Abstract
Aim. This study aimed to describe barriers and facilitators of the adherence of children with human immunodeficiency virus (HIV) to antiretroviral therapy (ART) from the perspectives of their caregivers.
Methods. In-depth interviews were held with the caregivers of 15 children. The collected data were analyzed using thematic analysis procedures. The Consolidated Criteria for Reporting Qualitative Research (COREQ) were followed in the study.
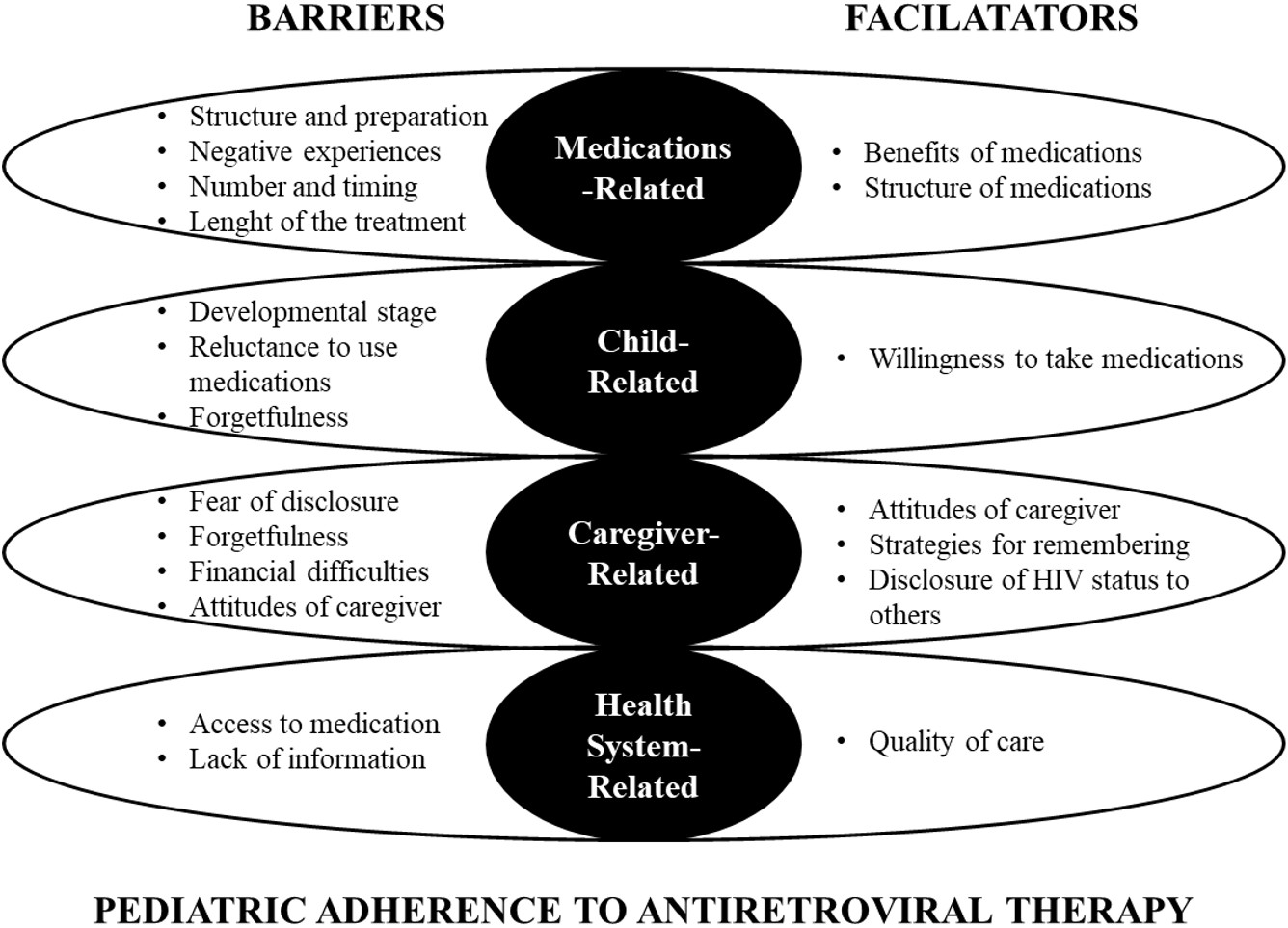
Results. The perspectives of caregivers were categorized under four themes and subthemes. Barriers and facilitators of the adherence of children with HIV to ART were categorized into 4 main themes: (1) medication-related, (2) child-related, (3) caregiver-related, and (4) health system-related. The results indicated that understanding the factors that influence pediatric ART adherence is critical to the development of adequate strategies. In addition, disclosure of HIV status to the child is also an important factor affecting drug administration in the social environment.
Conclusions. To ensure adherence to lifelong ART, targeted caregiver support through continuous supervision, clear guidance on drug preparation, and strategies for effective administration should be integrated into context-specific interventions that address the combined influence of factors related to the child, medication, healthcare, and of the sociocultural environment.
