Graphical Abstract
Abstract
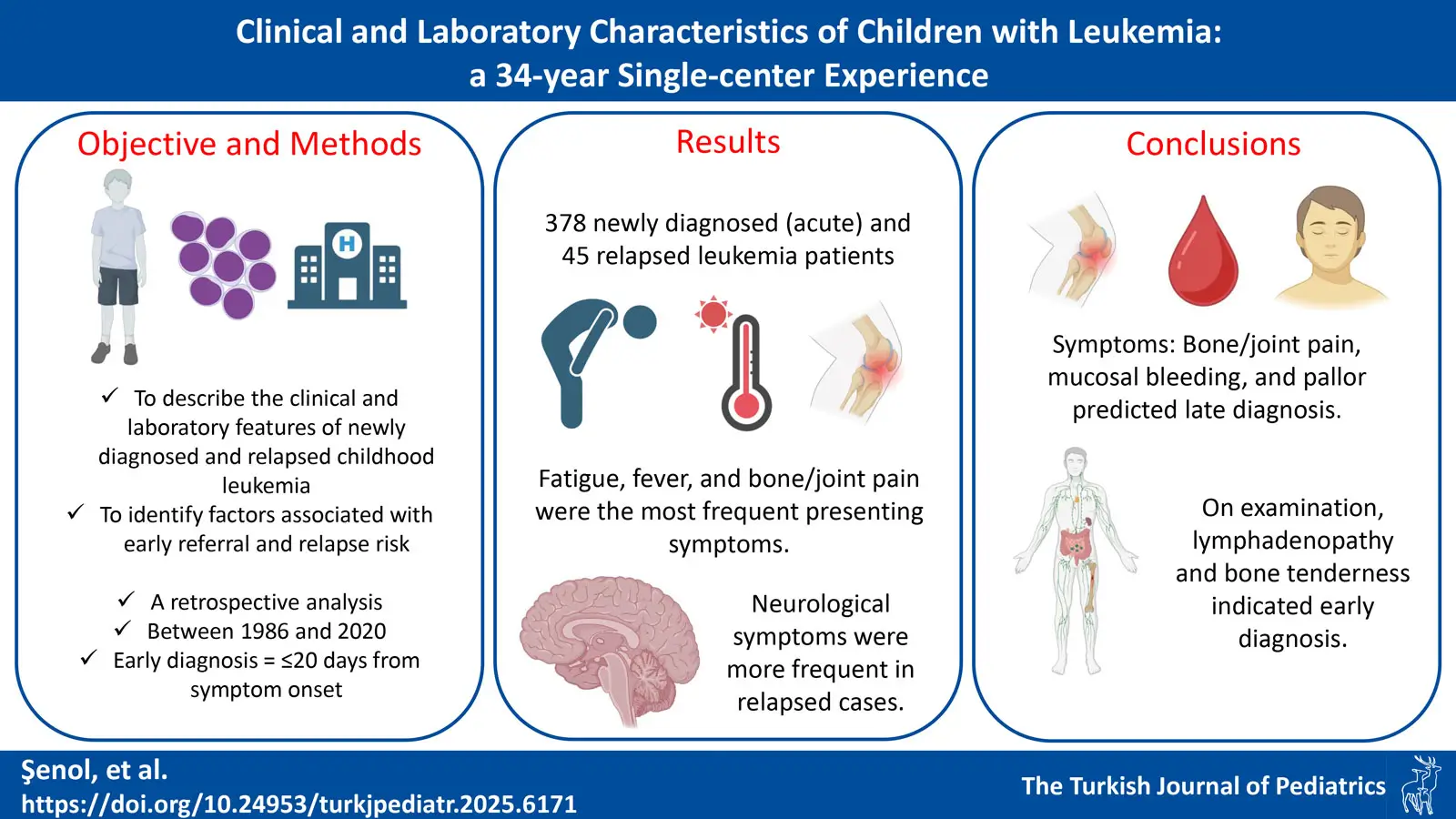
Backround. Leukemia is the most common childhood malignancy and often presents with nonspecific symptoms, which may lead to delays in diagnosis. Early recognition of clinical signs and laboratory abnormalities is essential to ensure timely referral and improve outcomes. This study assesses the clinical and laboratory characteristics of pediatric patients with acute and relapsed leukemia, points out key considerations during diagnosis, and investigates potential factors contributing to delayed diagnosis.
