Abstract
Objective: This study aimed to determine whether children diagnosed with attention deficit hyperactivity disorder (ADHD) continue to receive this diagnosis during adolescence and young adulthood, and to examine the relationships between autistic traits, psychological resilience, emotion regulation levels, and the continuity of diagnosis.
Methods: In the initial evaluations conducted between 2012 and 2013, 121 children diagnosed with ADHD began medication treatment. From this group, 20 participants aged 13 to 25 who agreed to participate in the second evaluation, conducted between 2020 and 2022, were included in this study. The presence of ADHD in their second evaluation was determined using the DSM-5 criteria. Psychiatric comorbidities in adolescents were screened using the Schedule for Affective Disorders and Schizophrenia for School-Age Children - Present and Lifetime Version, 2016 Turkish Adaptation of the DSM-5, while for adults, the DSM-5 criteria were utilized. Parents completed the Social Responsiveness Scale and the Family Assessment Device, while the young participants completed the Child and Youth Resilience Measure and the Difficulties in Emotion Regulation Scale.
Results: Among the participants, 10 individuals (50%) continued to have an ADHD diagnosis, exhibiting lower psychological resilience and significantly more autistic traits. No difference in emotional dysregulation was observed between those with and without an ADHD diagnosis, and a negative relationship between autistic traits and psychological resilience was identified.
Conclusion: The continuity of an ADHD diagnosis during adolescence and young adulthood may be associated with psychological resilience and autistic traits. However, the limited number of participants and the cross-sectional design highlight the need for larger longitudinal studies to further explore the cause-and-effect relationships.
Keywords: adolescence, attention deficit hyperactivity disorder, autism spectrum disorder, emotion regulation, psychological resilience
Introduction
Attention deficit hyperactivity disorder (ADHD) is a neurodevelopmental disorder that begins in childhood and is characterized by symptoms of inattention, hyperactivity, and impulsivity.1 It is estimated that ADHD affects 5.9% of adolescents and 2.5% of adults.2,3 Studies indicate that 60-85% of children diagnosed with ADHD continue to exhibit symptoms during adolescence.4 Additionally, research on the prevalence of ADHD in adulthood has produced varying findings, with a reported persistence rate ranging from 5% to 75%.5
Factors associated with the continuity of an ADHD diagnosis during adolescence and young adulthood include familiarity with ADHD, psychosocial adversity, comorbidity with conduct, mood, and anxiety disorders, parental conflict, childhood sexual assault, lower educational attainment, income loss, severity of ADHD, family history of psychopathology, family and school functioning, behavioral impairment, lower intelligence quotient (IQ), and cyclothymic, irritable, or anxious temperament.6-12
Autistic traits, which encompass social deficits, communication challenges, and repetitive behaviors that do not meet the criteria for a diagnosis of autism spectrum disorder (ASD), are present in approximately 30% of children diagnosed with ADHD.13,14 These children often exhibit a more severe form of ADHD compared to those without autistic traits. Furthermore, they experience greater impairments in functional areas such as academics, activities, and social interactions compared to their peers without autistic traits.15-18
Emotion regulation refers to an individual’s ability to adjust their emotional state in an adaptive and goal-directed manner.19 Recent studies emphasize that difficulties in emotion regulation are a fundamental component of the ADHD diagnosis.20 In cases where ADHD is accompanied by deficient emotional self-regulation from childhood through adolescence, higher rates of psychiatric comorbidities, particularly oppositional defiant disorder (ODD), persistence of ADHD, and social problems, along with functional impairments, have been observed during follow-up.21
Psychological resilience is the capacity to effectively cope with, adapt to, or manage stress and challenging circumstances.22 Research has shown that psychological resilience tends to be weaker in adolescents and young adults diagnosed with ADHD compared to those without the diagnosis.23,24 Emerging adults with ADHD identify several important resilience factors, including strategies for managing ADHD, supportive relationships, acceptance, a positive perception of their ADHD, tailored non-stigmatizing support, and engagement in meaningful activities.25 Better psychological resilience among adolescents with ADHD is correlated with improved psychosocial functioning and a lower incidence of depression and anxiety disorders in young adulthood.26
Upon reviewing the literature, while various studies indicate that difficulties in emotion regulation are associated with the persistence of ADHD diagnoses during adolescence21,27, other research has shown that autistic traits exacerbate the clinical presentation of ADHD, increase comorbidities, and lead to poorer functioning.15-17 A longitudinal study conducted with a population sample indicated that autistic traits and ADHD traits are reciprocal, often decreasing, persisting, or emerging together over time.28 However, to the best of our knowledge, no research has specifically examined the impact of autistic traits on the continuity of ADHD diagnoses, nor have studies investigated the effect of psychological resilience on ADHD diagnosis continuity.
Considering the negative impact of autistic traits and emotion dysregulation on ADHD’s clinical presentation, we aimed to investigate the relationship between the continuity of the ADHD diagnosis in adolescents and adults diagnosed in childhood and these variables. Additionally, we sought to explore the relationship between psychological resilience and the persistence of the ADHD diagnosis, emphasizing the need to assess both negative and positive traits in psychiatric evaluations. This study, utilizing a cross-sectional design due to the limited sample size, focuses on the continuation of the ADHD diagnosis as individuals transition from childhood to adolescence and young adulthood, particularly regarding autistic traits, psychological resilience, and emotion regulation.
We hypothesized that psychological resilience will be weaker, problems with emotional regulations will be more pronounced, autistic traits and clinical deterioration will be more common in the group with an ongoing ADHD diagnosis.