Keywords: antiretroviral therapy, adherence, children, barriers, facilitators, human immunodeficiency virus (HIV)
Introduction
Human immunodeficiency virus (HIV) continues to affect millions of people worldwide. According to UNICEF (2023), an estimated 39 million individuals were living with HIV in 2022, including 2.58 million children and adolescents under the age of 19.1 In Türkiye, the number of individuals diagnosed with HIV has been progressively increasing each year.2 To prevent acquired immune deficiency syndrome (AIDS), antiretroviral therapy (ART) should be provided effectively, and the individual’s adherence to treatment should be at a rate of 95-100%.3,4 Adherence to ART decreases drug resistance, reduces the risk of HIV transmission, lowers HIV-related morbidity rates, and improves the patient’s quality of life.3,5-7 A child’ s adherence to ART is a significant challenge for caregivers because it is influenced by many factors that make it easier or more complex8 such as the child’s behavior, the tolerability of medications, the quality of health services, the disclosure of HIV status, and the fear of stigma.9-11 To understand the barriers to and facilitators of ART adherence in children is essential for achieving the Sustainable Development Goals (SDGs), especially SDG #3: Good health and well-being (United Nations, n.d.).12
Despite the increase in the number of children diagnosed with HIV in Türkiye2, current studies on ART compliance are limited to adults.13-15 Therefore, this study aimed to identify barriers to and facilitators of children’s adherence to ART from the perspectives of caregivers in Türkiye.
Material and Methods
Study design
A phenomenological qualitative research approach was used in this study. The authors followed the COREQ Checklist to ensure accurate and complete reporting.16
Settings and participants
From November 2022 to January 2023, we conducted semi-structured interviews with caregivers of children and adolescents on ART at a Pediatric Infectious Diseases Clinic of İstanbul University Hospital in Istanbul. A purposive sampling method was used to identify participants. Eligible caregivers were responsible for the primary care of pediatric patients diagnosed with HIV and on ART for at least 3 months, and voluntarily agreed to participate in the study. Three researchers (AD, NMA, ED) contacted the participants by phone, explaining the purpose of the study and asking whether they would like to participate in the study. The term used in this study, “participant”, refers to caregivers.
Data collection
An in-depth interview method was employed to collect the data by using a semi-structured interview form. This open-ended interview questionnaire was developed by the researcher team based on the relevant literature.17-19 Examples of the questions that were used are shown in Table I.
| Table I. Interview questions |
| Interview topic: Providing care to a child with HIV |
|
Questions: How has your child’s disease changed your life? How is your child's care going? What is the most difficult situation you have experienced in caring for your child? When you need support in this process, how do you get support? |
| Interview topic: Antiretroviral therapy |
|
Questions: How is your child's treatment going? Can you share your experiences regarding your child's treatment? How do you manage your child’s treatment regime? What types of difficulties do you experience with your child's treatment/use of medication? What do you think are the factors that make it easier or more difficult for your child to take medication? How did you find solutions? |
Each interview was audio-recorded and lasted 30-45 minutes. One of the authors, with prior experience in in-depth interviews (ÖŞ), conducted the face-to-face interviews in the outpatient clinic room with only the interviewer and the participant present. Privacy was ensured by giving an anonymous ID.
Data analysis
The recordings were transcribed verbatim by one of the researchers (ÖŞ). The data were analyzed using the six-step thematic analysis method.20 At the beginning of the data analysis process, two researchers (ÖŞ, AA) independently listened to the audio recordings and checked the transcripts for corrections for any mistakes. This was to assure methodological accuracy and ensure that the transcripts correctly expressed the statements of the participants. Once the raw data were gathered, three researchers (ÖŞ, AA, SB) independently created their codes and themes by reading the raw data. Then, they came together and identified the similarities and differences between the themes and subthemes they determined through codes. The researchers utilized code meanings and code frequencies to assess data saturation.21 After 15 caregivers were interviewed, it was determined that there was no new code, the data reached the saturation point, it was decided that the data were sufficient, and no more interviews were held. The transcripts were sent to the researchers participating in the study (AS, ND, NMA, ED , SHT) for their opinions and recommendations, and the final revision was made. Each author provided final approval for the publication of this version and agreed to be considered accountable for all aspects of the work.
Ethical considerations
The study was conducted in accordance with the Declaration of Helsinki, and the study was approved by the İstanbul University’s Social Sciences Ethics Review Board (1109334/22.08.2022). Additionally, institutional permission was obtained before the study. Before the interview, informed consent was taken from all participants for participation to the research and record audio of interviews. Due to the sensitive nature of the research topic, before each interview, the researcher reminded the participants that participation was voluntary and that they could cease participation at any time during the interview.
