules of 23.56 mm2, with an area under the curve (AUC) of 0.810, a sensitivity of 0.692, and a specificity of 0.798, with a 95% confidence interval of 0.752-0.867.
Discussion
Testicular appendage torsion is a common cause of scrotal emergencies in children, with a peak incidence between the ages of 6-12 years old, with androgen and estrogen receptors in the testicular adnexal structures, and the occurrence of torsion may be related to increased stimulation by sex hormones before puberty.10 Most cases have no obvious trigger; a few may be associated with exercise, trauma, or surgery. It can develop on both the left and right sides without obvious favoritism. Its clinical presentation is sudden scrotal pain, but in infants, unexplained crying and refusal to be touched in the scrotum should also rule out testicular appendage torsion. Diagnosis can be aided by identifying a small nodule over the testicle and increased pain on palpation. Although conservative treatment is often effective, failure may cause aseptic inflammation of the epididymis, potentially causing infertility due to vas deferens obstruction.11,12 However, no studies have indicated how to assess the risk of conservative failure of testicular appendage torsion. Gopal et al.13 believe that the full use of clinical and ultrasound data should be made to limit emergency scrotal exploration to children at higher risk. Ultrasound is of great interest as the examination of choice for this disease, from which more useful information can be obtained to screen patients at high risk of conservative failure to assist in clinical assessment.14
Our study retrospectively analyzed 457 patients with testicular appendage torsion, of whom 52 (11.38%) experienced conservative treatment failure. Difficulty in relieving pain may be related to the extent of testicular appendage torsion, and ultrasound can reveal the torsion of the testicular appendage itself and associated inflammatory changes, such as hydrocele, edema of the scrotal wall, and increased blood flow to the epididymis. The study identified the nodule size as an independent predictive value for conservative failure, with the incidence ratio of conservative failure increasing by 12.3% for each 1 mm2 increase in nodule size. The risk of conservative failure was high when nodule size exceeded 23.56 mm2 (AUC = 0.810). Compared to the case report of Horiike et al.9, who used the diameter of the testicular appendage torsion nodule, our study selected the area of the largest section of the torsional nodule, which is perhaps more accurate. Hydrocele, scrotal wall edema, and increased blood flow to the epididymis are signs of inflammation, which aligns with Tanaka et al.7, who recommended surgical treatment for severe inflammatory symptoms. In addition, some scholars have recommended surgical treatment for patients with recurrent pain after improvement with conservative treatment.15
Differentiating testicular appendage torsion from testicular torsion is critical, and the key distinctions lie primarily in the age of presentation and symptom severity. Testicular torsion is more common in adolescents and typically prompts immediate evaluation due to its severity. In contrast, testicular appendage torsion often presents with milder symptoms, leading to potential delays in assessment and a higher likelihood of localized inflammatory signs.
This study’s strength lies in its substantial number of clinical cases and the development of a logistic regression model to quantitatively evaluate the ultrasound characteristics, providing a scientific basis for clinical decision-making. Upcoming studies can explore more factors that might influence treatment choices to improve the prediction model’s accuracy and efficiency. Since this was a single-center study, our model’s applicability in different healthcare institutions requires further validation. Future studies should explore additional predictive factors, and conduct multi-center validation to improve the model’s accuracy and generalizability.
Conclusion
This study has identified ultrasound indicators that significantly influence the outcomes of conservative treatment in children with testicular adnexal torsion. Notably, the size of the testicular adnexal torsion nodule emerged as an independent predictor of the failure of conservative management. This pivotal finding would offer a quantitative foundation for distinguishing between cases suitable for conservative versus surgical interventions, thereby addressing the prevailing gap in objective ultrasound criteria guiding surgical indications.
Ethical approval
The study was approved by the Ethics Committee of the Affiliated Children’s Hospital of Zhejiang University School of Medicine, and informed consent was waived (date: January 24th, 2024, number: 2024-IRB-0167-P-01).
Source of funding
The authors declare that the study is supported/funded by Zhejiang Provincial Public Welfare Technology Application Research Project, grant number: LGF22H180002.
Conflict of interest
The authors declare that there is no conflict of interest.
