Graphical Abstract
Abstract
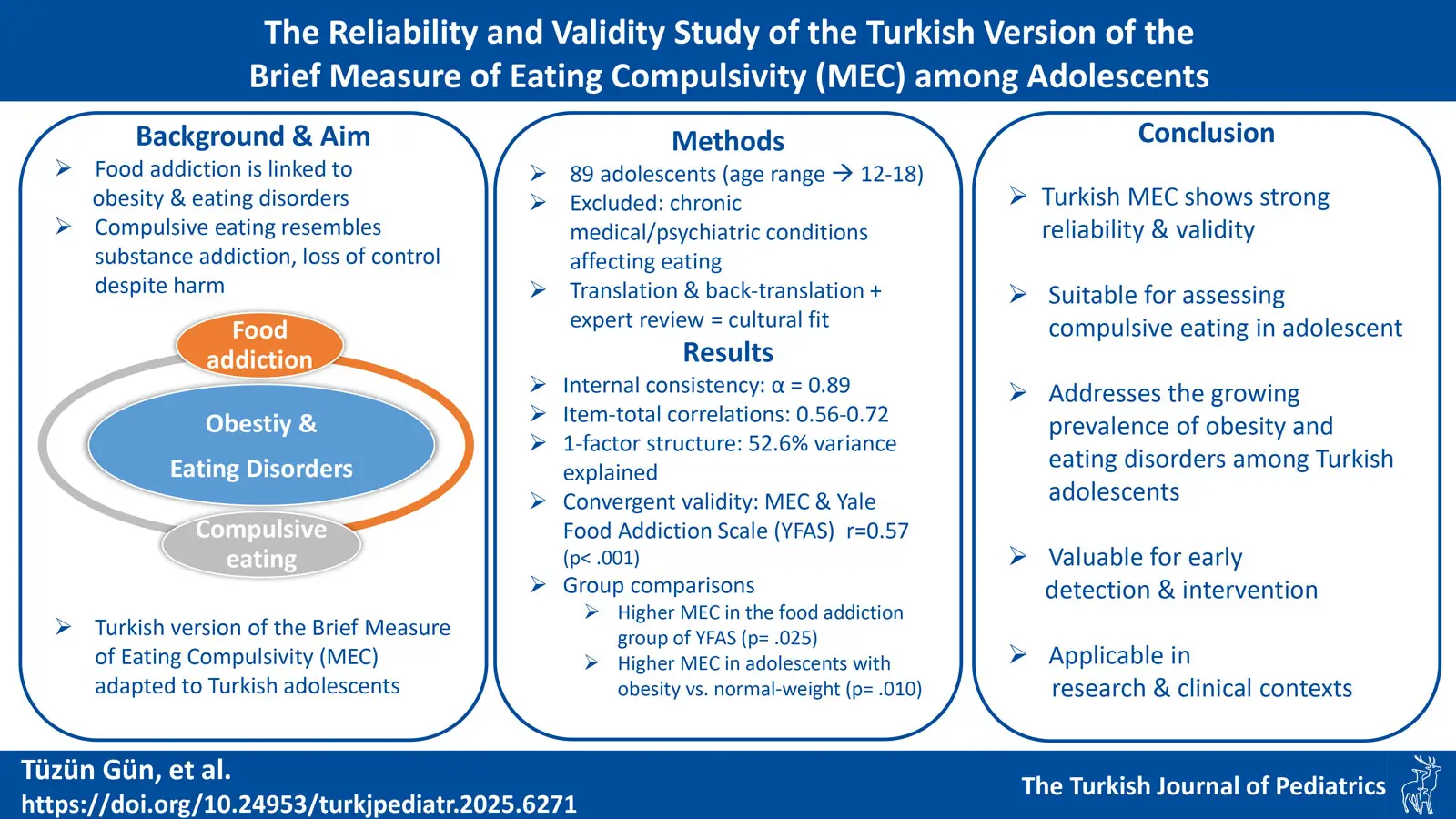
Background. Food addiction has been increasingly recognized as a contributing factor to obesity and eating disorders. Compulsive eating, characterized by an uncontrollable urge to consume food despite adverse consequences, shares behavioral similarities with substance addiction. This study aims to adapt the Brief Measure of Eating Compulsivity (MEC) into Turkish and evaluate its validity and reliability in the adolescent population.
