Graphical Abstract
Abstract
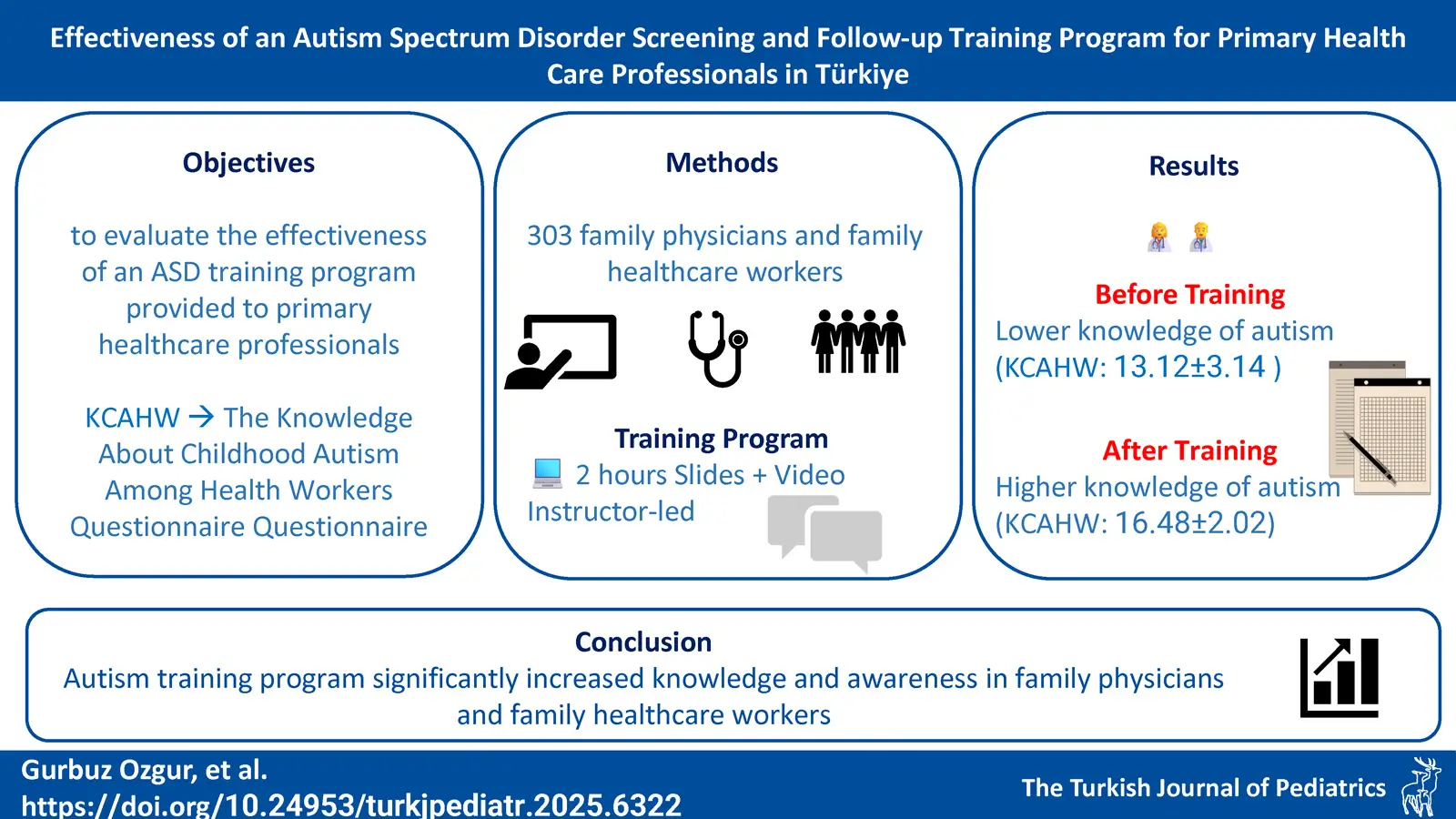
Background. Autism spectrum disorder (ASD) screening and follow-up programs are implemented in all provinces in Türkiye as part of the National Action Plan for Individuals with ASD. Primary health care professionals are trained regarding ASD by child and adolescent psychiatrists, aiming to ensure that risky children are diagnosed and referred earlier and diagnosed in early childhood. The aim of this study is to objectively evaluate the effectiveness of an ASD training program provided to primary healthcare professionals.