Methods. A retrospective analysis was performed on pediatric patients diagnosed with leukemia at a tertiary care hospital between the years 1986 and 2020. Early diagnosis was defined as a diagnosis made within 20 days of symptom onset.
Results. Among the 378 patients, fatigue was the most frequently reported symptom, followed by fever and bone or joint pain. Common laboratory abnormalities included anemia (83%), thrombocytopenia (80%), and leukocytosis (46%). Bone or joint pain (p< 0.001), mucosal bleeding (p=0.013), and pallor (p=0.005) were significantly associated with late diagnosis. In contrast, lymphadenopathy (p=0.014) and bone tenderness (p=0.024) were linked to earlier recognition. Among laboratory findings, low hemoglobin levels were associated with early diagnosis (p=0.023) and elevated platelet count was also significantly related to delayed diagnosis (p=0.028). In relapsed leukemia cases, abnormal blood count findings were common, and neurological symptoms were observed more frequently compared to acute leukemia patients.
Conclusions. Fatigue, fever, and bone or joint pain were identified as the most common presenting symptoms in acute leukemia cases, while hepatomegaly, splenomegaly, and lymphadenopathy were the predominant physical findings. Bone or joint pain, mucosal bleeding, and pallor were associated with late diagnosis, whereas lymphadenopathy and bone tenderness appeared to facilitate earlier recognition.
Keywords: childhood leukemia, clinical presentation, diagnostic delay, relapsed leukemia
Introduction
Leukemia is the most common childhood cancer, accounting for one-third of all childhood cancer cases.1Acute leukemias are divided into two main groups: acute lymphoblastic leukemia (ALL) and acute myeloid leukemia (AML).2 Relapsed leukemia is defined as the reappearance of disease in patients who have previously achieved remission.3 The initial symptoms, physical examination findings, and laboratory values of leukemias can mimic those of many other diseases. This often leads to misdiagnosis and delays in the diagnostic process.4 Low awareness of clinical symptoms and appropriate diagnostic tests may also contribute to delays in diagnosis.5 Therefore, early identification of symptoms, presence of specific physical findings and proper evaluation of laboratory tests are of critical importance. Herein, data at presentation of newly diagnosed leukemia cases and leukemic relapse cases over a 34-year period were analyzed. In this descriptive study, we defined the characteristics of patients who would be referred to the pediatric hematology department from primary health care institutions and the patients who would be at risk of relapse in the follow-up of leukemia.
Materials and Methods
Study design and participants
This study was approved by the Dokuz Eylül University Hospital Network Ethics Committee (Number of approval: 2020/15-36). In this study, pediatric patients diagnosed with acute leukemia and relapsed leukemia between the years 1986 and 2020 in the Division of Pediatric Hematology, Department of Pediatrics, Faculty of Medicine, Dokuz Eylül University were included. Symptoms, findings and laboratory parameters of the patients at the time of diagnosis were retrospectively analyzed.
Patients with acute leukemia were classified into two subgroups: ALL and AML. Relapsed cases were evaluated in comparison with patients newly diagnosed with acute leukemia.
The categorization of early and late diagnosis in the acute leukemia group was based on the median time to diagnosis calculated for the entire study population. Patients with a diagnostic interval shorter than the median value were assigned to the early diagnosis group, while those with an interval equal to or longer than the median were assigned to the late diagnosis group.
Symptom onset was assessed according to the history provided by the family. The time at which all presenting symptoms were first reported at the initial visit was considered the onset point.
Since there is a wide variation in age, normal blood count values were determined for each age group.6
Statistical evaluation
IBM SPSS Statistics 24.0 (SPSS Inc., Chicago, IL, USA) program was used for statistical evaluation. Frequency distributions were evaluated as number and percentage, and continuous variables (measurements) were evaluated as mean ± standard deviation. Shapiro–Wilk test was used to determine whether the data was normally distributed. For numerical variables, if the assumptions of parametric tests were met, the results were presented as mean ± standard deviation; if not, the median (minimum-maximum, interquartile range [IQR]) was reported. For categorical variables, the frequency (n) and percentage (%) were provided. In the comparison of continuous variables for two groups, Student-t test was used if there was a normal distribution, and Mann-Whitney U test if there was no normal distribution. Categorical variables were compared using Pearson chi-square or Fisher’s exact test. Reported p values were considered significant if <0.05. Logistic regression analysis was performed to identify clinical predictors of late diagnosis. In addition to symptom-based variables, similar regression models were planned for physical examination findings and laboratory parameters to assess their independent associations with delayed diagnosis.