Materials and Methods
Participants
The participants in this study consisted of individuals who were included in the research conducted by Ünal et al. between 2012 and 2013 , during which they were diagnosed with ADHD based on assessments performed at that time and began medication treatment while aged 6 to 18 years.29 These individuals were contacted again by phone between January 2020 and December 2022, invited to the Department of Child and Adolescent Psychiatry at Hacettepe University, and those who volunteered to participate were included in the study after it was confirmed that they met the inclusion criteria during psychiatric evaluations.
Participants with intellectual disabilities, anxiety disorders, mood disorders, ASD, psychotic disorders, substance use disorders, chronic illnesses, and neurological conditions were excluded from the study during the initial assessments in childhood. However, children with specific learning disorders, ODD, and conduct disorder (CD) comorbidities were included in the study. In our current study, participants with chronic and neurological conditions, ASD, intellectual disabilities, psychotic disorders, and substance use disorders were excluded.
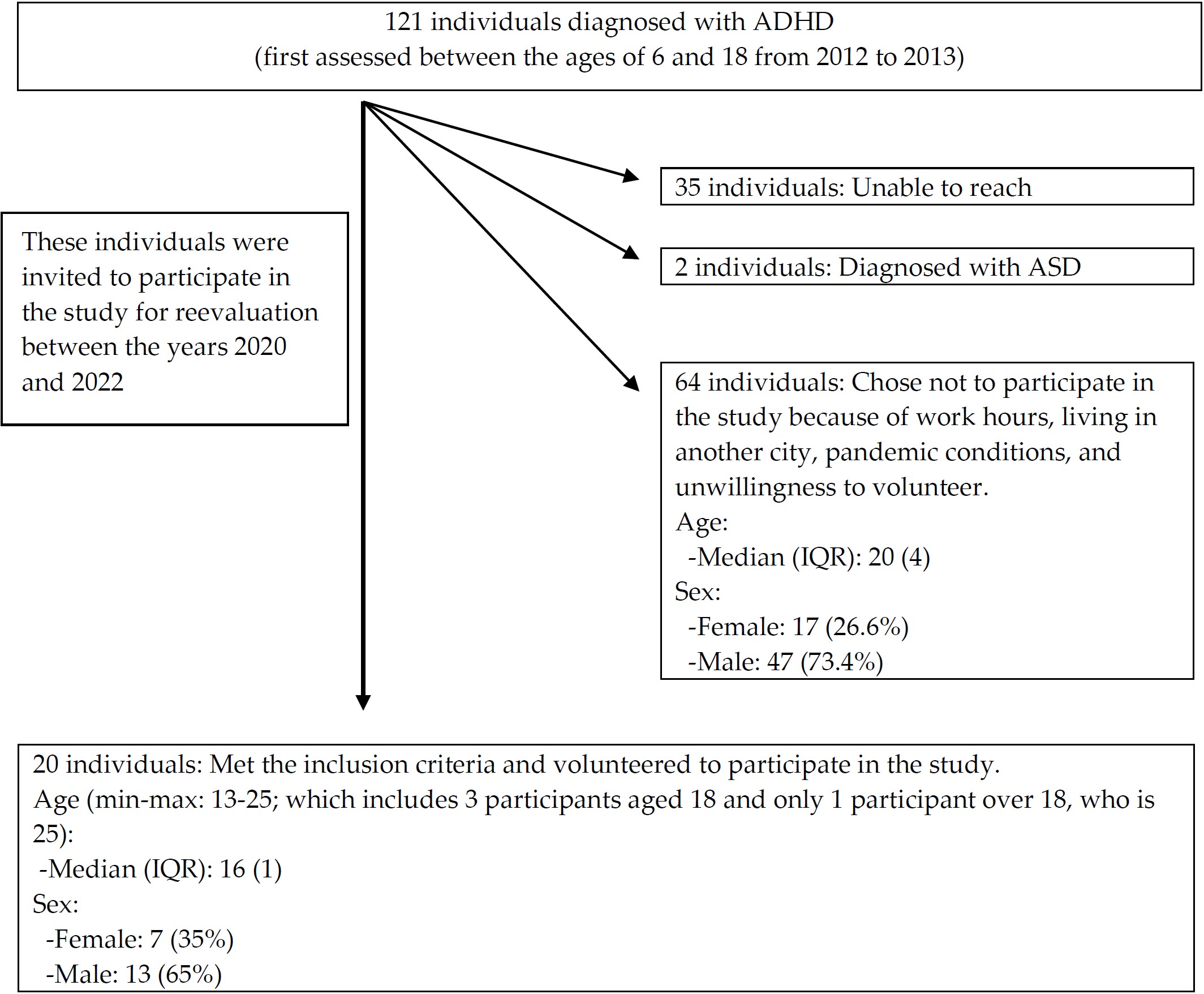
Out of the 121 individuals targeted for participation, 35 could not be reached, 2 were diagnosed with ASD, and 64 chose not to participate for various reasons (such as work commitments, residing in another city, pandemic conditions, or unwillingness to volunteer). As a result, 20 participants (3 aged 18, 1 aged 25, and the remaining participants under 18) with ages ranging from 13 to 25 years (7 females and 13 males) were included in our study. The flow of the study sample formation is illustrated in Fig. 1.
If the participants were under 18 years of age, written consent was obtained from both themselves and their parents; if they were over 18, consent was obtained from the participants themselves.
Ethics approval
The ethical approval for this study was granted by the Hacettepe University Non-Interventional Clinical Research Ethics Committee on November 5, 2019, with decision number 2019/26-36.
