Abstract
Background. Delirium in patients with ulcerative colitis may be seen, especially in the elderly and in patients hospitalized for a long time. In children, Wernicke’s encephalopathy may occur due to thiamine deficiency in both ulcerative colitis and Crohn’s disease. We present a patient with ulcerative colitis who presented with delirium as the first symptom, did not respond to steroid treatment and improved with anti-tumor necrosis factor-alpha treatment.
Case Presentation. A 14-year-old male child presented with complaints of nonsensical speech and hallucinations for two days. He also had 2-3 loose, non-bloody stools per day. Neurological examination was normal. There was no electrolyte abnormality or vitamin deficiency. The patient’s diarrhea gradually increased and became bloody, and was ultimately diagnosed with ulcerative colitis. The patient, who did not respond to steroid treatment, completely recovered with anti-tumor necrosis factor treatment.
Conclusions. We report a patient with ulcerative colitis who presented with delirium as the first symptom. The absence of electrolyte imbalance or vitamin deficiency in our patient suggests that inflammation is the cause of this condition. To the best of our knowledge, this is the first description of the relationship between inflammatory bowel disease and delirium in children.
Keywords: ulcerative colitis, delirium, children
Introduction
Inflammatory bowel diseases (IBD) are chronic inflammatory conditions affecting the digestive tract and are divided into two main groups: ulcerative colitis (UC) and Crohn’s disease (CD). IBDs may also affect extraintestinal organs such as joints, eyes, mouth and skin. Extraintestinal manifestations are mostly caused by immunologic mechanisms, but may also be due to nutritional and metabolic complications, prothrombotic state and side effects of medications. Neurologic involvement is relatively less common. Neurologic complications have been reported 3% in adult IBD patients.1 Data on neurologic manifestations of IBD in children are limited and mostly consist of case reports. However, new and rare symptoms and complications have been reported in parallel with the increasing prevalence of this disease in children. Epilepsy, cerebrovascular disease, neuropathies, and neuropsychiatric disorders are the most common.2
Delirium is a neurocognitive disorder with rapid onset and fluctuating course, characterized by attention deficit, cognitive impairment and dysfunction, decreased ability to sustain and focus attention, damage to cognition and disorientation.3 Delirium usually occurs within a short period of time after an intense inflammatory stress event in vulnerable individuals.4 In IBD, alterations in brain activity, involvement of the brain-gut axis, malnutrition and inflammatory process may increase the risk of delirium. In a study conducted in geriatric (>65 years) IBD patients, the rate of delirium was found to be 0.3% and delirium picture was found to occur in patients who were hospitalized for a long time and whose nutrition was impaired.5 In this article, a child who presented with delirium and was subsequently diagnosed with UC is described.
Case Presentation
A 14-year-old male patient with no medical history presented with complaints of nonsensical speech and hallucinations for two days. He had diarrhea for two days and had no complaints of abdominal pain, vomiting or fever. His diarrhea was 2-3 times a day, watery and there was no nocturnal defecation. On examination, his height was 1.60 meters (z score: -0.77) and weight was 48.1 kg (z score: -0.93), and body mass index was 18.79 kg/m2 (z score: -0.65). He was agitated, aggressive and had poor time-space orientation. Other neurologic and systemic examinations were normal. Laboratory tests revealed low hemoglobin (9.6 g/dL), ferritin (12.9 µg/L), 25-hydroxy vitamin D (9.93 µg/L) and high C-reactive protein (48.8 mg/L). Other biochemical values (including electrolytes and albumin), urine and stool analysis and ammonia level were normal. Glucose, protein and immunoglobulin levels in the cerebrospinal fluid (CSF) were normal. Further laboratory investigations, including thyroid function tests, anti-nuclear antibodies, anti-double stranded deoxyribonucleic acid, complement (C3 and C4) levels and viral markers were negative. Electroencephalogram, brain magnetic resonance (MR) imaging and MR angiography were normal.