Methods. The study included a sample of 89 adolescents aged 12-18 years. Participants without chronic medical or psychiatric conditions affecting eating behaviors were included. The adaptation process involved translation, back-translation, and expert evaluations to ensure cultural and linguistic appropriateness. The psychometric properties of the Turkish MEC were assessed through internal consistency, exploratory factor analysis, and criterion validity using the Yale Food Addiction Scale (YFAS).
Results. The internal consistency of the Turkish MEC was 0.89, with item-total correlations ranging from 0.56 to 0.72. Factor analysis supported a single-factor structure explaining 52.6% of the variance. Convergent validity was established through a significant positive correlation with YFAS scores (r = 0.57, p < 0.001). Criterion validity analysis demonstrated significantly higher MEC scores in individuals classified as food addicts by YFAS (p = 0.025). Additionally, significant differences in MEC scores were observed across body mass index categories (p = 0.010), with higher scores in adolescents with obesity compared to the normal-weight group.
Conclusions. The Turkish version of the MEC demonstrated strong reliability and validity among adolescents, supporting its use in assessing compulsive eating behaviors. Given the increasing prevalence of obesity and eating disorders in Turkish youth, this tool provides a valuable resource for early detection and intervention in research and clinical settings.
Keywords: compulsive eating, obesity, adolescents
Introduction
The impact of food addiction on obesity and eating disorders has become a prominent focus in contemporary research. Central areas of inquiry include the excessive intake of certain foods, especially those rich in carbohydrates and fats, and the psychological determinants affecting eating behaviors.1,2 The observed resemblance between substance addiction and compulsive overeating broadly supports the concept of food addiction. Compulsiveness, characterized by an uncontrollable urge to continue a behavior despite its adverse consequences, is a crucial feature of addiction.3 This is exemplified by analogous patterns in both conditions, including persistent engagement in behaviors despite adverse outcomes, withdrawal symptoms, obsessive preoccupation, increasing consumption, guilt after excessive intake and repetitive behaviors.4,5
The causes of obesity include, but are not limited to genetic predisposition, poor dietary habits, lack of physical activity, and medical conditions.6 Notably, some individuals with obesity may exhibit eating patterns akin to those observed in substance addiction. This observation has resulted in the hypothesis that food addiction might also contribute to the development of obesity.7,8 Consequently, compulsive overeating is regarded as a factor that both contributes to and perpetuates obesity in affected individuals.
It is essential to adapt objective measurement tools into the Turkish language, which facilitates healthcare professionals’ ability to discuss eating behaviors and habits with their patients, thereby guiding research and practice in this domain. Reviewing the relevant literature in Türkiye, the single validated self-report measure is the Yale Food Addiction Scale (YFAS).9 The YFAS primarily evaluates food addiction based on substance dependence criteria, which may not fully capture the compulsive dimension of disordered eating behaviors. Considering the removal of the distinction between abuse and dependence in the 5th edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5)10 and the crucial role of compulsivity in assessing addiction, Shroder et al.11 identified a need for a concise, user-friendly instrument that could effectively assess the compulsive component of food addiction and could be used in both research and clinical settings. The Brief Measure of Eating Compulsivity (MEC) was developed as a short and effective tool to assess a key aspect of food addiction—eating compulsivity. The 10-item scale (MEC-10) was initially validated in a sample of 65 individuals with a body mass index (BMI) of 30 or higher, demonstrating strong internal consistency and excellent test-retest reliability. Its brevity and psychometric strength make it suitable for clinical and research applications. Given the rising prevalence of obesity within the adolescent population in Türkiye12-14, it was deemed necessary to adapt a brief yet comprehensive measure, such as the MEC, to address the gap in assessment tools within this specific age group. Therefore, the aim of this study was to examine the validity and reliability of MEC, designed to assess compulsive eating, a significant facet of eating behaviors.