Materials
In our study, the ongoing presence of an ADHD diagnosis among participants was determined according to DSM-5 criteria.1 For participants under the age of 18, the presence of additional psychiatric comorbidities and an ASD diagnosis was assessed using the Schedule for Affective Disorders and Schizophrenia for School-Age Children - Present and Lifetime Version, 2016 Turkish Adaptation of the DSM-5 (K-SADS-PL-DSM-5-T), administered by a child and adolescent psychiatrist. For participants aged 18 and over, all diagnoses available in the K-SADS were screened during the psychiatric evaluation based on DSM-5 criteria.
The sociodemographic information form, prepared by the researchers, and the clinical information form, which inquired about ADHD-related clinical information and psychosocial stressors, were completed by the parents. All of the scales described below were completed by the participants during their second evaluations in adolescence and young adulthood. The scales used in the study are described below:
Schedule for Affective Disorders and Schizophrenia for School-Age Children - Present and Lifetime Version, DSM-5 - Turkish Adaptation (K-SADS-PL-DSM-5-T): This semi-structured interview, developed by Kaufman et al.30 and adapted in Turkish by Ünal et al.31, assesses ADHD and comorbid disorders in children and adolescents. It was utilized to evaluate the continuity of the ADHD diagnosis. This interview tool was used with participants under the age of 18.
Social Responsiveness Scale (SRS): This 65-item scale evaluates autism-like symptoms in children aged 4 to 18. Developed by Constantino et al.32 and adapted by Ünal et al.33, it was used to compare autistic traits between participants with and without an ADHD diagnosis. This scale was completed by the parents of all participants.
Child and Youth Resilience Measure (CYRM-12): Developed by Liebenberg et al.34, this 12-item scale measures resilience in individuals over 10 years old. The Turkish validity and reliability study was conducted by Arslan.35 This scale assessed the relationship between ADHD diagnosis and resilience levels and was completed based on self-report by all participants in our study.
Difficulties in Emotion Regulation Scale (DERS): A 36-item scale designed for individuals aged 18 and older, developed to measure difficulties in emotion regulation.36 The Turkish validation was completed by Rugancı and Gençöz.37 This scale was used to investigate emotion regulation difficulties in participants with and without a persistent ADHD diagnosis and was completed based on self-reports by all participants in our study. Due to the majority of our sample being comprised of participants under the age of 18, the necessity of using this scale with this age group has been noted as a limitation.
Family Assessment Device (FAD): This scale, utilizing the McMaster Family Functioning Model, assesses family structure and functionality.38 The Turkish validity and reliability study was conducted by Bulut.39 It was utilized to examine the relationship between the continuity of the ADHD diagnosis and family functioning. The scale was completed by all participants.
Hollingshead-Redlich Scale: This scale measures family socioeconomic and sociocultural status.40 It was completed based on information obtained from the family by the researcher.
Clinical Global Impression Scale (CGI): Developed to assess psychiatric disorders across all ages, this scale includes sections for illness severity, global improvement, and efficacy index.41 It was used to determine the severity of ADHD-related problems and was completed based on the clinical assessment conducted by the researcher.
Global Assessment Scale (GAS): A clinician-administered scale assessing functionality, with scores ranging from 0 to 100, used to determine the participants’ levels of functioning over the past week.42 This scale was completed following the clinical assessment conducted by the researcher.
Statistical analysis
The Statistical Program for Social Sciences (SPSS) version 23.0 was used for data analysis. The normality of numerical variables was assessed using the Shapiro-Wilk goodness-of-fit test, while the homogeneity of variance was examined with Levene’s test. The independent two-sample t-test was employed for normally distributed variables, and the Mann-Whitney U test was used for those that were not normally distributed. Categorical variables are presented as numbers and percentages, and Pearson’s chi-square test and Fisher’s exact test were utilized for analysis based on expected frequencies. Spearman’s correlation test was employed to assess relationships between two quantitative variables. The significance level was set at p < 0.05, and effect sizes were computed for each statistical test to determine clinical relevance.
Results
Sociodemographic and clinical characteristics of participants
The sociodemographic characteristics of the participants, the status of the ongoing ADHD diagnosis, and other clinical variables are presented in Table I. Information regarding psychiatric comorbidities are included in Table II.
|
For those to which the t-test was applied, the Mean ± Standard Deviation notation was used. For those to which the Mann-Whitney U test was applied, the Median (Interquartile Range) notation was used. The percentages given in the table are column percentages. ADHD, attention deficit hyperactivity disorder; CGI, Clinical Global Impression Scale; GAS, Global Assessment Scale. |
|
| Table I. Sociodemographic and clinical characteristics of participants. | |
| Variable |
|
|
|
|
| Age |
|
| Socio-economic level |
|
| CGI disease severity score |
|
| CGI improvement score |
|
|
|
|
| GAS score |
|
|
|
|
| Sex | |
| Female |
|
| Male |
|
| Mother's education level | |
| Below high school |
|
| High school and above |
|
| Father's education level | |
| Below high school |
|
| High school and above |
|
| ADHD diagnosis | |
| Yes |
|
| No |
|
| ADHD treatment | |
| Continues treatment |
|
| Stopped treatment |
|
| Psychiatric treatment in the last six months | |
| Yes |
|
| No |
|
| Psychosocial stressor | |
| Yes |
|
| No |
|
| Self-harming behavior | |
| Yes |
|
| No |
|
| Suicide plan/attempt | |
| Yes |
|
| No |
|
| Forensic case history | |
| Yes |
|
| No |
|
| The percentages given in the table are column percentages. | |
| Table II. Psychiatric comorbidities of participants, N (%). | |
| Variable |
|
| Depression | |
| None |
|
| Threshold/subthreshold |
|
| Social anxiety disorder | |
| None |
|
| Threshold/subthreshold |
|
| Generalized anxiety disorder | |
| None |
|
| Threshold/subthreshold |
|
| Specific phobia | |
| None |
|
| Threshold/subthreshold |
|
| Tic disorder | |
| None |
|
| Threshold/subthreshold |
|
| Obsessive-compulsive disorder | |
| None |
|
| Threshold/subthreshold |
|
| Panic disorder | |
| None |
|
| Threshold/subthreshold |
|
Comparison of groups with and without ongoing ADHD diagnosis
In the group still diagnosed with ADHD, the GAS score was significantly lower, indicating poorer functionality. In this group, CGI scores for disease severity and improvement were significantly higher, suggesting greater current severity and less improvement compared to the past. The Social Responsiveness Scale (SRS) score was also significantly higher, reflecting a greater presence of autistic traits, while the CYRM-12 score was significantly lower, indicating reduced resilience. There were no significant differences between the two groups in terms of the DERS and FAD scores (Table III).