Results
Of the total 423 patients in this study, 378 patients were diagnosed with newly diagnosed acute leukemia and 45 patients with relapsed leukemia. In the acute leukemia group, 313 (83%) patients had ALL, and its frequency aligned with previous studies.7,8 The median age of patients with acute leukemia was 58.5 months (3-216 months, IQR: 91 months) for ALL and 142.5 months (1 month-214 months, IQR: 89 months) for AML. The ages of diagnosis closely resembled those observed in earlier studies.9-11
Seventy-three patients with acute leukemia (19.3%) were referred with a suspicion of leukemia from various hospital departments. The majority were referred from the pediatric emergency department (26 patients, 6.9%), followed by orthopedics (10 patients, 2.6%), otorhinolaryngology (8 patients, 2.1%), and rheumatology (6 patients, 1.6%).
A total of 378 patients diagnosed with acute leukemia were included in the study. The mean age of these patients (196 males, 52%) was 71.5 months (1-216 months, IQR: 104 months). The median time from the onset of the first symptom to diagnosis was 20 days (2-350 days, IQR: 23 days). The most extreme outlier was a patient who had initially presented with the same symptoms—including fever, fatigue, approximately 10% weight loss over the preceding month, and bone pain—approximately ten months prior, followed by a recurrence of these symptoms. Fatigue was the most frequently reported symptom, followed by fever, bone or joint pain, and cutaneous signs of bleeding. The frequencies of symptoms were compared between ALL and AML patients. Bone or joint pain was more common in ALL patients and neurologic symptoms were more common in AML patients. Also, asymptomatic patients were more common in the AML group. Table I presents the distribution of symptoms among two groups. In addition to these, less common presenting symptoms among all patients with acute leukemia included cough (11 patients), gingival hyperplasia (7 patients), diarrhea (6 patients), hematuria (4 patients), night sweats (3 patients), and chest pain (2 patients).
| ALL: acute lymphoblastic leukemia, AML: acute myeloid leukemia. | |||
| Table I. Distribution of symptoms in acute leukemias (N=378). | |||
| Symptoms |
|
|
|
| Fatigue |
|
|
|
| Fever |
|
|
|
| Bone or joint pain |
|
|
|
| Weight loss |
|
|
|
| Mucosal bleeding |
|
|
|
| Skin bleeding |
|
|
|
| Neurological |
|
|
|
| Neck swelling |
|
|
|
| Pallor |
|
|
|
| Abdominal pain |
|
|
|
| Asymptomatic |
|
|
|
Among the physical examination findings at the time of admission, extramedullary involvement findings such as hepatomegaly, splenomegaly and lymphadenopathy (LAP) were common. Extramedullary involvement was observed more often in the ALL group, compared to the AML group. Pallor was the most frequent physical examination finding in the AML group. The comparative physical examination findings for the two groups are summarized in Table II.
| ALL: acute lymphoblastic leukemia, AML: acute myeloid leukemia. | |||
| Table II. Physical examination findings in acute leukemia (N=378). | |||
| Findings |
|
|
|
| Hepatomegaly |
|
|
|
| Splenomegaly |
|
|
|
| Lymphadenopathy |
|
|
|
| Pallor |
|
|
|
| Ecchymosis |
|
|
|
| Petechiae |
|
|
|
| Testicular enlargement, firmness |
|
|
|
| Normal Findings |
|
|
|
Anemia was present in 313 patients (82.8%), thrombocytopenia in 304 patients (80.4%), and both in 267 patients (70.6%). Leukocytosis was observed more commonly compared to leukopenia. The frequencies of abnormal complete blood count (CBC) findings are summarized in Table III.