Results
The study analyzed data from 15 participants. Table II summarizes the sociodemographic characteristics of the participants and the pediatric patients they cared for. Qualitative analysis results are presented as themes and subthemes below and in Fig. 1.
| F: female, HIV: human immunodeficiency virus, M: male, mo: months, yr: years. | |||||||||
| Table II. Sociodemographic characteristics of caregivers and pediatric patients | |||||||||
|
|
|
||||||||
| Gender | Age (yr) | Level of education | HIV status | Relation to child | Age | Sex | Route of infection | Time since treatment initiation | |
| P-1 | F | 37 | University | Positive | Mother | 16 yr | F | Perinatal | 15 yr |
| P-2 | F | 22 | High school | Positive | Mother | 42 mo | M | Perinatal | 30 mo |
| P-3 | F | 43 | Primary-secondary school | Positive | Mother | 20 mo | F | Perinatal | 12 mo |
| P-4 | F | 38 | Primary-secondary school | Positive | Mother | 4 yr | M | Perinatal | 4 yr |
| P-5 | F | 53 | Primary-secondary school | Positive | Mother | 14 yr | M | Perinatal | 13 yr |
| P-6 | F | 46 | Primary-secondary school | Positive | Mother | 7 yr | M | Perinatal | 4 mo |
| P-7 | F | 45 | University | Negative | Legal guardian | 17 yr | M | Unknown | 26 mo |
| P-8 | M | 42 | University | Positive | Father | 5 yr | F | Perinatal | 4 yr |
| P-9 | F | 24 | University | Negative | Legal guardian | 16 yr | F | Unknown | 4 mo |
| P-10 | F | 27 | High school | Positive | Mother | 10 yr | M | Perinatal | 3 yr |
| P-11 | F | 58 | High school | Negative | Mother | 17 yr | M | Sexual | 18 mo |
| P-12 | F | 28 | Primary-secondary school | Positive | Mother | 5 yr | F | Perinatal | 5 yr |
| P-13 | F | 47 | Primary-secondary school | Negative | Mother | 17 yr | M | Blood transfusion | 9 yr |
| P-14 | F | 33 | Primary school | Positive | Mother | 42 mo | M | Perinatal | 30 mo |
| P-15 | F | 23 | High school | Positive | Mother | 30 mo | M | Perinatal | 30 mo |
Barriers to adherence to antiretroviral treatment
Theme 1: Medication-related barriers
From the perspectives of the participants, the ‘structure and preparation of drugs’, ‘negative experiences with medications’, and ‘the numbers and timing of medications’ were barriers to children’s adherence to ART.
Structure and preparation of drugs. The participants reported that they had difficulty in calculating the dose by snapping the tablets into smaller pieces (lopinavir + ritonavir/Kaletra®), and they stated that the long dissolution period of the drug prolonged its preparation time (10/15).
‘…but there is one called “Kaletra” (lopinavir + ritonavir/Kaletra®). We developed some methods at home because the drug is very hard to break. At first, we tried hitting it with a hammer or something, but it didn’t work. Then, my wife found something [some method].’ (P-8, father of 5-year-old girl)
Negative experiences with medicines. According to the statements of the participants, due to the bitter taste of the medicine, it was very difficult to administer, and their children started to feel nausea and vomiting as soon as they tasted it (9/15).
‘He immediately vomited after taking the medication, and I was nearby holding a bucket. He gets nauseous because it tastes so bad.’ (P-14, mother of 3.5-year-old boy)
Numbers and timing of medications. The participants stated that the number of medications was too much, and therefore, they had difficulty in arranging medication times at occasions such as before going to bed or school (6/15).
‘He takes a lot of medications. When he goes to school in the morning, I give him the medication to take [there]. He can’t have breakfast because he goes early. ... I tell him you must take it at this time, but he could skip it [without my knowledge].’ (P-5, mother of 15-year-old boy)
‘...if he was very sleepy that day and was very tired. There were times when I couldn’t give him the medicine because he was too sleepy.’ (P-4, mother of 4-year-old boy)
Length of the treatment. The participants emphasized that taking drugs continuously and coming to the hospital often for treatment caused boredom in children (2/15).
‘He is upset because he is constantly being treated. He regularly gives blood tests… He is tired. He doesn’t want to go anymore.’ (P-10, mother of 10-year-old boy)
Theme 2: Child-related barriers
Based on the statements of the participants, the ‘child’s developmental stage’, ‘forgetfulness’, and ‘unwillingness to take medication’ were found to negatively affect children’s compliance with ART.
Child’s developmental stage. It was determined that children had different behaviours that made medication compliance difficult according to their developmental stage. The participants reported that young children ran away when they saw the medicine, while preschool children asked why they were taking the medicine (6/15).
‘He immediately hides when he sees me holding the medication. I must give it to him regularly. It was and is hard...’ (P-15, mother of 2.5-year-old boy)
‘We can’t explain it because he is very young. He says, mom, other children don’t take [medication] every day.’ (P-4, mother of 4-year-old boy)
Reluctance to use medicine. The participants revealed that children expressed reluctance to take medication when they felt better and asked why they had to continue using the medicine (5/15).
‘If I give him the boxes of medicine, he knows all of them, he can take them, but sometimes he says that’s enough. He says he doesn’t have anything [of concern in terms of health]. …especially when he feels much better, he says, he’s no different from others.’ (P-7, legal guardian of a 17-year-old boy)
Forgetfulness. The participants said that their children’s treatment was disrupted due to forgetfulness (3/15).
‘This one is very forgetful, extremely forgetful. I even recall him not taking his medication for a week…’ (P-11, mother of 17-year-old boy)
Theme 3: Caregiver-related barriers
From the perspectives of the participants, the ‘fear of disclosure’, ‘caregiver’s attitude’, and ‘forgetting and financial difficulties’ were associated with children’s adherence to ART.