|
p-value was obtained using the Mann-Whitney U test. *p<0,05 ADHD: attention deficit hyperactivity disorder, CGI: Clinical Global Impression Scale, CYRM-12: Child and Youth Resilience Measure-12, DERS: Difficulties in Emotion Regulation Scale, FAD: Family Assessment Device, GAS: Global Assessment Scale, SRS: Social Responsiveness Scale |
|||||
| Table III. Comparison of the mean ranks of the scale scores of groups with ongoing ADHD diagnosis and those no longer diagnosed with ADHD. | |||||
| Variable |
(N=10) |
(N=10) |
|
|
|
| GAS |
|
|
|
|
|
| CGI-disease severity |
|
|
|
|
|
| CGI-improvement |
|
|
|
|
|
| CYRM-12 |
|
|
|
|
|
| SRS |
|
|
|
|
|
| DERS-lack of emotional awareness |
|
|
|
|
|
| DERS-lack of emotional clarity |
|
|
|
|
|
| DERS-nonacceptance of emotional responses |
|
|
|
|
|
| DERS-limited access to emotion regulation strategies |
|
|
|
|
|
| DERS-impulse control difficulties |
|
|
|
|
|
| DERS-difficulty engaging in goal-directed behavior |
|
|
|
|
|
| FAD-problem solving |
|
|
|
|
|
| FAD-communication |
|
|
|
|
|
| FAD-role |
|
|
|
|
|
| FAD-affective responsive |
|
|
|
|
|
| FAD-affective involvement |
|
|
|
|
|
| FAD-behavioral control |
|
|
|
|
|
| FAD-general functionality |
|
|
|
|
|
A negative correlation was found across the entire group between psychological resilience and autistic traits (r = -0.530, p < 0.05), and psychological resilience also negatively related to lack of emotional clarity and difficulty in goal-directed behavior (DERS subscales) (r = -0.669, p < 0.05; r = -0.583, p < 0.05; Table IV). Additionally, there was no significant difference between the two groups regarding comorbid psychiatric disorders (Supplementary Table S1).
|
Spearman correlation test was performed. *Correlation is significant at the p<0.05 level. CYRM-12: Child and Youth Resilience Measure-12, DERS: Difficulties in Emotion Regulation Scale, SRS: Social Responsiveness Scale |
||||||||
| Table IV. Correlation test results between participants' SRS, CYRM-12, and DERS scale scores. | ||||||||
| SRS | CYRM-12 | DERS- lack of emotional clarity | DERS- lack of emotional awareness | DERS- nonacceptance of emotional responses | DERS- limited access to emotion regulation strategies | DERS- impulse control difficulties | DERS- difficulty engaging in goal-directed behavior | |
| SRS | ||||||||
| CYRM-12 |
|
|||||||
| DERS- lack of emotional clarity |
|
|
||||||
| DERS- lack of emotional awareness |
|
|
|
|||||
| DERS- nonacceptance of emotional responses |
|
|
|
|
||||
| DERS- limited access to emotion regulation strategies |
|
|
|
|
|
|||
| DERS- impulse control difficulties |
|
|
|
|
|
|
||
| DERS- difficulty engaging in goal-directed behavior |
|
|
|
|
|
|
|
|
There were no significant differences between the groups continuing to receive an ADHD diagnosis and those who did not, regarding the following variables: sociodemographic characteristics, prenatal/perinatal problems, developmental features, psychiatric treatment history, and familial and psychosocial stressors (Supplementary Table S2).
Discussion
This study aimed to determine whether adolescents and young adults who were initially diagnosed with ADHD during childhood and started on medication continue to meet the ADHD diagnosis, and to compare current adolescents and young adults with and without an ADHD diagnosis in terms of autism-like symptoms, psychological resilience, and emotion regulation levels. However, the inability of a significant portion of individuals over the age of 18 to participate in the study, the limited number of participants, and the likelihood that these individuals are still seeking treatment, as indicated by the median age of participants being 16, suggest that the findings should primarily be considered in the context of adolescent characteristics.
Sixty to eighty-five percent of children diagnosed with ADHD continue to demonstrate symptoms during adolescence.4 We found that the rate of retaining an ADHD diagnosis from childhood into adolescence is 50%. This rate is consistent with findings reported by other studies in the literature.43,44 However, the limited number of participants and the heterogeneous distribution in terms of age in our study prevent us from interpreting this finding as the continuation rate of the ADHD diagnosis during adolescence. Since the participants consisted of individuals who were diagnosed and began treatment during childhood (even though we found the treatment continuation rate to be 20%), and given that ADHD treatment is known to reduce symptom burden in adolescence and young adulthood45,46, this rate might have been higher if examined in a population that had never received treatment.