Methods. Three hundred and three individuals consisting of family physicians and family healthcare workers (FHW) who participated in the ASD training program were recruited in the study in the Muğla province of Türkiye. The Knowledge About Childhood Autism Among Health Workers Questionnaire (KCAHW) was completed by all participants before and after the training.
Results. The mean total KCAHW scores pre- and post-training were 13.12±3.14 and 16.48±2.02, respectively. There was a statistically significant difference in Domains 1, 2, 3, and 4 and the total scores pre- and post-training (p<0.001). The effect sizes of the differences in KCAHW domains 1, 2, 3, 4, and the total score for family physicians and FHWs’ pre- and post-test means were 0.24, 0.01, 0.08, 0.14, and 0.22, respectively.
Conclusions. Family physicians and the FHWs benefited from the intervention in all domains of the KCAHW. The training program provided within the scope of the ASD screening and follow-up program significantly increased knowledge and awareness of ASD in primary healthcare providers.
Keywords: autism spectrum disorder, general practitioners, primary care physicians, screening, training
Introduction
Autism spectrum disorder (ASD) is a neurodevelopmental disorder that emerges in early childhood. In DSM-5, ASD is categorized into two main domains: deficits in social communication and interaction and restricted, repetitive patterns of behavior, interests, or activities.1 Recent studies have focused on predictors of loss of autism diagnosis and have demonstrated the impact of early diagnosis and intervention.2-5 The most important step towards diagnosis is recognizing the early signs of ASD and referring the child to a child and adolescent psychiatrist for further evaluation. However, the age of diagnosis remains suboptimal. According to the results of a meta-analysis study, the mean age of ASD diagnosis was determined as 60.48 months.6
In a recent review examining the impact of implemented policies on early diagnosis of autism, it was found that both screening models and training programs increased early diagnosis.7 The American Academy of Pediatrics recommends that all children aged 18-24 months be screened for ASD symptoms.8 Today, some countries have implemented nationwide screening programs to facilitate the early detection of ASD.9-12 In addition to increasing ASD awareness among healthcare professionals, studies are recommended to raise awareness of risk symptoms of autism in children in all environments where they come into contact with children, such as schools13 and among parents.14,15 A study conducted in the United States emphasizes that early autism diagnosis is shaped by diverse state-level screening practices, early intervention efforts, and existing disparities, suggesting that refining national and state policies is essential to support timely identification and access to services.16 Countries are trying to produce and implement health policies for the early diagnosis of autism. In Türkiye, the Autism Spectrum Disorder Screening and Follow-up Program is conducted by the Ministry of Health under the National Action Plan for Individuals with Autism Spectrum Disorder, ensuring that all children aged 18-36 months are screened for ASD symptoms.17,18 As part of this program, family physicians are required to evaluate children aged 18-36 months at least once for ASD risk. In the literature, various studies have assessed the knowledge of physicians and other healthcare professionals about ASD. However, a significant portion of these studies indicate that levels of knowledge are either insufficient or lower than expected.19-21 Research suggests that postgraduate training on ASD significantly enhances awareness and knowledge.22-25 This is particularly important for primary healthcare professionals and pediatric clinic staff, as they have a greater chance of encountering children aged 18-36 months and hence identifying ASD risk at an early stage.
The aim of this study is to evaluate the effectiveness of ASD training provided to primary healthcare workers on their knowledge on ASD.