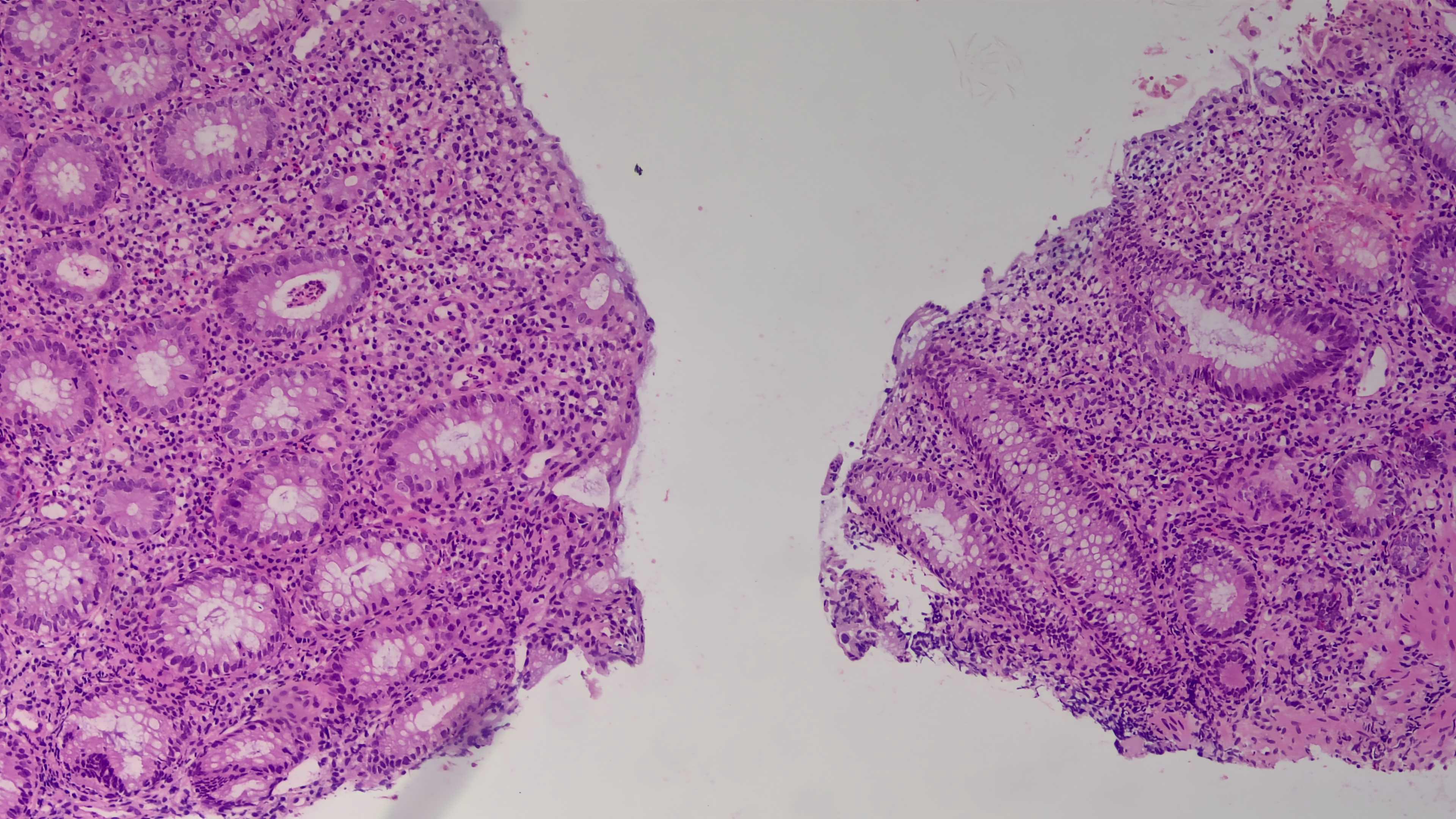
Vitamin B1 level was not evaluated because of the technical inadequacies in our hospital. The family was asked for a detailed list of the meals eaten by the child for three days. Using the “Computer Assisted Nutrition Program, Nutrition Information Systems Package Program (BeBiS, Version 7.2)”, adequate vitamin B1 intake was determined. Brain MRI was also normal and Wernicke’s encephalopathy was not considered. However, while investigating, the patient was hospitalized and immediately started on 250 mg intravenous thiamine three times a day for three days, followed by 100 mg daily. Intravenous immunoglobulin (1 g/kg/day) was administered for 5 days due to the inability to rule out autoimmune encephalopathy. As no clinical improvement was observed, pulse steroid therapy with methylprednisolone (30 mg/kg/day) was initiated for 5 days, followed by maintenance at 2 mg/kg/day. However, no response was obtained to this treatment either. Thereupon, plasma exchange was performed a total of 5 times. However, the patient’s delirium state continued. In addition, diarrhea increased and became bloody. Fecal calprotectin measured >300 μg/g and anti-neutrophil cytoplasmic antibodies were positive. Subsequently, a colonoscopy was performed in the third week of admission. We observed that the terminal ileum mucosa appeared normal. The submucosal vascular network had disappeared from the rectum to the cecum and the mucosa was granular and fragile. There were also multiple ulcers with exudate in the rectum and sigmoid colon (Mayo endoscopic score 3) (Fig. 1). Histopathologic examination revealed cryptitis, multiple crypt abscesses and intense lymphoplasmacytic inflammation (Fig. 2).

The patient was diagnosed with UC and a tumor necrosis factor-alpha (TNF-α) antagonist (infliximab) was started at a dose of 5 mg/kg at weeks 0, 2 and 6 and then every 8 weeks. After the 2nd dose, the delirium and diarrhea improved. After the 3rd dose, the patient had a Pediatric Ulcerative Colitis Activity Index (PUCAI) score of 5 (55 before treatment) and fecal calprotectin < 20 μg/g. The patient received infliximab treatment for two years and had no complaints during follow-up.