In our study, the most common threshold and subthreshold psychiatric comorbidities in young people diagnosed with ADHD were depression, anxiety disorders, and obsessive-compulsive disorder. This finding aligns with previous studies suggesting that these conditions are frequent among youth and adults with ADHD.47 Those diagnosed with depression and anxiety disorders were excluded during the initial evaluation; however, these comorbidities were still detected at high rates in our sample. Surprisingly, no cases of conduct or substance use disorders were found. This may be due to the study sample not living in a risky social environment and beginning ADHD treatment at an early age. Adolescents who participated in the study may have been more willing to complete time-consuming activities, such as scales and psychiatric interviews, while seeking help, which could explain the higher prevalence of internalizing disorders compared to disruptive disorders in our sample. If those who declined or were unreachable had been included, conduct disorder, substance use disorder, or academic and social issues might have been more apparent. Nonetheless, 10% of participants failed a class, 20% experienced peer bullying, 20% were involved in criminal cases, 25% had a history of self-harm, and 19% reported suicide plans or attempts. This indicates that some participants faced impairments in their individual, relational, educational, and social functioning despite the absence of conduct or substance abuse disorders. The attention and impulse control deficits in individuals diagnosed with ADHD can lead to deteriorating social skills, academic failure, accidents, antisocial behavior, and occupational and relational problems, even without comorbid diagnoses.48,49
In our study, we found that the group still meeting the ADHD diagnosis during adolescence exhibited significantly higher levels of autistic traits. Previous studies have shown that features of autism are associated with a worse clinical course in patients diagnosed with ADHD, and children diagnosed with both ADHD and autistic traits continued to exhibit these traits in their ten-year follow-up. They experienced more problems in interpersonal relationships as well as in educational and neurocognitive areas, and they had a higher burden of early-onset psychopathology.16,17 To the best of our knowledge, no study has specifically investigated the direct effect of autistic traits on the continuation of an ADHD diagnosis. While the limitations of our study’s methodology and its cross-sectional nature prevent us from making definitive interpretations, examining this issue in larger samples and through longitudinal designs could help fill the existing gap in the literature.
We found that the level of psychological resilience was significantly higher in the group that no longer met the ADHD diagnosis during adolescence compared to the group that still had the diagnosis. While some studies examining resilience in children diagnosed with ADHD found no significant differences in resilience between children diagnosed with ADHD and controls50,51, others suggested that resilience is lower in youth diagnosed with ADHD compared to controls23,26. The differing results may be attributed to the multidimensional nature of resilience, which includes individual, familial, and social-environmental factors. Resilience involves having multiple skills to cope with challenges.52 In our study, the lower resilience observed in the ADHD group may be related to the negative impact of ADHD on cognitive factors, self-regulation skills, peer relationships, and family functioning. Studies with larger samples and investigations of these multidimensional resilience factors are needed to shed light on this issue.
We found a significant negative relationship between resilience and autistic traits in all participants. To the best of our knowledge, there is currently no study examining the relationship between autistic traits and resilience. However, it has been shown that young people with autistic traits experience significant impairments in their social functioning and quality of life.53,54 Considering the multidimensional nature of resilience, it can be anticipated that young people with autistic traits may be more vulnerable in terms of resilience due to their psychosocial challenges. In our study, the lower resilience observed in the group with a continuing diagnosis of ADHD may be associated with the higher prevalence of autistic traits in this group. In the correlation analysis conducted with all participants, we found a negative relationship between resilience and autistic traits. However, further analytical methods are needed to determine whether the lower psychological resilience in individuals with ADHD is related to the core symptoms of ADHD itself or is influenced by autistic traits. Unfortunately, we could not perform this analysis due to the limited sample size per group for examining the relationship between autistic traits and resilience in both groups with and without a diagnosis. It is recommended that this gap in the literature regarding the relationship between autistic traits and resilience be investigated in studies with larger samples.
We also found a significant negative relationship between resilience and both lack of emotional clarity and difficulty in engaging in goal-directed behavior. However, we did not find a significant relationship between resilience and variables such as lack of emotional awareness, non-acceptance of emotional responses, limited access to emotion regulation strategies, and impulse control difficulties, which are other sub-dimensions of emotional regulation difficulties. Based on this finding, it can be concluded that resilience and emotion regulation are related but distinct concepts, with resilience encompassing a broader scope that includes emotion regulation.55
We did not find any statistically significant differences in emotion regulation skills between the groups that met the ADHD diagnosis during adolescence and those that did not. Emotional dysregulation in children with ADHD is linked to a higher incidence of psychiatric comorbidities, poorer social functioning, and persistence of ADHD.21 Our inability to find differences in emotion regulation skills may be due to improved emotional control from childhood treatment and ongoing neurodevelopment in adolescence.56,57 Studies have shown that psychostimulants reduce emotional lability and irritability in children58,59, and similar beneficial effects are observed in adults.60,61 However, it is important to note this limitation, as the scale measuring emotion regulation difficulties is primarily intended for adults. Additionally, the limited sample size may have contributed to our inability to detect differences between the groups with and without a diagnosis.
Our study has methodological limitations. We did not anticipate a low number of participants over the age of 18, which led to applying the DERS, typically for adults, to adolescents. Additionally, the study coincided with the pandemic, resulting in heterogeneous findings as some participants were evaluated before and others after the pandemic. Finally, the small sample size intended for a longitudinal study resulted in a cross-sectional design, limiting our ability to use advanced analytical techniques and necessitating caution in interpreting both significant and non-significant results.
Despite this limitation, the thorough evaluations of participants in both initial and follow-up assessments, the use of a semi-structured interview to identify comorbidities, and the investigation of possible psychosocial challenges are key strengths of our study. While the number of participants was small, they were comprehensively examined regarding various psychosocial and clinical variables. Furthermore, although this study followed a cross-sectional design, the lack of existing research on the relationship between autistic traits, psychological resilience, and the continuity of the ADHD diagnosis suggests that our study lays a foundation for establishing cause-and-effect relationships in future larger-sample longitudinal studies.