| Table III. Complete blood count abnormalities in acute leukemia (N=378). | |
| Findings |
|
| Anemia |
|
| Thrombocytopenia |
|
| Anemia and thrombocytopenia |
|
| Leukocytosis |
|
| Leukocytosis and thrombocytopenia |
|
| Anemia and leukocytosis |
|
| Anemia, leukocytosis and thrombocytopenia |
|
| Leukopenia |
|
| Anemia and leukopenia |
|
| Leukopenia and thrombocytopenia |
|
| Anemia, leukopenia and thrombocytopenia (pancytopenia) |
|
Laboratory tests revealed that liver enzymes and phosphate levels were significantly higher in the ALL group. In the AML group, mean corpuscular volumes were recorded to be higher. No significant difference was observed between the other parameters. Table IV summarizes all laboratory parameters in acute leukemia.
| Data presented as median (range); ALL: acute lymphoblastic leukemia, ALT: alanine aminotransferase, AML: acute myeloid leukemia, AST: aspartate aminotransferase, LDH: lactate dehydrogenase, MCV: mean corpuscular volume. | |||
| Table IV. Laboratory findings in patients with ALL and AML (N=378). | |||
| Parameters |
|
|
|
| Leukocytes (x109 /L) |
|
|
|
| Neutrophils (x109 /L) |
|
|
|
| Hemoglobin (g/dL) |
|
|
|
| MCV (fL) |
|
|
|
| Thrombocytes (x109 /L) |
|
|
|
| LDH (IU/L) |
|
|
|
| Uric acid (mg/dL) |
|
|
|
| AST (IU/L) |
|
|
|
| ALT (IU/L) |
|
|
|
| Calcium (mg/dL) |
|
|
|
| Phosphate (mg/dL) |
|
|
|
Comparison between the early and late diagnosis groups revealed similar median ages at diagnosis, with 78.5 months in the early group and 84 months in the late group. Laboratory parameters, including leukocyte count, neutrophil count, hemoglobin level, and mean corpuscular volume, showed no significant differences between the groups. Thrombocyte and lactate dehydrogenase (LDH) levels were also comparable. Additionally, biochemical markers—including uric acid, aspartate aminotransferase, alanine aminotransferase, calcium, and phosphate—were similar in both groups.
In terms of clinical symptoms, fatigue, fever, and neck swelling occurred at similar rates across both groups. However, bone or joint pain, and weight loss were notably more prevalent in the late diagnosis group. Other symptoms, such as skin/ mucosal bleeding, neurological symptoms, and pallor, do not show substantial differences between the groups (see Table V).
|
Data presented as median (range) for numerical variables and as n (%) for categorical variables. ALL: acute lymphoblastic leukemia, ALT: alanine aminotransferase, AML: acute myeloid leukemia, AST: aspartate aminotransferase, LDH: lactate dehydrogenase, MCV: mean corpuscular volume. |
|||
| Table V. Comparatison of the characteristics of patients with early vs. late diagnosis. | |||
| Parameters |
|
|
|
| Age (month) |
|
|
|
| Leukocytes (x109 /L) |
|
|
|
| Neutrophils (x109 /L) |
|
|
|
| Hemoglobin (g/dL) |
|
|
|
| MCV (fL) |
|
|
|
| Thrombocytes (x109 /L) |
|
|
|
| LDH (IU/L) |
|
|
|
| Uric acid (mg/dL) |
|
|
|
| AST (IU/L) |
|
|
|
| ALT (IU/L) |
|
|
|
| Calcium (mg/dL) |
|
|
|
| Phosphate (mg/dL) |
|
|
|
| Fatigue |
|
|
|
| Fever |
|
|
|
| Bone or joint pain |
|
|
|
| Weight loss |
|
|
|
| Mucosal bleeding |
|
|
|
| Skin bleeding |
|
|
|
| Neurological |
|
|
|
| Neck swelling |
|
|
|
| Pallor |
|
|
|
In the logistic regression analysis, several clinical features were significantly associated with late diagnosis. Bone or joint pain (B = 1.357, p < 0.001, odds ratio [OR] = 3.886), mucosal bleeding (B = 1.076, p = 0.013, OR = 2.932), and pallor (B = 0.851, p = 0.005, OR = 2.341) were independently associated with a significantly increased likelihood of late diagnosis. When physical examination findings were analyzed separately, lymphadenopathy (B =-0.544, p = 0.014, OR = 0.580) and bone tenderness (B= -0.573, p=0.024, OR=0.564) were significantly associated with a decreased likelihood of late diagnosis. Among laboratory parameters, lower hemoglobin levels (B= -1.127, p = 0.023, OR = 0.880) and higher platelet counts (B=0.001, p=0.028, OR=1.003) were significantly associated with late diagnosis. Neutrophil count approached statistical significance (B = -0.017, p = 0.072, OR = 0.983), indicating a potential trend.