Materials and Methods
Ethics and consent
The study was conducted in compliance with the principles of the Declaration of Helsinki Ethical Principles for Medical Research Involving Human Participants. Approval was obtained from the Muğla Provincial Directorate of Health and the Muğla Sıtkı Koçman University Human Research Ethics Committee (180171/150). All participants who volunteered to the study were provided with detailed verbal information regarding the study and the procedures involved, and written informed consent was obtained.
Study sample
A total of 303 family physicians and family healthcare workers (FHWs) employed in family health centers and social health centers who had received ASD training and participated in the ASD Screening and Follow-up Program organized by the Ministry of Health in Muğla city and its districts between November 1, 2018, and February 1, 2019, were included in the study.
Family physicians and FHWs who had previously participated in the Turkish validity and reliability study of the “Knowledge About Childhood Autism Among Health Workers Questionnaire” (KCAHW) in Muğla were excluded from the study. The KCAHW was administered to participants before and after the training to assess changes in their knowledge.
Training content
Each training session consisted of a maximum of 20 participants and lasted approximately 2 hours. The sessions were held in a meeting room supplied with a computer and projector. Pen and paper questionnaires were given to participants before the training and given again after the training ended. The training sessions were conducted interactively by the same child and adolescent psychiatrist and included:
- A brief slide presentation prepared by the Ministry of Health, covering theoretical information on ASD, including its definition, diagnostic criteria, etiopathogenesis, frequency, social-emotional and language development stages in typically developing children, autism symptoms, prognosis, course and treatment.
- A video presentation illustrating case examples of ASD. These were videos of children from different age groups, shot in the presence of a child psychiatrist and parents in an examination environment, showing the symptoms of normal development and autism (such as stereotypy, speech delay) and the findings detected during the examination (such as calling out to one’s name, eye contact, joint attention, imitation games).18
Data collection tools
Sociodemographic data form: Participants completed a questionnaire designed by the researchers to assess their sociodemographic and occupational characteristics.
The Knowledge About Childhood Autism Among Health Workers Questionnaire (KCAHW): KCAHW, developed by Bakare et al., consists of 19 items.26 This questionnaire is used to measure health workers’ knowledge of ASD and evaluates four domains related to autism:
- Social Interaction Deficits (8 items) – Evaluates impairments in social interaction observed in children with ASD.
- Communication and Language Development (1 item) – Assesses symptoms related to communication and language skills.
- Repetitive and Stereotypical Behaviors (4 items) – Examines obsessive-compulsive tendencies, repetitive actions, and stereotypical behavioral characteristics of ASD.
- General Knowledge About Autism (6 items) – Covers autism as a disorder, its possible comorbid conditions, and the typical age of onset.
The total score from the questionnaire ranges between 0 and 19. Response options were categorized as “I don’t know,” “Yes,” and “No,” with correct answers scoring 1 point and incorrect responses receiving 0 points. In Domain 4, three items were reverse-scored. The total score of the scale consists of the sum of the four domain scores. Higher scores indicate greater knowledge of ASD.
The mean scale score in the studied population reflects the overall knowledge level of childhood ASD within that group. The Turkish validity and reliability of the KCAHW was established by Gürbüz Özgür et al.27
Data analysis
Descriptive statistics are presented as mean, median, standard deviation, number, and percentage. The normality of the distribution was assessed using the Shapiro-Wilk test. Pre- and post-training scale domain scores were compared using the Wilcoxon signed- ranks test due to failure to provide conditions of normal distribution conditions, and Cohen’s effect size (ES) statistics was also used in the comparisons. In brief, ES was calculated with the “(Group 1 Mean - Group 2 Mean)/ Pooled Standard Deviation” formula.28
Confounding and effect-modifier variables were determined with the stratified analysis method by using Wilcoxon signed- ranks tests. Since neither the dependent nor independent variables were dichotomous, certain conditions were used instead of using the Mantel-Haenszel analysis to determine confounding or effect-modifier variables.