This study found that half of the adolescents diagnosed with ADHD in childhood and treated still met the criteria for an ADHD diagnosis. These adolescents exhibited more autistic traits and lower psychological resilience compared to those who no longer met the diagnosis. No significant differences were found in emotion regulation skills. Additionally, significant negative relationships were observed between autistic traits and psychological resilience, as well as between resilience and certain emotion regulation difficulties. These results should be interpreted with caution due to the limited sample size and cross-sectional nature of the study. Future follow-up studies with larger samples will enhance our understanding of the factors affecting the persistence of ADHD diagnosis.
Acknowledgements
We would like to thank Prof. Dr. Ebru Çengel Kültür for her significant contributions to the development of the study design.
Ethical approval
The study was approved by Non-Interventional Clinical Studies Ethics Committee of Hacettepe University (date: 05.11.2019, number: 2019/26-36).
Source of funding
The authors declare the study received no funding.
Conflict of interest
The authors declare that there is no conflict of interest.
References
- American Psychiatric Association (APA). Diagnostic and statistical manual of mental disorders: DSM-5. Washington, DC: APA; 2013. https://doi.org/10.1176/appi.books.9780890425596
- Willcutt EG, Nigg JT, Pennington BF, et al. Validity of DSM-IV attention deficit/hyperactivity disorder symptom dimensions and subtypes. J Abnorm Psychol 2012; 121: 991-1010. https://doi.org/10.1037/a0027347
- Simon V, Czobor P, Bálint S, Mészáros A, Bitter I. Prevalence and correlates of adult attention-deficit hyperactivity disorder: meta-analysis. Br J Psychiatry 2009; 194: 204-211. https://doi.org/10.1192/bjp.bp.107.048827
- Pliszka S, AACAP Work Group on Quality Issues. Practice parameter for the assessment and treatment of children and adolescents with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry 2007; 46: 894-921. https://doi.org/10.1097/chi.0b013e318054e724
- Sibley MH, Swanson JM, Arnold LE, et al. Defining ADHD symptom persistence in adulthood: optimizing sensitivity and specificity. J Child Psychol Psychiatry 2017; 58: 655-662. https://doi.org/10.1111/jcpp.12620
- Biederman J, Faraone S, Milberger S, et al. Predictors of persistence and remission of ADHD into adolescence: results from a four-year prospective follow-up study. J Am Acad Child Adolesc Psychiatry 1996; 35: 343-351. https://doi.org/10.1097/00004583-199603000-00016
- Ebejer JL, Medland SE, van der Werf J, et al. Attention deficit hyperactivity disorder in Australian adults: prevalence, persistence, conduct problems and disadvantage. PLoS One 2012; 7: e47404. https://doi.org/10.1371/journal.pone.0047404
- Caye A, Spadini AV, Karam RG, et al. Predictors of persistence of ADHD into adulthood: a systematic review of the literature and meta-analysis. Eur Child Adolesc Psychiatry 2016; 25: 1151-1159. https://doi.org/10.1007/s00787-016-0831-8
- Biederman J, Petty CR, O’Connor KB, Hyder LL, Faraone SV. Predictors of persistence in girls with attention deficit hyperactivity disorder: results from an 11-year controlled follow-up study. Acta Psychiatr Scand 2012; 125: 147-156. https://doi.org/10.1111/j.1600-0447.2011.01797.x
- Mick E, Byrne D, Fried R, Monuteaux M, Faraone SV, Biederman J. Predictors of ADHD persistence in girls at 5-year follow-up. J Atten Disord 2011; 15: 183-192. https://doi.org/10.1177/1087054710362217
- Agnew-Blais JC, Polanczyk GV, Danese A, Wertz J, Moffitt TE, Arseneault L. Evaluation of the persistence, remission, and emergence of attention-deficit/hyperactivity disorder in young adulthood. JAMA Psychiatry 2016; 73: 713-720. https://doi.org/10.1001/jamapsychiatry.2016.0465
- Skala K, Riegler A, Erfurth A, Völkl-Kernstock S, Lesch OM, Walter H. The connection of temperament with ADHD occurrence and persistence into adulthood - an investigation in 18 year old males. J Affect Disord 2016; 198: 72-77. https://doi.org/10.1016/j.jad.2016.03.051
- Constantino JN, Todd RD. Autistic traits in the general population: a twin study. Arch Gen Psychiatry 2003; 60: 524-530. https://doi.org/10.1001/archpsyc.60.5.524
- Uchida M, Faraone SV, Joshi G, et al. How prevalent are autistic traits among children with attention-deficit/hyperactivity disorder? A qualitative review of the literature. Scand J Child Adolesc Psychiatr Psychol 2012; 1: 33-40. https://doi.org/10.21307/sjcapp-2013-005
- Cooper M, Martin J, Langley K, Hamshere M, Thapar A. Autistic traits in children with ADHD index clinical and cognitive problems. Eur Child Adolesc Psychiatry 2014; 23: 23-34. https://doi.org/10.1007/s00787-013-0398-6
- Joshi G, DiSalvo M, Faraone SV, et al. Predictive utility of autistic traits in youth with ADHD: a controlled 10-year longitudinal follow-up study. Eur Child Adolesc Psychiatry 2020; 29: 791-801. https://doi.org/10.1007/s00787-019-01384-8
- Kotte A, Joshi G, Fried R, et al. Autistic traits in children with and without ADHD. Pediatrics 2013; 132: e612-e622. https://doi.org/10.1542/peds.2012-3947
- Biederman J, Fitzgerald M, Faraone SV, Fried R, Woodworth KY, Saunders A, et al. Are autistic traits in youth meaningful? A replication study in non-referred siblings of youth with and without attention-deficit/hyperactivity disorder. Scand J Child Adolesc Psychiatr Psychol 2015; 4: 77-87. https://doi.org/10.21307/sjcapp-2016-012
- Thompson RA. Emotion regulation: a theme in search of definition. Monogr Soc Res Child Dev 1994; 59: 25-52.