References
- Tan Tanny SP, Wijekoon N, Pacilli M, Nataraja RM. Clinical state of the paediatric acute scrotum in south-eastern Victoria. ANZ J Surg 2019; 89: 1615-1619. https://doi.org/10.1111/ans.15399
- Jefferies MT, Cox AC, Gupta A, Proctor A. The management of acute testicular pain in children and adolescents. BMJ 2015; 350: h1563. https://doi.org/10.1136/bmj.h1563
- Kummari S, Das S, Mahajan S. Role of high-resolution ultrasonography with colour and duplex doppler in the evaluation of acute scrotal diseases. Cureus 2023; 15: e49231. https://doi.org/10.7759/cureus.49231
- Wunsch R. Ultrasound imaging of the testes in children and adolescents. Radiologie (Heidelb) 2024; 64: 35-44. https://doi.org/10.1007/s00117-023-01220-w
- Madsen SMD, Rawashdeh YF. Assessing timeline delays associated with utilization of ultrasound diagnostics in paediatric acute scrotum, pre and per COVID-19 pandemic. J Pediatr Urol 2023; 19: 653.e1-653.e7. https://doi.org/10.1016/j.jpurol.2023.07.003
- Deeg KH. Differential diagnosis of acute scrotum in childhood and adolescence with high-resolution duplex sonography. Ultraschall Med 2021; 42: 10-38. https://doi.org/10.1055/a-1325-1834
- Tanaka K, Kato H, Nikai K, Mikami T, Okazaki T. Testicular appendage torsion in children. Pediatr Int 2022; 64: e15010. https://doi.org/10.1111/ped.15010
- Shi J, Chen Z, Zhang L, Li H. Scrotal small-incision to remove the testicular appendage for the treatment of patients with testicular appendage torsion: an experience of 230 cases. Asian J Surg 2024; 47: 2012-2013. https://doi.org/10.1016/j.asjsur.2023.12.208
- Horiike M, Yokoyama S, Yokoyama K, Yoshida A. Testicular appendage torsion resulting in testicular ischemia and necrosis in a child. Journal of Pediatric Surgery Case Reports 2021; 74: 102024. https://doi.org/10.1016/j.epsc.2021.102024
- Samnakay N, Cohen RJ, Orford J, King PA, Davies RJ. Androgen and oestrogen receptor status of the human appendix testis. Pediatr Surg Int 2003; 19: 520-524. https://doi.org/10.1007/s00383-002-0936-7
- Lotti F, Studniarek M, Balasa C, et al. The role of the radiologist in the evaluation of male infertility: recommendations of the European Society of Urogenital Radiology-Scrotal and Penile Imaging Working Group (ESUR-SPIWG) for scrotal imaging. Eur Radiol 2025; 35: 752-766. https://doi.org/10.1007/s00330-024-10964-5
- Laimer G, Müller R, Radmayr C, Lindner AK, Lebovici A, Aigner F. Multiparametric ultrasound in torsion of the testicular appendages: a reliable diagnostic tool? Med Ultrason 2022; 24: 33-37. https://doi.org/10.11152/mu-3206
- Gopal M, O’Connor E, McDonald L, et al. Emergency scrotal exploration in children: is it time for a change in mindset in the UK? J Pediatr Urol 2021; 17: 190.e1-190.e7. https://doi.org/10.1016/j.jpurol.2020.11.029
- Lim SH, Yang DM, Kim HC, et al. Ultrasonography of intrascrotal torsed appendages: size and interval between symptom onset and the ultrasonographic examination according to echogenicity. Ultrasonography 2023; 42: 259-264. https://doi.org/10.14366/usg.22169
- Lala S, Price N, Upadhyay V. Re-presentations and recurrent events following initial management of the acute paediatric scrotum: a 5-year review. ANZ J Surg 2019; 89: E117-E121. https://doi.org/10.1111/ans.13905
Copyright and license
Copyright © 2025 The Author(s). This is an open access article distributed under the Creative Commons Attribution License (CC BY), which permits unrestricted use, distribution, and reproduction in any medium or format, provided the original work is properly cited.