Criteria for identifying confounding and effect-modifying variables
Condition 1: If a significant result is achieved in the p<0.05 level in the hypothesis test during the before-after comparison which is done before the related independent variable is categorized and if the before-after analyses done (stratified) for all the sub-categories of the same variable are significant at the p<0.05 level, then this variable is neither confounding, nor is an effect modifier.
Condition 2: For a variable to be accepted as a “confounding variable,” the before-after comparison done before the independent variable is categorized needs to be significant at the p<0.05 level; a “non-significant” result should be achieved at the p<0.05 level in all the strata of the related variable in the stratified analyses (or in the before-after analyses for all the sub-categories of the same variable).
Condition 3: For a variable to be accepted as an “effect modifier variable,” the before-after comparison done before the independent variable is categorized needs to significant at the p<0.05 level; “significant” result should be achieved in the p<0.05 level in one of strata of the related variable and “non-significant” in another stratum in the stratified analyses (or in the before-after analyses for all the sub-categories of the same variable).
The data were analyzed using SPSS Version 17.00 for Windows (Chicago: SPSS Inc., 2008). For statistical significance, a type 1 error (p-value) threshold of 0.05 was applied.
Results
A total of 303 participants were included in the study, of whom 197 were female and 106 were male. Among them, 48.2% (n=146) were family physicians, while 51.8% were FHWs, including midwives, nurses, and health officers.
The mean age of the participants was 43.2 ± 8.49 years, with an average number of children of 1.4 ± 0.82. The mean duration of work experience in the field was 20.18 ± 8.66 years (ranging from 0 to 46 years). The sociodemographic characteristics of the health workers included in the study are presented in Table I. Among the family physicians, 7% had completed a child psychiatry internship during their medical training.
| ASD: autism spectrum disorder. | ||
| Table I. The sociodemographic characteristics of the participants | ||
|
|
||
| Gender | Female |
|
| Male |
|
|
| Occupation | Family physician |
|
| Family healthcare worker |
|
|
| Physician’s specialty | Practitioner |
|
| Family physician specialist |
|
|
| Unknown |
|
|
| Educational status | High-school |
|
| Undergraduate |
|
|
| Graduate |
|
|
| Post-graduate |
|
|
| Doctorate/practice in medicine |
|
|
| Marital status | Married |
|
| Single/divorced |
|
|
| Income-expense level | Low |
|
| Medium |
|
|
| High |
|
|
| Unknown |
|
|
| Work history at a mental health center | Yes |
|
| No |
|
|
| Unknown |
|
|
| Child psychiatry internship | Yes |
|
| No |
|
|
| Unknown |
|
|
| Having child diagnosed with ASD | Yes |
|
| No |
|
|
| Having child with a chronic disease / disability | Yes |
|
| No |
|
|
| Child with ASD in one’s environment | Yes |
|
| No |
|
|
| Completed the follow-up of a child with ASD | Yes |
|
| No |
|
|
| Previous ASD training | Yes |
|
| No |
|
|
| Unknown |
|
|
| Perceived knowledge level | Insufficient |
|
| Medium |
|
|
| Sufficient |
|
|
| Unknown |
|
|
A statistically significant increase was observed in all domains and total scores of the KCAHW questionnaire administered before and after the training sessions (Table II). Additionally, family physicians and FHWs were compared in terms of pre- and post-training score differences across each domain (Table II). In this comparison, Cohen’s effect size was used. A significant difference between family physicians and FHWs was observed only in the first domain, where the effect size indicated a weak effect. In other words, physicians showed greater improvement in the first domain compared to FHWs, but no significant differences were found in the other domains.
| * Wilcoxon signed ranks test; ** Cohen's effect size (ES): (Group 1 Mean - Group 2 Mean) / Pooled Standard Deviation; *** Mann-Whitney U test |
||||||||
| Table II. The Knowledge About Childhood Autism Among Health Workers Questionnaire domains and total score means of the participants and their comparison before and after training | ||||||||
|
|
|
|
|
|
|
|
|
|
| Domain 1 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
| Domain 2 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
| Domain 3 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
| Domain 4 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
| Total score |
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
As a result of the stratified analysis, none of the independent variables were found to be confounding factors. However, for the 2nd domain, age, gender, marital status, income-expense level, years of experience in the field, and ASD knowledge perception level were identified as effect modifier variables (Table III). Participants’ correct response rates to the KCAHW scale items before and after the training are presented in Table IV.