Materials and Methods
Participants
The study was conducted at Hacettepe University, Division of Adolescent Medicine. The sample comprises 89 adolescents aged 12-18 who attend the adolescent medicine outpatient clinic. Adolescents without chronic medical conditions (such as diabetes mellitus or other endocrine disorders) and/or psychiatric diagnoses (including eating disorders) were included in the study. Other exclusion criteria include cognitive impairments affecting comprehension and completion of the questionnaire, using prescription/nonprescription drugs, or having a substance abuse problem that may cause compulsive eating behavior. Adolescents whose BMI was between the 5th and 85th percentiles and below the 5th percentile according to age and gender were included in the normal weight and underweight groups, respectively. Adolescents whose BMI was between the 85th-95th and above the 95th percentile according to age and gender were included in the overweight and obesity groups, respectively. Ethics board approval of the study (GO/19/770) was obtained from the Hacettepe University Non-Interventional Clinical Research Ethics Committee. Written informed consent was obtained from parents, and written assent was obtained from participants.
Measurement tools
Brief Measure of Eating Compulsivity (MEC): This measure was developed by Schroder et all.11 It is a ten-item, five-point Likert scale (0 = definitely false and 4 = definitely true). The compulsive eating score is defined as the sum of the item scores and a higher score indicates an elevated level of compulsive eating. The internal consistency (Cronbach alpha) of the original scale was found to be 0.94. Factor analysis revealed that the scale explains 67.4% of the total variance, with items loading onto a single factor. The test-retest reliability coefficient was 0.92. The validity study showed that the score from the MEC effectively predicted the group identified as food addicts by the Yale Food Addiction Scale. The Spearman’s correlation between the two scales was 0.727 (p < 0.001).
Yale Food Addiction Scale (YFAS): The Yale Food Addiction Scale is employed to identify individuals’ addiction to high-fat and sugary foods, paralleling the diagnostic criteria for substance addiction. This scale, designed to assess food addiction, comprises 27 items and demonstrates substantial internal consistency, as indicated by a Cronbach’s alpha coefficient of 0.93. Furthermore, the scale’s discriminant validity is statistically significant, evidenced by the observed difference between clinical and non-clinical groups (t = 10.662, p < 0.002). The Turkish adaptation of the scale was performed by Bayraktar, Erkman, and Kurtuluş15 and demonstrated statistically significant internal consistency (Cronbach’s alpha = 0.93) and discriminant validity (t = 10.662, p < 0.002).
Procedure
To conduct the Turkish adaptation study, including translation, validity, and reliability of the MEC within an adolescent sample, the research team first secured prior approval from Rita Shroeder for the Turkish validation of the scale with Turkish adolescents. After obtaining the permission, the scale was independently translated from English to Turkish by two individuals proficient in both languages. These translators were familiar with the subject matter under investigation and thoroughly understood the construct assessed by the test. Subsequently, two professors of pediatrics evaluated and provided necessary recommendations for these translations for accuracy and cultural relevance. The research team reviewed these evaluations to establish a consensus translation, which was subsequently back-translated into English by another professor in psychology proficient in both languages and found to be compatible with the original scale. Then the final Turkish version was obtained to use for the validation. Participants were asked to fill out both the MEC and YFAS under supervision, ensuring that they could seek clarification if they encountered any difficulties in understanding the items.