There were 45 patients (27 males, 60%) diagnosed with relapsed leukemia. Twenty-one (46.6%) of these patients were on maintenance therapy and 24 (53.4%) were diagnosed after the end of chemotherapy.
Our findings revealed that 37.8% of patients with relapse were diagnosed with relapse even though they were asymptomatic during routine follow-up. The majority of patients (42 out of 45, 93.3%) experienced relapse within the first five years following initial diagnosis. Among patients diagnosed with relapse, the most frequent complaints were related to the neurologic system, accounting for 18%. Three patients with relapse presented with testicular enlargement. The newly diagnosed leukemia group showed a higher frequency of symptoms like fatigue, fever, bone or joint pain, and weight loss, whereas the relapsed leukemia group had more instances of neurologic and testicular involvement. The distribution of symptoms for both groups is summarized in Table VI.
| Table VI. Distribution of symptoms in leukemias (N=423). | |||
| Symptoms |
|
|
|
| Fatigue |
|
|
|
| Fever |
|
|
|
| Bone or joint pain |
|
|
|
| Weight loss |
|
|
|
| Skin bleeding |
|
|
|
| Neurological symptoms |
|
|
|
| Neck swelling |
|
|
|
| Pallor |
|
|
|
| Testicular enlargement |
|
|
|
| Asymptomatic |
|
|
|
Patients with relapsed leukemia had less significant physical examination findings compared to those with newly diagnosed leukemia. The presence of hepatomegaly was observed in 10 patients (22%), splenomegaly in 7 patients (16%), and LAP in 3 patients (7%) with relapse. Testicular enlargement was observed in 4 patients (9%), surpassing its frequency in the newly diagnosed leukemia group (p=0.01).
Thrombocytopenia (26 cases, 58%) and anemia (16 cases, 36%) were the predominant CBC results among relapsed patients. Pathological CBC findings were observed in all symptomatic patients and in 55% of those without symptoms. Elevated uric acid and LDH levels due to tumor lysis syndrome were observed in 18 patients (40%).
Discussion
Acute leukemia is the most common malignancy in children. Since access to diagnostic facilities is more difficult especially in developing countries, the time to diagnosis varies from that in developed countries.5,12 Therefore, presenting symptoms, physical examination findings and first-line investigations should guide access to diagnostic facilities.
In the present study, fatigue was the most common symptom among patients diagnosed with acute leukemia (48.8%), followed by fever (46%), bone or joint pain (31%), and skin hemorrhage (17%). A recent study of 203 patients with ALL revealed that the most common symptoms were fatigue, fever, and bone or joint pain.13 A study conducted in our country, Türkiye showed that the top three symptoms were consistent with those of the present study, although fever was the leading cause for presentation.14 Another study conducted in Colombia identified pallor as the most frequently reported symptom, followed by anorexia and weight loss as the second and third most common symptoms, respectively.15 The most frequent presenting symptom in a study of 101 pediatric ALL patients from Saudi Arabia was fever, which was observed in one third of the cases. Fatigue and bone pain were also among the primary symptoms reported.16 In another study conducted in Türkiye, ALL was identified as the most common malignancy among children presenting with rheumatological symptoms17, underlining the importance of careful interpretation of clinical features in this patient group.
Another study from Saudi Arabia examined the presenting symptoms of 30 children with AML. The patients were highly symptomatic, with bone pain being the most common presenting symptom. The next most frequently reported symptoms were high fever and a history of bleeding.18 Our study involved the evaluation of 313 patients with ALL and 65 patients with AML. Both groups experienced fatigue and fever as the most common symptoms. Differences in the timing of presentation may explain the variation in symptom frequency.