- Soler-Gutiérrez AM, Pérez-González JC, Mayas J. Evidence of emotion dysregulation as a core symptom of adult ADHD: a systematic review. PLoS One 2023; 18: e0280131. https://doi.org/10.1371/journal.pone.0280131
- Biederman J, Spencer TJ, Petty C, et al. Longitudinal course of deficient emotional self-regulation CBCL profile in youth with ADHD: prospective controlled study. Neuropsychiatr Dis Treat 2012; 8: 267-276. https://doi.org/10.2147/NDT.S29670
- Windle G. What is resilience? A review and concept analysis. Reviews in Clinical Gerontology 2011; 21: 152-169. https://doi.org/10.1017/S0959259810000420
- Regalla MA, Guilherme P, Aguilera P, Serra-Pinheiro MA, Mattos P. Attention deficit hyperactivity disorder is an independent risk factor for lower resilience in adolescents: a pilot study. Trends Psychiatry Psychother 2015; 37: 157-160. https://doi.org/10.1590/2237-6089-2015-0010
- Shi M, Liu L, Sun X, Wang L. Associations between symptoms of attention-deficit/ hyperactivity disorder and life satisfaction in medical students: the mediating effect of resilience. BMC Med Educ 2018; 18: 164. https://doi.org/10.1186/s12909-018-1261-8
- Dangmann CR, Skogli GKW, Holthe MEG, Steffenak AKM, Andersen PN. Life gets better: important resilience factors when growing up with ADHD. J Atten Disord 2024; 28: 1198-1209. https://doi.org/10.1177/10870547241246645
- Schei J, Nøvik TS, Thomsen PH, Lydersen S, Indredavik MS, Jozefiak T. What predicts a good adolescent to adult transition in ADHD? The role of self-reported resilience. J Atten Disord 2018; 22: 547-560. https://doi.org/10.1177/1087054715604362
- Barkley RA, Fischer M. The unique contribution of emotional impulsiveness to impairment in major life activities in hyperactive children as adults. J Am Acad Child Adolesc Psychiatry 2010; 49: 503-513. https://doi.org/10.1097/00004583-201005000-00011
- Shakeshaft A, Heron J, Blakey R, et al. Co-development of attention deficit hyperactivity disorder and autistic trait trajectories from childhood to early adulthood. J Child Psychol Psychiatry 2023; 64: 1596-1607. https://doi.org/10.1111/jcpp.13851
- Unal D, Unal MF, Alikasifoglu M, Cetinkaya A. Genetic variations in attention deficit hyperactivity disorder subtypes and treatment resistant cases. Psychiatry Investig 2016; 13: 427-433. https://doi.org/10.4306/pi.2016.13.4.427
- Kaufman J, Birmaher B, Brent D, et al. Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry 1997; 36: 980-988. https://doi.org/10.1097/00004583-199707000-00021
- Ünal F, Öktem F, Çetin Çuhadaroğlu F, et al. Reliability and validity of the schedule for affective disorders and schizophrenia for school-age children-present and lifetime version, DSM-5 November 2016-Turkish adaptation (K-SADS-PL-DSM-5-T). Turk Psikiyatri Derg 2019; 30: 42-50.
- Constantino JN, Davis SA, Todd RD, et al. Validation of a brief quantitative measure of autistic traits: comparison of the social responsiveness scale with the autism diagnostic interview-revised. J Autism Dev Disord 2003; 33: 427-433. https://doi.org/10.1023/a:1025014929212
- Ünal S, Güler AS, Dedeoğlu C, Taşkın B, Yazgan Y. Dikkat eksikliği hiperaktivite bozukluğu tanısı olan klinik örneklemde sosyal karşılıklılık: Okul örnekleminden elde edilen kontrol grubu ile karşılaştırma. In: 19. Ulusal Çocuk ve Ergen Ruh Sağlığı ve Hastalıkları Kongresi, Hatay, Türkiye, 2009: 204.
- Liebenberg L, Ungar M, LeBlanc JC. The CYRM-12: a brief measure of resilience. Can J Public Health 2013; 104: e131-e135. https://doi.org/10.1007/BF03405676
- Arslan G. Psychometric properties of child and youth resilience measure (CYRM-12): the study of reliability and validity. Ege Journal of Education 2015; 16: 1-12.
- Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology and Behavioral Assessment 2004; 26: 41-54. https://doi.org/10.1023/b:joba.0000007455.08539.94
- Ruganci RN, Gençöz T. Psychometric properties of a Turkish version of the difficulties in emotion regulation scale. J Clin Psychol 2010; 66: 442-455. https://doi.org/10.1002/jclp.20665
- Epstein NB, Baldwin LM, Bishop DS. The McMaster family assessment device. Journal of Marital and Family Therapy 1983; 9: 171-180. https://doi.org/10.1111/j.1752-0606.1983.tb01497.x
- Bulut I. Aile değerlendirme ölçeği el kitabı. Ankara: Özgüzeliş Matbaası; 1990.