| *p ≤ 0.001; **p between 0.001 and 0.05. | ||||||
| Table III. Results of stratified analysis for the Knowledge About Childhood Autism Among Health Workers Questionnaire domains (pre-test and post-test) | ||||||
| Possible confounding effect / effect modifier variable | Variable categories |
|
||||
|
|
|
|
|
|
||
| Age group (years) | <39 (n=95) |
|
|
|
|
|
| 40-45 (n=88) |
|
|
|
|
|
|
| 46+ (n=120) |
|
|
|
|
|
|
| Gender | Female (n=197) |
|
|
|
|
|
| Male (n=106) |
|
|
|
|
|
|
| Marital status | Married (n=247) |
|
|
|
|
|
| Single/divorced (n=56) |
|
|
|
|
|
|
| Income-expense level | Low (n=99) |
|
|
|
|
|
| Medium (n=106) |
|
|
|
|
|
|
| High (n=89) |
|
|
|
|
|
|
| Years working in the field (years) | 0-14 (n=79) |
|
|
|
|
|
| 15-24 (n=107) |
|
|
|
|
|
|
| 25+ (n=117) |
|
|
|
|
|
|
| Perceived knowledge level | Insufficient (n=138) |
|
|
|
|
|
| Medium (n=102) |
|
|
|
|
|
|
| Sufficient (n=54) |
|
|
|
|
|
|
| Occupation | Family physician (n=157) |
|
|
|
|
|
| Family healthcare worker (n=146) |
|
|
|
|
|
|
| Whole group (n=303) |
|
|
|
|
|
|
| Table IV. Correct response rates of family physicians and healthcare workers to the Knowledge About Childhood Autism Among Health Workers Questionnaire items before and after training | ||||
|
|
|
|||
|
|
|
|
|
|
| Domain 1 | ||||
| Item 1 |
|
|
|
|
| Item 2 |
|
|
|
|
| Item 3 |
|
|
|
|
| Item 4 |
|
|
|
|
| Item 5 |
|
|
|
|
| Item 6 |
|
|
|
|
| Item 7 |
|
|
|
|
| Item 8 |
|
|
|
|
| Domain 2 | ||||
| Item 9 |
|
|
|
|
| Domain 3 | ||||
| Item 10 |
|
|
|
|
| Item 11 |
|
|
|
|
| Item 12 |
|
|
|
|
| Item 13 |
|
|
|
|
| Domain 4 | ||||
| Item 14 |
|
|
|
|
| Item 15 |
|
|
|
|
| Item 16 |
|
|
|
|
| Item 17 |
|
|
|
|
| Item 18 |
|
|
|
|
| Item 19 |
|
|
|
|
Discussion
Primary healthcare workers interact with infants and children regularly during vaccination appointments and developmental follow-ups. During these visits, family physicians play a crucial role in identifying children at risk for ASD at an early stage through screening tests. As a result, various countries have implemented training programs for healthcare workers, including practicing physicians, within the framework of ASD action plans.10,11 In the literature, numerous studies using different assessment tools have reported that healthcare professionals’ knowledge of ASD is often insufficient.20 In our study, we evaluated ASD knowledge using KCAHW, and our findings are discussed below in relation to existing literature.