In a recent study, 96.1% of patients diagnosed with acute leukemia had abnormal physical examination findings. This high rate highlights the importance of careful physical examination. In our 313 patients, the most common abnormal physical examination finding was hepatomegaly (65.3%). Splenomegaly (56.6%) and LAP (45.5%) were the other common abnormal findings, respectively. The present study’s findings aligned with the physical examination results in the study by Pérez et al.13 These three findings were more frequently reported in another study conducted in our country.14
Physical examination often reveals abnormal findings, but laboratory tests must be considered because there are a wide variety of different underlying diseases. CBC findings revealed that anemia was common (83%) in newly diagnosed leukemia patients. Thrombocytopenia was the second most common abnormal CBC finding in 304 patients (80%). Anemia and thrombocytopenia were present in 267 patients (71%). In the study by Pérez et al. evaluating CBC results, anemia and thrombocytopenia were prominent among other findings. The combination of the two was observed in more than half of the patients.13 These findings emphasize that the differential diagnosis of acute leukemia should be considered in patients with anemia and thrombocytopenia. These two laboratory findings can serve as a guide for referring patients to the hematology department, particularly from primary healthcare institutions.
Early and late diagnosis thresholds vary across studies. Thresholds for early and late diagnosis vary across studies. For example, a study from our country defined early diagnosis as within 15 days of symptom onset19, whereas studies from China and Japan used cutoffs of 24 and 30 days, respectively.20,21 These discrepancies underscore the absence of a universally accepted definition. In our study, we selected 20 days—the median time to diagnosis—as the threshold, in order to ensure comparable sample sizes between the early and late diagnosis groups. The median time to diagnosis reported in the literature ranges between 18.5 and 21 days4,22, which is consistent with the findings in our study.
Our study highlights the importance of identifying clinical and laboratory features associated with early and late diagnoses of acute leukemia.
Although the mean values of laboratory parameters were similar between the early and late diagnosis groups, multivariate regression analysis revealed that anemia was independently associated with a decreased likelihood of delayed diagnosis, while elevated platelet counts were linked to an increased risk. Our finding contrasts with previous literature. For example, a recent study in Türkiye reported elevated leukocyte and LDH levels, along with lower platelet counts late diagnosis group.19 These results suggest that peripheral blood abnormalities tend to become more pronounced in delayed cases. However, in our cohort—which included a larger sample size—we observed no such trend, indicating that delayed diagnosis may not consistently be associated with more evident hematological changes. Similarly, in a study by Dai et al. involving 419 patients with ALL, white blood cell counts and hemoglobin levels were found to be comparable between the early and late diagnosis groups, whereas platelet counts were higher in the late diagnosis group.20 In light of these findings, it may be inferred that patients with more marked laboratory abnormalities are more likely to receive an earlier diagnosis. Accordingly, the observation that peripheral blood parameters were similar between early and late diagnosis groups in these two larger studies —despite the expectation of more pronounced abnormalities in delayed cases— may also be attributed to this tendency. This may lead to the suggestion that greater clinical awareness is directed toward laboratory parameters. In our study, we also investigated clinical symptoms and physical examination findings that might contribute to diagnostic delay. Notably, certain clinical symptoms, including bone or joint pain, mucosal bleeding, and pallor, emerged as significant indicators of delayed diagnosis. In contrast, physical findings such as lymphadenopathy and bone tenderness appeared to be more frequent in patients diagnosed earlier, suggesting that the presence of specific physical signs may facilitate timely recognition.
Our findings, showing similar frequencies of fatigue, fever, and lymphadenopathy between groups, further highlight the diagnostic challenges and the often subtle nature of presenting symptoms.
Despite advances in modern chemotherapy, relapsed leukemia remains the leading cause of mortality among children diagnosed with acute leukemia.23 In the present study, relapse occurred in 45 (11.9%) out of 378 patients with acute leukemia. Among the patients, 19 (42%) experienced relapse while undergoing treatment, while 26 (%58) had relapsed during post-chemotherapy follow-up. In this study, 17 asymptomatic cases (37.8%) were diagnosed with relapsed leukemia based on physical examination and laboratory findings at routine follow-up. This result underlines the importance of follow-up. Among the laboratory tests, especially CBC revealed frequently abnormal results in symptomatic and asymptomatic patients. Once again, in this study the significance of routine follow-up with CBC was highlighted, as also reported in previous studies.24 Neurologic symptoms were the most common symptom in relapsed cases. We recorded this as a result that could lead to an increased focus on neurologic symptoms at routine follow-up.