Fear of disclosure. It was revealed that most of the participants did not disclose the diagnosis to their child or other relatives. They reported that they hid the medicine and removed the labels from the boxes, especially when they went on a vacation or had guests because they were concerned about stigma (13/15).
‘… the only difficulty we have is that we don’t tell anyone. When someone comes to our house, we always hide all the medicine, we take out the boxes, labels, etc. just in case they accidentally see them. Sometimes, when we visit our friends or relatives, we can’t give [our child] the medicine there either.’ (P-8, father of 5-year-old girl)
Forgetfulness. The participants stated that they had a lot of responsibilities because they had to take care of household chores and their other children, and they occasionally forgot to give their child medication (5/15).
‘…I have to attend to my other child. I forget about it [administering medication], I am dealing with other things, sometimes I forget.’ (P-14, mother of 3.5-year-old boy)
Financial difficulties. Although the medicines they used were free of charge, the participants stated that in some cases, they had to pay a fee (4/15).
‘They have pills there but not syrup. I purchase the syrup from abroad. It’s a bit expensive, let’s say four bottles, 800 euros, they last for three months (Lopinavir/ritonavir, syrup). So, [I purchase it] as long as I can...’ (P-2, mother of 42-month-old boy)
Attitudes of caregivers. According to the participants, they often had difficulties in the treatment of their children; some participants tried hard and used different methods to give their children the medication, while some gave up when they were unable to have their children take the medicine (1/15).
‘He doesn’t take [the medicine] in any way, I mean, I’ve tried in every way. I’ve given up these days.’ (P-2, mother of 42-month-old boy)
Theme 4: Healthcare system-related barriers
The participants stated that ‘access to medication’ and ‘lack of information’ were barriers to their children’s adherence to ART.
Access to medication. It was determined that the participants had problems in access to drugs that were prescribed with a medical report and that were available free of charge from pharmacies (4/15).
‘It’s been a week since we were able to get the tablet. There was a problem with the medical report.’ (P-6, mother of 7-year-old boy)
Lack of information. The participants stated that they had received insufficient information about the preparation steps of medicines, such as how to calculate the dose and how to administer it (4/15).
‘At first, we had a very hard time. Then we talked to the doctor, and he said you can put it in her formula. I had already found this on my own (this method) and I could not give it in any other way.’ (P-3, mother of 20-month-old girl)
Facilitators of Adherence to Antiretroviral Treatment
Theme 1: Medication-related facilitators
It was determined that for the participants, ‘benefits of medication’ and ‘the structure of medicines’ facilitated the compliance of their children with ART.
Benefits of medication. The participants stated that they observed the positive effects of the medication and that these effects were influential in their administration of the medication to children regularly (5/15).
‘There’s no problem if he takes the medicine. He needs to take the medicine for his survival and immunity.’ (P-11, mother of 17-year-ol boy)
Structure of drugs. It was found that the children of the participants found it easier to take drugs in the form of syrups compared to tablets (2/15).
‘There is no difficulty with syrups. She already has [other] syrups with a spoon, there is no problem with syrups.’ (P-3, mother of 20-month-old girl)
Theme 2: Child-related facilitators
Willingness to take medication. Some participants stated that their children were used to the treatment and were willing to take their medication (2/15).
‘...it’s very bitter, but she got used to it, and now she takes the medicine herself.’ (P-8, father of 5-year-old girl)
Theme 3: Caregiver-related facilitators
Caregiver-related facilitators were identified as ‘caregiver’s attitudes’, ‘strategies for remembering’, and ‘disclosure of HIV status to others.’
Attitudes of the caregiver. It was stated by the participants that they had a lot of difficulties while administering the medication, but most of them had their children take the medication even if they had to persuade them to take it (7/15).
‘I say to him, if he doesn’t take the medicine, I would turn off the cartoon [on TV]’ (P-14, mother of 42-month-old boy)
Strategies for remembering. Some participants reported that they used some strategies to have their children take their medication (4/15).
‘We set an alarm on the phone, otherwise, we forget.’ (P-13, mother of 17-year-old boy)
‘You know, if I go somewhere, I always carry my spares in my bag in case the schedule is disrupted. In case I need to go somewhere urgently, I immediately grab it before leaving.’ (P-3, mother of 20-month-old girl)
Disclosure of HIV status to others. The participants who disclosed the HIV diagnosis of their children stated that they received support from their close relatives in the treatment of their children (2/15).
‘He doesn’t take his medicine with anyone else. Either with me or with my brother. My mom, my brother, my whole family, they all support me.’ (P-2, mother of 42-month-old boy)
Theme 4: Healthcare system-related facilitators
Quality of care. Some participants expressed their view that they were satisfied with the quality of service they received, and their children were well cared for (3/15).
‘The healthcare workers here are very good. God bless them all. They are very protective. Like a family.’ (P-10, mother of 10-year-old boy)
Discussion
This study explores the barriers and facilitators to pediatric ART adherence in Türkiye, highlighting caregivers’ challenges and the need for targeted interventions.