Discussion
We report a patient with UC who presented with delirium without any previous symptoms. UC may rarely present with neuropsychiatric symptoms. In the literature, delirium due to UC is usually associated with electrolyte disturbances or vitamin deficiencies, but the absence of these factors in our patient suggests that systemic inflammation may have led directly to neurological involvement. The fact that the patient showed resistance to steroid treatment but rapidly improved with an anti-TNF agent points to the critical role of TNF-α-mediated cytokine storm in the pathogenesis.
The etiology of UC is mostly thought to be related to various factors, including genetics, environment, infection and immune regulation disorders.6 Cytokines act as important signals in the initiation and maintenance of UC. Increased TNF-α levels in UC have proinflammatory effects on both the intestinal and central nervous systems. It has been suggested that neuronal damage associated with delirium may be linked to the inflammatory cascade triggered by TNF-α in the brain-gut axis.7,8 In this case, the patient did not respond to steroid treatment and his clinical condition rapidly improved with anti-TNF therapy. Anti-TNF therapy suppressed the cytokine storm by targeting TNF-α and controlled both gastrointestinal and neurological symptoms. Anemia and elevated acute phase reactant levels in our patient also indicate the severity of systemic inflammation. Increased proinflammatory cytokines such as TNF-α and interleukin-6 may lead to bone marrow suppression and stimulation of hepatic acute phase protein synthesis.
The management of extra-intestinal symptoms in IBD (most commonly in the joints, skin, hepatobiliary system and eyes) has been significantly altered by the use of anti-TNF drugs. A systematic review supported the benefits of anti-TNFs in the treatment of extraintestinal symptoms through the analysis of 9 interventional trials and 13 non-interventional trials.9 However, we could not find any data in the literature on the ameliorating effect of anti-TNF therapy on neurologic symptoms in UC patients. Our case shows that anti-TNF therapy has the potential to improve the neurologic manifestations of IBDs.
In conclusion, we present a patient with UC who presented with delirium as the first symptom and improved with anti-TNF therapy. Anti-TNF therapy may suppress the gastrointestinal symptoms of UC as well as the effects of inflammation on the brain and may help improve neurologic symptoms such as delirium. However, more clinical trials are needed to better understand the effect of anti-TNF therapy on neurologic symptoms.
Ethical approval
A written consent form was obtained from the family for this publication.
Source of funding
The authors declare the study received no funding.
Conflict of interest
The authors declare that there is no conflict of interest.
References
- Casella G, Tontini GE, Bassotti G, et al. Neurological disorders and inflammatory bowel diseases. World J Gastroenterol 2014; 20: 8764-8782. https://doi.org/10.3748/wjg.v20.i27.8764
- Dubinsky M. Special issues in pediatric inflammatory bowel disease. World J Gastroenterol 2008; 14: 413-420. https://doi.org/10.3748/wjg.14.413
- Siegel EJ, Traube C. Pediatric delirium: epidemiology and outcomes. Curr Opin Pediatr 2020; 32: 743-749. https://doi.org/10.1097/MOP.0000000000000960
- Ditzel FL, van Montfort SJ, Vernooij LM, et al. Functional brain network and trail making test changes following major surgery and postoperative delirium: a prospective, multicentre, observational cohort study. Br J Anaesth 2023; 130: e281-e288. https://doi.org/10.1016/j.bja.2022.07.054
- Aldiabat M, Aleyadeh W, Rana T, et al. Burden of delirium on mortality and healthcare resource utilization in geriatric patients hospitalized for inflammatory bowel disease. Proc (Bayl Univ Med Cent) 2024; 37: 509-515. https://doi.org/10.1080/08998280.2024.2342106
- Turner D, Ruemmele FM, Orlanski-Meyer E, et al. Management of paediatric ulcerative colitis, part 1: ambulatory care-an evidence-based guideline from European Crohn’s and colitis organization and European Society of Paediatric Gastroenterology, Hepatology and Nutrition. J Pediatr Gastroenterol Nutr 2018; 67: 257-291. https://doi.org/10.1097/MPG.0000000000002035
- Liu X, Yu Y, Zhu S. Inflammatory markers in postoperative delirium (POD) and cognitive dysfunction (POCD): a meta-analysis of observational studies. PLoS One 2018; 13: e0195659. https://doi.org/10.1371/journal.pone.0195659
- Noah AM, Almghairbi D, Evley R, Moppett IK. Preoperative inflammatory mediators and postoperative delirium: systematic review and meta-analysis. Br J Anaesth 2021; 127: 424-434. https://doi.org/10.1016/j.bja.2021.04.033
- Peyrin-Biroulet L, Van Assche G, Gómez-Ulloa D, et al. Systematic review of tumor necrosis factor antagonists in extraintestinal manifestations in inflammatory bowel disease. Clin Gastroenterol Hepatol 2017; 15: 25-36.e27. https://doi.org/10.1016/j.cgh.2016.06.025
Copyright and license
Copyright © 2025 The Author(s). This is an open access article distributed under the Creative Commons Attribution License (CC BY), which permits unrestricted use, distribution, and reproduction in any medium or format, provided the original work is properly cited.