When analyzing intervention studies aimed at increasing knowledge levels on ASD, various training programs can be identified, including face-to-face education, computer-assisted distance learning, case-based education, intensive one-day training, and weekly or monthly repetitive sessions.20 In our study, a 2-hour theoretical training combined with video-based case presentations was implemented, as planned by the Ministry of Health. The findings revealed a significant increase in ASD knowledge levels among both family physicians and other primary healthcare workers following the training. Similarly, another training study conducted in Türkiye reported that family physicians’ knowledge levels improved after a 2-hour ASD training program.22 Additionally, Carbone et al. found that after training, the ASD screening rates of 26 primary physicians increased during their 18- to 24-month age group medical examinations.23 Studies evaluating the effectiveness of ASD training programs generally rely on researcher-developed questionnaires or assess differences in participants’ subjective perceptions. In contrast, we used the KCAHW measurement tool, which is internationally recognized for assessing training effectiveness. Therefore, our findings will allow for comparisons with other studies that have used the same measurement tool, contributing to a more standardized evaluation of ASD training programs. The knowledge level measured in the study measures the gains immediately after the training. The level of knowledge of health workers cannot be determined in the long term with this study alone. However, it is possible to see that this training is effective in our other study where we examined the number of children screened and referred by the same sample in the same province after the training and the rate of children diagnosed with autism.29
Eseigbe et al. used the KCAHW in their study to assess the ASD knowledge levels of physicians from different specialties and reported that 34% of 76 family physicians had a KCAHW mean total score above 15.30 Similarly, in Salama’s study, the KCAHW was administered to 70 family physicians, revealing a mean score of 11.2 ± 3.5 In a study by Eray and Murat, it was found that 65.3% of family physicians lacked sufficient knowledge about ASD.22 In contrast, in our study, only 17.8% of family physicians reported that they did not have a sufficient level of knowledge. Additionally, in a study by Gürbüz Özgür et al. on primary healthcare workers, 21.3% of participants perceived their ASD knowledge as sufficient or highly sufficient.27 In our study, 16.5% of participants had received prior training on ASD. Similarly, a study conducted in the United Kingdom reported that approximately two-thirds of practitioners had not received any ASD training during their medical school training or family physician specialization training.31 In our study, it was found that only 7% of physicians had completed an internship in child psychiatry during their medical training, while 11.9% of all participants (nurses, midwives, and other health workers as well as physicians) had undergone internship training in child psychiatry.
Since theoretical and practical training related to ASD diagnosis is typically provided during child psychiatry internships, we believe that incorporating ASD-focused lectures into the education curriculum of all healthcare-related disciplines could be an effective strategy for enhancing knowledge levels after graduation. In another study conducted among senior students of medical, nursing, and psychology faculties, the mean KCAHW score was 10.67 ± 3.73 overall, with faculty-specific scores as follows: 12.24 ± 3.24 for medical students, 10.76 ± 3.5 for nursing students, 9.01 ± 3.76 for psychology students.32 This study found that KCAHW scores had a positive relationship with both the number of weeks spent in psychiatry and pediatrics rotations and the number of psychiatry/abnormal psychology course hours.32 These findings emphasize the importance of integrating ASD-related training into both pre- and post-graduate curricula to enhance knowledge and awareness. The study also evaluated the impact of the training program on primary healthcare workers, who were the main target audience. The results showed that while both family physicians and FHWs benefited equally across all domains, including total scores, family physicians demonstrated a significantly greater improvement in Domain 1 when effect size was analyzed. One possible explanation for this finding is that Domain 1 contains the highest number of items and is primarily based on clinical observation. Additionally, physicians frequently encounter differential diagnosis scenarios, which may have led them to reframe their past knowledge and clinical observations in light of the new training. Since the scale applied in the study was not developed to directly evaluate the effectiveness of the training, the lack of a high increase in the response rates (in Domain 4 items) to some information not included in the content of the training (e.g. comorbidity, detailed etiology) suggests that this training corresponds to greater gains, especially in domains 1, 2 and 3 of KCAHW (Table IV). This information may provide practical implications for future program development and policy planning.