Barriers to adherence
Medication-related barriers were the most frequently stated barriers by the participants. Since the children had difficulty taking the drugs in pill form, they were more exposed to their bitter taste and thus experienced nausea and vomiting. The participants of this study often tried to disguise the bitter taste of medicines by mixing them with other foods, which was similar to other methods mentioned in previous studies22, but children still have negative experiences with ART, such as nausea and vomiting. Our results, as in previous studies, showed that factors leading to difficulties in drug administration such as drug size17,23, negative experiences including side effects8,17,23,24, the numbers and timing of taking medication17,23 affect children’s adherence to ART. Similar to the results of studies with adolescents, activities of daily living, such as school or sleep prevented adolescents from taking their medication at the right time.18 Therefore, long treatment durations may cause fatigue and boredom in children.8,17,25
The World Health Organization (WHO) has consistently revised its treatment protocols for individuals living with HIV in response to emerging evidence and clinical needs. In line with these efforts, the Paediatric Drug Optimization (PADO) initiative was launched in 2013 to establish strategic priorities for the development of antiretroviral therapies tailored to children.26 This initiative has substantially contributed to the advancement of several high-priority pediatric ART formulations, including dispersible fixed-dose combinations (FDC) and long active injectable options. However, these formulations of dispersible FDCs remain largely inaccessible in many low- and middle-income countries (LMICs), including Türkiye.27 The United States Food and Drug Administration (FDA) approved cabotegravir–rilpivirine (CAB/RPV) in 2021 as the first long-acting injectable treatment for adults living with HIV.28 However, the development of such injectable therapies has also been identified as a long-term priority under the PADO-3 framework.29 Children have difficulty taking oral medications, especially tablets, due to factors such as taste, smell, and the need for daily intake, which negatively affects medication adherence. Therefore, it is argued that long-acting injectable therapies should also be prioritized within pediatric HIV treatment research.
This gap between global drug development and local availability becomes particularly problematic during the formulation of individualized treatment plans for children. For example, lopinavir/ritonavir (LPV/r), one of the very few ART currently available in a liquid formulation for children, has been reported to have poor palatability in the literature30,31; however, one caregiver in our study stated that they were unable to administer the tablet form to their child and therefore resorted to obtaining the syrup formulation from abroad at a high cost. Therefore, ART regimens should be individualized, and access to appropriate pediatric drug formulations must be improved. If palatable options are not available, caregivers should be supported with strategies to increase children’s compliance with unpleasant-tasting medications, such as numbing the taste with ice chips or masking the taste with sweet or tangy foods.30
The developmental stage of a child affects their behaviors of adherence to ART. Similar with our results, caregivers have reported that children aged 1-4 years refuse and avoid medication during administration whereas preschool children inquire as to why they are taking medication.23,32 According to the participants of our study, adolescents who knew their diagnosis but were not fully informed were reluctant to take their medication, especially when they were asymptomatic or felt well. This is thought to be closely related to the explanation of the diagnosis. Recent studies have shown that the disclosure of HIV status to adolescents and the closest members of the family plays an important role in improving medication adherence.9-11,33 The disclosure of HIV status to children helps them better understand their need to adhere to their medication regimen.5,9,10,18 Nevertheless, HIV and AIDS are still taboo in Türkiye, and they are perceived as fatal. Thus, parents may be unwilling to disclose this condition to their children and other family members. This is also supported by the fact that sexual relationships are one of the transmission routes of HIV, and sexuality is not yet a topic that is easily discussed in Turkish society.
Caregivers may experience self-stigma when they internalize the societal stigma toward people living with HIV, which can lead to feelings of guilt and shame. These emotions may result in withdrawal from social environments, delaying taking or giving medication in front of family members or friends, avoiding seeking support, and eventually becoming socially isolated. Consistent with previous research, our results showed that caregivers removed medication labels, skipped doses, or inadvertently missed medication times for fear of disclosure or stigmatization.22 Disruptions in medication regimens are known to negatively affect adherence to ART.3,5,34 Although this study did not include clinical data such as viral load measurements or drug resistance testing, the adherence-related challenges reported by caregivers such as fear of stigma and lack of social support and emotional distress are known to contribute to poor treatment outcomes. Previous mixed-method studies have shown that similar psychosocial and structural barriers can lead to virological failure and increase the risk of drug resistance in pediatric and adolescent populations living with HIV.35,36
The barriers related to the health system were stated by the participants of this study as delays in the electronic system for accessing drugs for free and their lack of information counseling on drug preparation. Drug reports and the pharmacy system need to be synchronized to avoid delays in accessing these drugs. Otherwise, treatment may be interrupted, and parents may have to purchase these medications and experience financial difficulties. Additionally, combined antiretroviral therapies may contribute to stock-outs and pose challenges for treatment adherence in young children.27 However, beyond adherence, access to these medications is a fundamental right for children. Therefore, it is essential for health systems to develop proactive strategies that can anticipate and address delays in electronic systems or stock-out situations. Previous studies have suggested that lack of access and inadequate counseling on the use of medications negatively affect compliance with treatment.3,18,22
Facilitators of adherence
According to the results of this study, the themes that facilitated children’s adherence to ART varied. Medication-related facilitators included the caregiver’s observation of the benefits of ART on children and the syrup form. The benefits of ART are known to positively affect children’s adherence to treatment.35 The observation of the positive effects of drugs on children is thought to be a source of motivation for caregivers to continue their children’s treatment regularly.37 Secondly, although it is known that the syrup form of drugs is an important factor in treatment compliance in terms of taste and easy administration23 very few children were able to access syrup forms in Türkiye because these forms were not covered by the healthcare system. This also posed financial challenges as a barrier for parents in ensuring their children’s adherence to ART. It is vital to facilitate access to the syrup form of ART and improve the taste and size of pills so that children can take them easily. Considering all the barriers and facilitators related to medication, one of the most important interventions to facilitate adherence to ART is access to the syrup form.