Statistical analysis
Statistical Package for Social Sciences (SPSS Inc. Chicago IL) is used to analyze data, version 22.0, with a significance level set at p ≤ 0.05 for all statistical procedures. Among the 94 participants, those who left 5% or more of the scale items blank were identified using the NMISS function, which calculates the number of missing observations for each variable, enabling us to assess data completeness and ensure that our analyses appropriately accounted for any incomplete cases, and 5 participants were removed from the data set. All subsequent analyses were conducted on this final sample of 89 participants. The suitability of the variables to a normal distribution was assessed using Kolmogorov-Smirnov test. Descriptive statistics for continuous variables are presented as mean ± standard deviation (SD), or median and interquartile range (IQR), while categorical variables are expressed as percentages. For the scale scores that deviated from a normal distribution, the Mann-Whitney U and Kruskal-Wallis tests were employed for comparisons. The Cronbach’s alpha coefficient and item-total correlations were computed to determine the internal consistency. Additionally, the split-half reliability was assessed, and the Spearman-Brown coefficient was calculated to evaluate the consistency between the two halves of the scale. Exploratory factor analysis (EFA) method was used to evaluate the scale’s factor structure. Spearman’s correlational analysis was employed to investigate the relationship between MEC and BMI. The Kruskal-Wallis test was used to examine the differences in MEC scores across BMI groups. The Mann-Whitney U test was used to investigate the difference between the MEC mean scores of the groups based on the YFAS food addiction score.
Results
Demographics and anthropometric data
The mean age of the sample (n=89) was 14.9 ± 1.65 years, and 65.2% were female. Participants’ mean weight was 66.09 ± 17.72 kg (min-max: 34-113 kg), and the mean height was 162.9 ± 8.62 cm (min-max: 134-182 cm). BMI Z score ranged from -3.63 to 2.43, with a mean of 0.64 ± 1.33. In the BMI distribution, 5% of the participants were classified as underweight, 33% as normal weight, 24% as overweight and 27% as obese.
Reliability analysis
The median score of MEC was 13 (IQR=14). The Cronbach’s alpha value was calculated as an indicator of the internal consistency coefficient and found to be 0.89. Cronbach’s alpha values exceeding 0.80 indicate high internal consistency.16 The split-half reliability of the 10-item scale was assessed using the Spearman-Brown coefficient. The Spearman-Brown coefficient for equal length was 0.89, indicating good internal consistency for the scale. In addition to assessing the internal consistency coefficient, item-total score correlations were analyzed. The item-total correlation values ranged from 0.56 to 0.72. All item-total test correlation coefficients were above 0.40. Table I shows the summary of the psychometric properties of the MEC items.
| Table I. Psychometric properties of Brief Measure of Eating Compulsivity (MEC). | |||||
|
|
|
|
|
|
|
| I have urges to eat a lot of the time |
|
|
|
|
|
| I feel disturbed about my urges to eat |
|
|
|
|
|
| I have very little control over my eating |
|
|
|
|
|
| I often fear losing control of my eating |
|
|
|
|
|
| I am not able to control how much I eat in the presence of any food |
|
|
|
|
|
| I often feel out of control around certain foods |
|
|
|
|
|
| Food is like a drug to me |
|
|
|
|
|
| It worries me how little control I have over my eating |
|
|
|
|
|
| When I come across a very tasty food I can’t stop thinking about it |
|
|
|
|
|
| I feel defeated by food |
|
|
|
|
|
Validity analysis
Before evaluating factor structure, the Kaiser-Meyer Olkin (KMO) and Bartlett tests were used. The KMO value of 0.89 (higher than 0.050) and a statistically significant result on the Bartlett test (x= 418.73, df=45, p<0.00) were found. These showed that the data were appropriate for factor analysis. The EFA (Principal Component Analysis, varimax rotation) showed a single factor that accounted for 52.6% of the total variance.
Convergent validity
To evaluate the convergent validity of the MEC, Spearman’s correlational coefficient between MEC and YFAS was analyzed, and it was found that the coefficients for the relationship were statistically significant (Spearman’s r=0.57, p<.001).
Criterion validity
A significant difference (U = 433.5, p = 0.025) was observed between the mean MEC scores of individuals diagnosed with food addiction (MEC mean rank = 65.93) and those without such a diagnosis (MEC mean rank = 43.21), as assessed by the YFAS. The mean MEC score for those diagnosed with food addiction is significantly higher.