Our study has some limitations, including its retrospective design and single-center setting. Moreover, we were unable to assess several potential contributors to diagnostic delay —such as misinterpretation of symptoms by patients or parents, delayed presentation to healthcare facilities, parental education level, socioeconomic status, the patient’s pubertal status, and the specialty of the first physician consulted outside the hospital— due to lack of available data.
Conclusions
The present study revealed that fatigue, fever, and bone or joint pain were the primary symptoms observed in children with acute leukemia. The most common physical examination findings in acute leukemia patients were hepatomegaly, splenomegaly, and lymphadenopathy. The most frequently observed abnormalities in the CBC of acute leukemia patients were anemia and thrombocytopenia. Clinical symptoms such as bone or joint pain, mucosal bleeding, and pallor were associated with late diagnosis, whereas physical signs like lymphadenopathy and bone tenderness were linked to earlier recognition. In addition, elevated platelet counts may indicate an increased risk of delayed diagnosis, whereas low hemoglobin levels appear to be associated with a lower likelihood of diagnostic delay. Abnormal CBC findings were commonly observed at the time of relapsed leukemia diagnosis. Moreover, neurological symptoms emerged as the leading cause for hospital admission in these cases. In addition to the complaints, a careful physical examination and evaluation of the CBC are important in both diagnosis of initial leukemia and the detection of relapse.
Ethical approval
The study was approved by Dokuz Eylül University Hospital Network Ethics Committee (date: 06.07.2020 number: 2020/15-36).
Source of funding
The authors declare the study received no funding.
Conflict of interest
The authors declare that there is no conflict of interest.
References
- Tubergen DG, Bleyer A, Ritchey AK. Acute lymphoblastic leukemia. In: Kliegman RM, Stanton BF, St Geme JW, Schor NF, Behrman RE, editors. Nelson textbook of pediatrics. 20th ed. Philadelphia: Elsevier Saunders; 2015.
- Seth R, Singh A. Leukemias in children. Indian J Pediatr 2015; 82: 817-824. https://doi.org/10.1007/s12098-015-1695-5
- Fuster JL. Current approach to relapsed acute lymphoblastic leukemia in children. World J Hepatol 2014; 3: 49. https://doi.org/10.5315/wjh.v3.i3.49
- Chen J, Mullen CA. Patterns of diagnosis and misdiagnosis in pediatric cancer and relationship to survival. J Pediatr Hematol Oncol 2017; 39: e110-e115. https://doi.org/10.1097/MPH.0000000000000688
- Fajardo-Gutiérrez A, Sandoval-Mex AM, Mejía-Aranguré JM, Rendón-Macías ME, Martínez-García MD. Clinical and social factors that affect the time to diagnosis of Mexican children with cancer. Med Pediatr Oncol 2002; 39: 25-31. https://doi.org/10.1002/mpo.10100
- Adeli K, Raizman JE, Chen Y, et al. Complex biological profile of hematologic markers across pediatric, adult, and geriatric ages: establishment of robust pediatric and adult reference intervals on the basis of the Canadian Health Measures Survey. Clin Chem 2015; 61: 1075-1086. https://doi.org/10.1373/clinchem.2015.240531
- Margolin JF, Rabi KR, Steuber CP, Poplack DG. Acute lymphoblastic leukemia. In: Pizzo PA, Poplack DG, editors. Principles and practice of pediatric oncology. Philadelphia: Lippincott Williams & Wilkins; 2011: 518-565.