Many studies have reported the importance of caregiver support for optimal ART adherence.10,11,19,38,39 Consistent with previous results, caregivers made sure that their children adhered to treatment by persuasion or bargaining. Moreover, caregiver strategies such as reminders of medication time, setting an alarm, or carrying a spare bag facilitated adherence to ART in both young children and adolescents.17,18 During clinic visits, frequent reminders provided to caregivers about the routine use of techniques such as setting alarms to remember medication times or carrying spare bags may positively affect children’s adherence to ART.
As mentioned earlier, some caregivers of children whose treatment was followed up in the same clinic reported the quality of health services as a facilitator, while some caregivers reported their lack of information about the health system as a barrier to their children’s adherence to ART. This finding suggested that children and caregivers followed in the same clinic may not benefit from the same quality of care. Previous studies have shown that family-centered care help improve adherence to ART.3,10
Strengths and limitations
This study includes data based on the self-reports of caregivers. The possibility of bias in parental/caregiver statements constitutes a limitation of our study. In terms of the generalizability of the results, our sample represented a small group of 15 caregivers from a single urban center, which limits the transferability of findings to rural settings or diverse healthcare institutions across Türkiye. Additionally, the study did not examine how intersecting social determinants such as maternal age, education, economic status collectively influence adherence, which may be better addressed in future research. The strength of our study is that it is the first study to our knowledge, conducted in Türkiye to investigate the situations that facilitate and complicate the adherence of children to ART from the perspectives of their caregivers. Our study also sheds light on the experiences of caregivers regarding children’s adherence to ART in Türkiye.
Conclusion and recommendations
Adherence to ART in the pediatric population is a complex and dynamic process. Caregivers identified more barriers than facilitators to children’s adherence to ART, with the most significant barriers related to negative experiences and medication forms. Factors such as the child’s developmental stage and the disclosure status of the diagnosis to the child or their environment also played a critical role. Not disclosing the diagnosis to the child often leads to uncertainty and reluctance about treatment, while withholding the diagnosis from the community can disrupt medication schedules due to challenges in administering medication in social settings. These findings highlight the need to further investigate adolescents’ self-perceptions of HIV and ART, particularly in relation to disclosure and treatment autonomy. Caregivers, as central figures in managing pediatric HIV treatment, face significant difficulties in ensuring adherence. Health professionals, in their educator role, should provide targeted support to caregivers, offering strategies to address these challenges and improve medication administration. Effective treatment efforts must consider the interconnected influences of the child, caregiver(s), medication regimens, healthcare system, and sociocultural factors. Further research is essential to explore pediatric adherence to ART in Türkiye, particularly using larger, more diverse samples, to develop comprehensive and context-specific interventions. Employing mixed-methods designs could further enrich findings by integrating in-depth qualitative insights with measurable adherence outcomes.
Acknowledgements
The authors acknowledge the staff of the Istanbul University Faculty of Medicine Hospital Pediatric Infectious Diseases Clinic in assistance in data and all caregivers for their participation.
Ethical approval
The study was approved by Istanbul University’s Social Sciences Ethics Review Board (1109334/22.08.2022). Additionally, institutional permission was obtained before the study. Before the interview, informed consent was taken from all participants for participation to the research and record audio of interviews. Due to the sensitive nature of the research topic, before each interview, the researcher reminded the participants that participation was voluntary and that they could cease participation at any time during the interview.
Source of funding
The authors declare the study received no funding.
Conflict of interest
The authors declare that there is no conflict of interest.