- Hollingshead AB, Redlich FC. Social class and mental illness: a community study. 1958. Am J Public Health 2007; 97: 1756-1757. https://doi.org/10.2105/ajph.97.10.1756
- Guy W. Clinical global impressions scale. APA PsycTests 1976. https://doi.org/10.1037/t48216-000
- Endicott J, Spitzer RL, Fleiss JL, Cohen J. The global assessment scale. A procedure for measuring overall severity of psychiatric disturbance. Arch Gen Psychiatry 1976; 33: 766-771. https://doi.org/10.1001/archpsyc.1976.01770060086012
- Biederman J, Petty CR, Evans M, Small J, Faraone SV. How persistent is ADHD? A controlled 10-year follow-up study of boys with ADHD. Psychiatry Res 2010; 177: 299-304. https://doi.org/10.1016/j.psychres.2009.12.010
- Di Lorenzo R, Balducci J, Poppi C, et al. Children and adolescents with ADHD followed up to adulthood: a systematic review of long-term outcomes. Acta Neuropsychiatr 2021; 33: 283-298. https://doi.org/10.1017/neu.2021.23
- Chan E, Fogler JM, Hammerness PG. Treatment of attention-deficit/hyperactivity disorder in adolescents: a systematic review. JAMA 2016; 315: 1997-2008. https://doi.org/10.1001/jama.2016.5453
- Kolar D, Keller A, Golfinopoulos M, Cumyn L, Syer C, Hechtman L. Treatment of adults with attention-deficit/hyperactivity disorder. Neuropsychiatr Dis Treat 2008; 4: 389-403. https://doi.org/10.2147/ndt.s6985
- Katzman MA, Bilkey TS, Chokka PR, Fallu A, Klassen LJ. Adult ADHD and comorbid disorders: clinical implications of a dimensional approach. BMC Psychiatry 2017; 17: 302. https://doi.org/10.1186/s12888-017-1463-3
- Kuriyan AB, Pelham WE, Molina BS, et al. Young adult educational and vocational outcomes of children diagnosed with ADHD. J Abnorm Child Psychol 2013; 41: 27-41. https://doi.org/10.1007/s10802-012-9658-z
- Young S, Gudjonsson G, Chitsabesan P, et al. Identification and treatment of offenders with attention-deficit/hyperactivity disorder in the prison population: a practical approach based upon expert consensus. BMC Psychiatry 2018; 18: 281. https://doi.org/10.1186/s12888-018-1858-9
- Chan ES, Groves NB, Marsh CL, Miller CE, Richmond KP, Kofler MJ. Are there resilient children with ADHD? J Atten Disord 2022; 26: 643-655. https://doi.org/10.1177/10870547211025629
- Charabin E, Climie EA, Miller C, Jelinkova K, Wilkins J. “I’m Doing Okay”: strengths and resilience of children with and without ADHD. J Atten Disord 2023; 27: 1009-1019. https://doi.org/10.1177/10870547231167512
- Alvord MK, Grados JJ. Enhancing resilience in children: a proactive approach. Professional Psychology: Research and Practice 2005; 36: 238. https://doi.org/10.1037/0735-7028.36.3.238
- Reed P, Giles A, Gavin M, Carter N, Osborne LA. Loneliness and social anxiety mediate the relationship between autism quotient and quality of life in university students. Journal of Developmental and Physical Disabilities 2016; 28: 723-733. https://doi.org/10.1007/s10882-016-9504-2
- Capp SJ, Agnew-Blais J, Lau-Zhu A, et al. Is quality of life related to high autistic traits, high ADHD traits and their Interaction? Evidence from a young-adult community-based twin sample. J Autism Dev Disord 2023; 53: 3493-3508. https://doi.org/10.1007/s10803-022-05640-w
- Troy AS, Willroth EC, Shallcross AJ, Giuliani NR, Gross JJ, Mauss IB. Psychological resilience: an affect-regulation framework. Annu Rev Psychol 2023; 74: 547-576. https://doi.org/10.1146/annurev-psych-020122-041854
- Silvers JA. Adolescence as a pivotal period for emotion regulation development. Curr Opin Psychol 2022; 44: 258-263. https://doi.org/10.1016/j.copsyc.2021.09.023
- Posner J, Kass E, Hulvershorn L. Using stimulants to treat ADHD-related emotional lability. Curr Psychiatry Rep 2014; 16: 478. https://doi.org/10.1007/s11920-014-0478-4
- Coghill DR, Rhodes SM, Matthews K. The neuropsychological effects of chronic methylphenidate on drug-naive boys with attention-deficit/hyperactivity disorder. Biol Psychiatry 2007; 62: 954-962. https://doi.org/10.1016/j.biopsych.2006.12.030
- Childress AC, Arnold V, Adeyi B, et al. The effects of lisdexamfetamine dimesylate on emotional lability in children 6 to 12 years of age with ADHD in a double-blind placebo-controlled trial. J Atten Disord 2014; 18: 123-132. https://doi.org/10.1177/1087054712448252
- Rösler M, Retz W, Fischer R, et al. Twenty-four-week treatment with extended release methylphenidate improves emotional symptoms in adult ADHD. World J Biol Psychiatry 2010; 11: 709-718. https://doi.org/10.3109/15622971003624197
- Reimherr FW, Williams ED, Strong RE, Mestas R, Soni P, Marchant BK. A double-blind, placebo-controlled, crossover study of osmotic release oral system methylphenidate in adults with ADHD with assessment of oppositional and emotional dimensions of the disorder. J Clin Psychiatry 2007; 68: 93-101. https://doi.org/10.4088/jcp.v68n0113
Copyright and license
Copyright © 2025 The Author(s). This is an open access article distributed under the Creative Commons Attribution License (CC BY), which permits unrestricted use, distribution, and reproduction in any medium or format, provided the original work is properly cited.