Analysis of BMI group differences according to MEC scores revealed a significant difference (χ2(3)=11.31, p=0.010) in MEC scores between the normal weight group (MEC mean rank =35.71) and the group with obesity (MEC mean rank = 57.56). The mean MEC score for the obese group was significantly higher than that of the normal weight group.
Discussion
This study’s results provide strong evidence for the reliability and validity of the Turkish version of MEC, supporting its use in assessing compulsive eating behaviors among Turkish adolescents. The Cronbach’s alpha coefficient of 0.89 indicates a high degree of internal consistency and the item-total score correlations ranged from 0.56 to 0.72, providing additional support for the reliability.16,17 The strong item-total correlations further support the internal consistency of the scale, indicating that the items measure a common underlying construct.17
The EFA revealed a single-factor structure, which aligns with the conceptual framework of the original scale, suggesting that compulsive eating is a unidimensional construct within this population.11 The significant positive correlation between MEC scores and the YFAS indicates that the MEC effectively measures a construct closely related to food addiction, consistent with previous research demonstrating the association between compulsive eating behaviors and food addiction symptoms.18 This result confirms that the scale captures behaviors characteristic of compulsive eating as intended and reinforces its relevance for both research and clinical settings. Adolescents with food addiction, as identified by the YFAS, had significantly higher MEC scores than those without food addiction. This distinction demonstrates that the MEC can differentiate between individuals based on their level of compulsive eating behavior.11
Adolescence is a critical period for physical, emotional, and cognitive development, during which unhealthy eating behaviors can become deeply ingrained and contribute to the development of long-term health risks, including obesity, eating disorders and metabolic disorders.19-21 As the findings suggest, adolescents with higher compulsive eating tendencies are more likely to have elevated BMI and meet the criteria for food addiction. This underscores the importance of identifying these behaviors early, as untreated compulsive eating can lead to obesity and escalate into more severe eating disorders.22 Moreover, differences in MEC scores across BMI categories provide further evidence of the scale’s sensitivity.11 The higher MEC scores among adolescents with obesity reflect the strong association between compulsive eating and obesity, highlighting the importance of assessing these behaviors in this population, while avoiding stigmatization. Given that obesity rates among Turkish youth are rising12-14, MEC can play a crucial role in the early detection of adolescents with compulsive eating and can promote targeted intervention since the treatment approach differs from obesity with other root causes.
Compulsive eating -characterized by a loss of control over eating- is a key component of several eating disorders, such as binge eating disorder.4,23 Assessing compulsive eating behaviors is critical, especially considering the DSM-5’s removal of the distinction between abuse and dependence, shifting the focus toward compulsivity as a core feature of addiction.24 It is essential to have reliable and valid tools to assess compulsive eating, which plays a key role in disordered eating behaviors. Our findings provide initial evidence that the Turkish version of the MEC is a suitable instrument for both research and clinical applications, offering a concise way to assess eating compulsivity in this age group.
Early intervention is essential for preventing the progression of disordered eating into clinical eating disorders, which are associated with serious physical and psychological consequences.25,26 Eating disorders can impair social functioning, and mental health, leading to depression, anxiety, and other medical complications, some of which can lead to life-threatening conditions.27,28 By identifying compulsive eating behaviors during adolescence, healthcare providers can intervene earlier, reducing the risk of developing full-blown eating disorders and obesity. In many developing countries, like Türkiye where awareness among caregivers and healthcare professionals are not high, and health services for eating disorders are still limited, having culturally adapted, psychometrically sound tools like the MEC is crucial. These tools allow for more accurate assessments in both research and clinical settings, enabling clinicians and researchers to better understand the unique patterns of disordered eating in adolescents. Furthermore, integrating assessments of compulsive eating into routine health screenings could enhance preventive efforts, providing opportunities for education, counseling, and behavioral interventions that promote healthy eating habits.