References
- United Nations Children’s Fund (UNICEF). Global and regional trends. 2023. Available at: https://data.unicef.org/topic/hivaids/global-regional-trends/ (Accessed on Dec 20, 2024)
- Republic of Türkiye Ministry of Health, General Directorate of Public Health, Department of Infectious Diseases and Early Warning. HIV/AIDS statistics. 2023. Available at: https://web.archive.org/web/20240331212302/https://hsgm.saglik.gov.tr/depo/birimler/bulasici-hastaliklar-ve-erken-uyari-db/Dokumanlar/Istatistikler/hiv-aids-2023.pdf
- Lin CJ, Cheng YI, Garvie PA, D’Angelo LJ, Wang J, Lyon ME. The effect of family-centered (FACE®) pediatric advanced care planning intervention on family anxiety: a randomized controlled clinical trial for adolescents with HIV and their families. J Fam Nurs 2020; 26: 315-326. https://doi.org/10.1177/1074840720964093
- Milward de Azevedo Meiners MM, Araújo Cruz I, de Toledo MI. Adherence to antiretroviral therapy and viral suppression: analysis of three periods between 2011 and 2017 at an HIV-AIDS center, Brazil. Front Pharmacol 2023; 14: 1122018. https://doi.org/10.3389/fphar.2023.1122018
- Bitwale NZ, Mnzava DP, Kimaro FD, Jacob T, Mpondo BC, Jumanne S. Prevalence and factors associated with virological treatment failure among children and adolescents on antiretroviral therapy attending HIV/AIDS care and treatment clinics in Dodoma municipality, central Tanzania. J Pediatric Infect Dis Soc 2021; 10: 131-140. https://doi.org/10.1093/jpids/piaa030
- Reif LK, Abrams EJ, Arpadi S, et al. Interventions to improve antiretroviral therapy adherence among adolescents and youth in low- and middle-income countries: a systematic review 2015-2019. AIDS Behav 2020; 24: 2797-2810. https://doi.org/10.1007/s10461-020-02822-4
- Vreeman RC, Ayaya SO, Musick BS, et al. Adherence to antiretroviral therapy in a clinical cohort of HIV-infected children in East Africa. PLoS One 2018; 13: e0191848. https://doi.org/10.1371/journal.pone.0191848
- Martelli G, Antonucci R, Mukurasi A, Zepherine H, Nöstlinger C. Adherence to antiretroviral treatment among children and adolescents in Tanzania: comparison between pill count and viral load outcomes in a rural context of Mwanza region. PLoS One 2019; 14: e0214014. https://doi.org/10.1371/journal.pone.0214014
- Amankwah-Poku M, Klutsey DA, Asante KO. Disclosure and health-related outcomes among children living with HIV and their caregivers. AIDS Res Ther 2021; 18: 13. https://doi.org/10.1186/s12981-021-00337-z
- Khumalo PN, Katirayi L, Ashburn K, et al. ‘There are no more secrets’: acceptability of a family-centered model of care for HIV positive children in Eswatini. BMC Health Serv Res 2020; 20: 951. https://doi.org/10.1186/s12913-020-05810-5
- Mengesha MM, Ajema D, Teshome A, Tura AK. The association between diagnosis disclosure and adherence to antiretroviral therapy among adolescents living with HIV in sub-Saharan Africa: a protocol for systematic review and meta-analysis. Syst Rev 2020; 9: 160. https://doi.org/10.1186/s13643-020-01420-8
- United Nations. Sustainable development goals. Available at: https://www.un.org/sustainabledevelopment/health/ (Accessed on Dec 20, 2024)
- Başoğlu S, Polat Ü, Güngör C. Self management in HIV / AIDS. University of Health Sciences Journal of Nursing 2020; 2: 183-190. https://doi.org/10.48071/sbuhemsirelik.696645
- Ceylan E, Koç A, İnkaya AÇ, Ünal S. Determination of medication adherence and related factors among people living with HIV/AIDS in a Turkish university hospital. Turk J Med Sci 2019; 49: 198-205. https://doi.org/10.3906/sag-1802-137
- Kalkan İA, Karaşahin Ö, Tuba DAL, et al. Does effective education intervention affects HIV patients compliance independently from drug posology? Dicle Med J 2019; 46: 789-797. https://doi.org/10.5798/dicletip.661385
- Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care 2007; 19: 349-357. https://doi.org/10.1093/intqhc/mzm042
- Ammon N, Mason S, Corkery JM. Factors impacting antiretroviral therapy adherence among human immunodeficiency virus-positive adolescents in Sub-Saharan Africa: a systematic review. Public Health 2018; 157: 20-31. https://doi.org/10.1016/j.puhe.2017.12.010
- Audi C, Jahanpour O, Antelman G, et al. Facilitators and barriers to antiretroviral therapy adherence among HIV-positive adolescents living in Tanzania. BMC Public Health 2021; 21: 2274. https://doi.org/10.1186/s12889-021-12323-1
- Galea JT, Wong M, Muñoz M, et al. Barriers and facilitators to antiretroviral therapy adherence among Peruvian adolescents living with HIV: a qualitative study. PLoS One 2018; 13: e0192791. https://doi.org/10.1371/journal.pone.0192791
- Braun V, Clarke V. Is thematic analysis used well in health psychology? A critical review of published research, with recommendations for quality practice and reporting. Health Psychol Rev 2023; 17: 695-718. https://doi.org/10.1080/17437199.2022.2161594
- Braun V, Clarke V. Thematic analysis. In: Cooper H, Camic PM, Long DL, Panter AT, Rindskopf D, Sher KJ, editors. APA handbook of research methods in psychology, Vol. 2. Research designs: Quantitative, qualitative, neuropsychological, and biological. American Psychological Association; 2012: 57-71. https://doi.org/10.1037/13620-004
- Coetzee B, Kagee A, Bland R. Barriers and facilitators to paediatric adherence to antiretroviral therapy in rural South Africa: a multi-stakeholder perspective. AIDS Care 2015; 27: 315-321. https://doi.org/10.1080/09540121.2014.967658
- Aston J, Wilson KA, Terry DR. The treatment-related experiences of parents, children and young people with regular prescribed medication. Int J Clin Pharm 2019; 41: 113-121. https://doi.org/10.1007/s11096-018-0756-z
- Abdela J, Assefa A, Shamele S. Prevalence of adverse drug reactions among pediatric patients on antiretroviral therapy in selected hospitals in Eastern Ethiopia: 8-year retrospective cross-sectional study. J Int Assoc Provid AIDS Care 2019; 18: 2325958218823208. https://doi.org/10.1177/2325958218823208
- Jjumba I, Kanyesigye M, Ndagijimana G, et al. Perceived barriers and facilitators to antiretroviral therapy adherence among youth aged 15-24 years at a regional HIV clinic in SouthWestern Uganda: a qualitative study. Afr Health Sci 2022; 22: 54-62. https://doi.org/10.4314/ahs.v22i2.7
- World Health Organization (WHO). Paediatric ARV drug optimization 2 meeting report, 8-9 December 2014. Available at: https://cdn.who.int/media/docs/default-source/hq-hiv-hepatitis-and-stis-library/pado2.pdf?sfvrsn=9ddd24e1_9 (Accessed on Apr 22, 2025).