- Pagliaro L, Chen SJ, Herranz D, et al. Acute lymphoblastic leukaemia. Nat Rev Dis Primers 2024; 10: 41. https://doi.org/10.1038/s41572-024-00525-x
- Katz AJ, Chia VM, Schoonen WM, Kelsh MA. Acute lymphoblastic leukemia: an assessment of international incidence, survival, and disease burden. Cancer Causes Control 2015; 26: 1627-1642. https://doi.org/10.1007/s10552-015-0657-6
- Fadoo Z, Nisar I, Yousuf F, et al. Clinical features and induction outcome of childhood acute lymphoblastic leukemia in a lower/middle income population: a multi-institutional report from Pakistan. Pediatr Blood Cancer 2015; 62: 1700-1708. https://doi.org/10.1002/pbc.25583
- Lustosa de Sousa DW, de Almeida Ferreira FV, Cavalcante Félix FH, de Oliveira Lopes MV. Acute lymphoblastic leukemia in children and adolescents: prognostic factors and analysis of survival. Rev Bras Hematol Hemoter 2015; 37: 223-229. https://doi.org/10.1016/j.bjhh.2015.03.009
- Lins MM, Amorim M, Vilela P, et al. Delayed diagnosis of leukemia and association with morbid-mortality in children in Pernambuco, Brazil. J Pediatr Hematol Oncol 2012; 34: e271-e276. https://doi.org/10.1097/MPH.0b013e3182580bea
- Jaime-Pérez JC, García-Arellano G, Herrera-Garza JL, Marfil-Rivera LJ, Gómez-Almaguer D. Revisiting the complete blood count and clinical findings at diagnosis of childhood acute lymphoblastic leukemia: 10-year experience at a single center. Hematol Transfus Cell Ther 2019; 41: 57-61. https://doi.org/10.1016/j.htct.2018.05.010
- Karbuz A, Yaralı N, Işık P, Bay A, Kara A, Tunç B. The demographic features and treatment complications of acute leukemia patients: a single center experience. Turk J Pediatr Dis 2017; 11: 19-26. https://doi.org/10.12956/tjpd.2016.254
- Castro-Jiménez MÁ, Rueda-Arenas E, Cabrera-Rodríguez D. Approach to prediagnostic clinical semiology, noticed by mothers, of childhood acute lymphoblastic leukemia. Arch Argent Pediatr 2015; 113: 331-336. https://doi.org/10.5546/aap.2015.eng.331
- Qari MH, Alattas AA, Binkuddah SM, et al. Mutations encountered in acute lymphoblastic leukemia: a retrospective study in a teaching hospital in Jeddah, Saudi Arabia. Cureus 2021; 13: e12426. https://doi.org/10.7759/cureus.12426
- Çağlayan Ş, Koç BŞ, Baba Ö, et al. Evaluation of childhood malignancies presenting with musculoskeletal manifestations from two different divisions: a multicenter study. Turk J Pediatr 2024; 66: 81-89. https://doi.org/10.24953/turkjped.2023.446
- Al Daama SA, Aldayel AQ, Alafgani S, et al. Chidhood AML: is it difficult to cure? King Fahd Specialist Hospital Damman experience. Life Science Journal 2013; 10: 2354-2360.
- Kirkız Kayalı S, Kaya Z. Pathological signs in the diagnosis and causes of delay at initial admission in children with acute leukemia: a single-center experience. Turkiye Klinikleri J Pediatr 2024; 33: 35-40. https://doi.org/10.5336/pediatr.2024-101461
- Dai Q, Liu R, Wang Y, et al. Longer time intervals from symptom onset to diagnosis affect the overall survival in children with acute lymphoblastic leukemia. J Pediatr Hematol Oncol 2022; 44: 285-292. https://doi.org/10.1097/MPH.0000000000002344
- Tamefusa K, Ochi M, Ishida H, et al. Delayed diagnostic interval and survival outcomes in pediatric leukemia: a single-center, retrospective study. Eur J Haematol 2024; 112: 714-722. https://doi.org/10.1111/ejh.14162
- Dang-Tan T, Trottier H, Mery LS, et al. Delays in diagnosis and treatment among children and adolescents with cancer in Canada. Pediatr Blood Cancer 2008; 51: 468-474. https://doi.org/10.1002/pbc.21600
- Sun W, Orgel E, Malvar J, et al. Treatment-related adverse events associated with a modified UK ALLR3 induction chemotherapy backbone for childhood relapsed/refractory acute lymphoblastic leukemia. Pediatr Blood Cancer 2016; 63: 1943-1948. https://doi.org/10.1002/pbc.26129
- Gandhi M, Rao K, Chua S, Saha V, Lilleyman J, Shankar A. Routine blood counts in children with acute lymphoblastic leukaemia after completion of therapy: are they necessary? Br J Haematol 2003; 122: 451-453. https://doi.org/10.1046/j.1365-2141.2003.04453.x
Copyright and license
Copyright © 2025 The Author(s). This is an open access article distributed under the Creative Commons Attribution License (CC BY), which permits unrestricted use, distribution, and reproduction in any medium or format, provided the original work is properly cited.