The MEC relies on self-reported data, which may introduce bias due to participants underreporting or overreporting their eating behaviors, particularly with sensitive topics like compulsive eating. The study employed a cross-sectional design, which limits the ability to assess changes in compulsive eating behaviors over time or determine causality between compulsive eating, BMI, and food addiction. Unlike the original scale development study, test-retest reliability could not be evaluated in this study due to difficulties in re-contacting the hospital-based outpatient sample within a standard retest interval. Although the sample provided meaningful insights, the study’s findings may not be generalizable to all adolescents in Türkiye. Although the MEC was adapted to Turkish, certain cultural nuances around food, eating behaviors, and addiction may not be fully captured. While the MEC showed significant associations with the YFAS, the study did not include other clinical assessments or interviews to provide a more comprehensive evaluation of compulsive eating or related mental health issues.
In conclusion, the Turkish adaptation of the MEC offers an effective, valid and reliable instrument to assess compulsive eating behaviors among adolescents in Türkiye. Its ability to distinguish between individuals with and without food addiction, as well as its alignment with related constructs like YFAS, underscores its relevance for both research on eating behaviors and clinical interventions targeting obesity and disordered eating.
Acknowledgements
We gratefully acknowledge the valuable recommendations and insights provided by Dr. Elif Nursel Özmert and Dr. Gülen Eda Utine who contributed to the translation and cultural adaptation of the scale.
Ethical approval
The study was approved by Hacettepe University Non-Interventional Clinical Research Ethics Committee (number: GO/19/770).
Source of funding
The authors declare the study received no funding.
Conflict of interest
The authors declare that there is no conflict of interest.
References
- Davis C, Carter JC. Compulsive overeating as an addiction disorder. A review of theory and evidence. Appetite 2009; 53: 1-8. https://doi.org/10.1016/j.appet.2009.05.018
- Schankweiler P, Raddatz D, Ellrott T, Hauck Cirkel C. Correlates of food addiction and eating behaviours in patients with morbid obesity. Obes Facts 2023; 16: 465-474. https://doi.org/10.1159/000531528
- Davis C. From passive overeating to “food addiction”: a spectrum of compulsion and severity. ISRN Obes 2013; 2013: 435027. https://doi.org/10.1155/2013/435027
- Gold M, Frost-Pineda K, Jacobs W. Overeating, binge eating, and eating disorders as addictions. Psychiatr Ann 2003; 33: 117-122. https://doi.org/10.3928/0048-5713-20030201-08
- Alavi SS, Ferdosi M, Jannatifard F, Eslami M, Alaghemandan H, Setare M. Behavioral addiction versus substance addiction: correspondence of psychiatric and psychological views. Int J Prev Med 2012; 3: 290-294.
- Westbury S, Oyebode O, van Rens T, Barber TM. Obesity stigma: causes, consequences, and potential solutions. Curr Obes Rep 2023; 12: 10-23. https://doi.org/10.1007/s13679-023-00495-3
- Liu Y, von Deneen KM, Kobeissy FH, Gold MS. Food addiction and obesity: evidence from bench to bedside. J Psychoactive Drugs 2010; 42: 133-145. https://doi.org/10.1080/02791072.2010.10400686
- Keser A, Yüksel A, Mutlu-Yeşiltepe G, Bayhan A, Özsu E, Hatun Ş. A new insight into food addiction in childhood obesity. Turk J Pediatr 2015; 57: 219-224.