- Kamphuis AE, Bamford A, Tagarro A, et al. Optimising paediatric HIV treatment: recent developments and future directions. Paediatr Drugs 2024; 26: 631-648. https://doi.org/10.1007/s40272-024-00656-4
- National Institutes of Health (NIH). FDA-approved HIV medicines. 2021. Available at: https://hivinfo.nih.gov/understanding-hiv/fact-sheets/fda-approved-hiv-medicines (Accessed on Apr 22, 2025).
- World Health Organization (WHO). Paediatric ARV drug optimization 3 review: summary report. 2018. Available at: https://iris.who.int/bitstream/handle/10665/272292/WHO-CDS-HIV-18.8-eng.pdf?sequence=1&isAllowed=y (Accessed on Apr 22, 2025).
- Clinicalinfo. Guidelines for the Use of antiretroviral agents in pediatric HIV infection. Available at: https://clinicalinfo.hiv.gov/en/guidelines/pediatric-arv/lopinavirritonavir (Accessed on Apr 22, 2025).
- Martinez BL, Riordan FA. Novel strategies in the use of lopinavir/ritonavir for the treatment of HIV infection in children. HIV AIDS (Auckl) 2010; 2: 59-67. https://doi.org/10.2147/hiv.s6616
- Mehta K, Ekstrand ML, Heylen E, Sanjeeva GN, Shet A. Adherence to antiretroviral therapy among children living with HIV in South India. AIDS Behav 2016; 20: 1076-1083. https://doi.org/10.1007/s10461-015-1207-7
- Kairania R, Onyango-Ouma W, Ondicho TG, Kigozi G. HIV status disclosure and antiretroviral therapy adherence among children in Masaka region, Uganda. Afr J AIDS Res 2022; 21: 251-260. https://doi.org/10.2989/16085906.2022.2060843
- van Elsland SL, Peters RPH, Grobbelaar C, et al. Disclosure of human immunodeficiency virus status to children in South Africa: a comprehensive analysis. South Afr J HIV Med 2019; 20: 884. https://doi.org/10.4102/sajhivmed.v20i1.884
- Ghanbari A, Khiaban MO, Sattari N, Kazemi AF. Adherence to antiretroviral therapy and its related factors among HIV-infected patients: a mixed-methods study. J Midwifery Reprod Health 2024; 12: 4299-4308. https://doi.org/10.22038/jmrh.2024.68680.2015
- Mukuku O, Govender K, Wembonyama SO. Barriers and facilitators to HIV viral load suppression among adolescents living with HIV in Lubumbashi, Democratic Republic of the Congo: a qualitative study. PLoS One 2025; 20: e0320417. https://doi.org/10.1371/journal.pone.0320417
- Abongomera G, Cook A, Musiime V, et al. Improved adherence to antiretroviral therapy observed among HIV-infected children whose caregivers had positive beliefs in medicine in Sub-Saharan Africa. AIDS Behav 2017; 21: 441-449. https://doi.org/10.1007/s10461-016-1582-8
- Paranthaman K, Kumarasamy N, Bella D, Webster P. Factors influencing adherence to anti-retroviral treatment in children with human immunodeficiency virus in South India-a qualitative study. AIDS Care 2009; 21: 1025-1031. https://doi.org/10.1080/09540120802612857
- Judd A, Melvin D, Thompson LC, et al. Factors associated with nonadherence to antiretroviral therapy among young people living with perinatally acquired HIV in England. J Assoc Nurses AIDS Care 2020; 31: 574-586. https://doi.org/10.1097/JNC.0000000000000171
Copyright and license
Copyright © 2025 The Author(s). This is an open access article distributed under the Creative Commons Attribution License (CC BY), which permits unrestricted use, distribution, and reproduction in any medium or format, provided the original work is properly cited.