- Gearhardt AN, Corbin WR, Brownell KD. Preliminary validation of the yale food addiction scale. Appetite 2009; 52: 430-436. https://doi.org/10.1016/j.appet.2008.12.003
- American Psychiatric Association (APA). Diagnostic and statistical manual of mental disorders (5th ed).Washington, DC: APA; 2013. https://doi.org/10.1176/appi.books.9780890425596
- Schroder R, Sellman JD, Adamson S. Development and validation of a brief Measure of Eating Compulsivity (MEC). Subst Use Misuse 2017; 52: 1918-1924. https://doi.org/10.1080/10826084.2017.1343352
- Pulat Demir H. Prevalence of obesity between 6-15 years children in Istanbul. İstanbul Gelişim University Journal of Health Sciences 2022; 17: 497-512. https://doi.org/10.38079/igusabder.1062876
- Alkan H, Enç N, Yeni K, Yıldız Ayvaz M, Kayıkcı EE, Kalkan Uğurlu Y. Evaluation of childhood obesity, prevalence, and related factors in Istanbul. Florence Nightingale J Nurs 2022; 30: 267-273. https://doi.org/10.5152/FNJN.2022.20106
- Alper Z, Ercan İ, Uncu Y. A meta-analysis and an evaluation of trends in obesity prevalence among children and adolescents in Turkey: 1990 through 2015. J Clin Res Pediatr Endocrinol 2018; 10: 59-67. https://doi.org/10.4274/jcrpe.5043
- Bayraktar F, Erkman F, Kurtuluş E. Adaptation study of Yale Food Addiction Scale. Bulletin of Clinical Psychopharmacology 2012; 22(Suppl. 1): S38.
- Taber KS. The use of Cronbach’s Alpha when developing and reporting research instruments in science education. Res Sci Educ 2018; 48: 1273-1296. https://doi.org/10.1007/s11165-016-9602-2
- Karakoç FY, Dönmez L. Basic principles of scale development. Tıp Eğitimi Dünyası 2014; 13: 39-49. https://doi.org/10.25282/ted.228738
- Meule A, Gearhardt AN. Food addiction in the light of DSM-5. Nutrients 2014; 6: 3653-3671. https://doi.org/10.3390/nu6093653
- Stabouli S, Erdine S, Suurorg L, Jankauskienė A, Lurbe E. Obesity and eating disorders in children and adolescents: the bidirectional link. Nutrients 2021; 13: 4321. https://doi.org/10.3390/nu13124321
- Golden NH, Schneider M, Wood C; Commitee on Nutiriton; Commitee on Adolesence; Section on Obesity. Preventing obesity and eating disorders in adolescents. Pediatrics 2016; 138: e20161649. https://doi.org/10.1542/peds.2016-1649
- Jebeile H, Lister NB, Baur LA, Garnett SP, Paxton SJ. Eating disorder risk in adolescents with obesity. Obes Rev 2021; 22: e13173. https://doi.org/10.1111/obr.13173
- Schag K, Schönleber J, Teufel M, Zipfel S, Giel KE. Food-related impulsivity in obesity and binge eating disorder-a systematic review. Obes Rev 2013; 14: 477-495. https://doi.org/10.1111/obr.12017
- Davis C. Compulsive overeating as an addictive behavior: overlap between food addiction and binge eating disorder. Curr Obes Rep 2013; 2: 171-178. https://doi.org/10.1007/s13679-013-0049-8
- Zachar P, First MB, Kendler KS. Revising substance-related disorders in the DSM-5: a history. J Stud Alcohol Drugs 2022; 83: 99-105.
- Koreshe E, Paxton S, Miskovic-Wheatley J, et al. Prevention and early intervention in eating disorders: findings from a rapid review. J Eat Disord 2023; 11: 38. https://doi.org/10.1186/s40337-023-00758-3
- Mills R, Hyam L, Schmidt U. Early intervention for eating disorders. Curr Opin Psychiatry 2024; 37: 397-403. https://doi.org/10.1097/YCO.0000000000000963
- Peebles R, Sieke EH. Medical complications of eating disorders in youth. Child Adolesc Psychiatr Clin N Am 2019; 28: 593-615. https://doi.org/10.1016/j.chc.2019.05.009
- Akgül S, Pehlivantürk Kızılkan M, Yıldırım A, Derman O. Prevalence of suicide attempt, suicide ideation and self-harm at diagnosis in adolescents with eating disorders. Int J Psychiatry Clin Pract 2024; 28: 63-67. https://doi.org/10.1080/13651501.2024.2337796
Copyright and license
Copyright © 2025 The Author(s). This is an open access article distributed under the Creative Commons Attribution License (CC BY), which permits unrestricted use, distribution, and reproduction in any medium or format, provided the original work is properly cited.