This study found that none of the analyzed independent variables were confounding factors for KCAHW scores. However, in Domain 2, age, gender, marital status, income-expense level, years of work experience, and ASD knowledge perception level were identified as effect modifier (moderator) variables. As is well known, the absence of confounding variables suggests that the obtained results are robust and reliable without requiring additional multiple analyses. However, effect modifier variables cannot be controlled through statistical adjustments; they can only be reported, as was done in this study. Given that multiple variables influenced Domain 2, we recommend interpreting the results with caution in this domain. Domain 2 of the scale consists of a single item. This item asks whether the respondents know that patients with ASD have a speech delay problem. We see that a significant majority of the respondents (both family physicians and FHW) knew this before the educational intervention. The vast majority of health workers knew this before the intervention, and very few did not. In the subcategories of the independent variables, the number of those who did not know decreased further. In the research sample, this homogeneity (the overwhelming majority of respondents knowing the subject before the educational intervention) is also due to the fact that the 2nd Domain in the scale was questioned with only one question. There is no such homogeneity in any of the other dimensions because the other dimensions were questioned with at least 4 items.
Among the strong points of our study, we can highlight the following: Objective measurement of training effectiveness using a validated and reliable questionnaire in Turkish; a large sample size, enhanced statistical power due to minimized variability, as the same trainer conducted all sessions, reducing potential bias.
Limitations
The study also has some limitations: Knowledge assessment was conducted immediately after the training, without a follow-up evaluation to measure long-term knowledge retention. Although our findings demonstrate strong internal validity, a regionally confined sample may limit the generalizability of results to the broader population of trained professionals across the country.
In developing countries, educational initiatives on ASD remain insufficient compared to Western countries.33 Determining which educational interventions are most effective is challenging. Factors such as the use of different training groups, cultural variations, and the lack of standardized measurement tools make direct comparisons difficult.
Conclusion
The ASD Screening and Follow-up Program is currently being implemented nationwide in Türkiye. Although our study showed an increase in level of knowledge immediately after the training, studies are needed to evaluate the knowledge levels in the long term. Examining the long-term effects of increase in knowledge levels of family physicians and other primary healthcare workers with data sources, such as referral statistics, diagnostic outcomes, or follow-up assessments over time, will yield objective results. We believe that this study will contribute to future research evaluating the effectiveness of ASD training programs, both in Türkiye and internationally.
Ethical approval
The study was approved by Muğla Provincial Directorate of Health and the Muğla Sıtkı Koçman University Human Research Ethics Committee (180171/150).
Source of funding
The authors declare the study received no funding.
Conflict of interest
The authors declare that there is no conflict of interest.
References
- American Psychiatric Association, DSM-5 Task Force. Diagnostic and statistical manual of mental disorders: DSM-5. 5th ed. Washington, DC: American Psychiatric Association; 2013: xliv, 947. https://doi.org/10.1176/appi.books.9780890425596
- Filipek PA, Accardo PJ, Ashwal S, et al. Practice parameter: screening and diagnosis of autism: report of the Quality Standards Subcommittee of the American Academy of Neurology and the Child Neurology Society. Neurology 2000; 55: 468-479. https://doi.org/10.1212/wnl.55.4.468
- Helt M, Kelley E, Kinsbourne M, et al. Can children with autism recover? If so, how? Neuropsychol Rev 2008; 18: 339-366. https://doi.org/10.1007/s11065-008-9075-9
- Wiggins LD, Baio J, Schieve L, Lee LC, Nicholas J, Rice CE. Retention of autism spectrum diagnoses by community professionals: findings from the autism and developmental disabilities monitoring network, 2000 and 2006. J Dev Behav Pediatr 2012; 33: 387-395. https://doi.org/10.1097/DBP.0b013e3182560b2f
- Mukaddes NM, Tutkunkardas MD, Sari O, Aydin A, Kozanoglu P. Characteristics of children who lost the diagnosis of autism: a sample from İstanbul, Turkey. Autism Res Treat 2014; 2014: 472120. https://doi.org/10.1155/2014/472120
- van ‘t Hof M, Tisseur C, van Berckelear-Onnes I, et al. Age at autism spectrum disorder diagnosis: a systematic review and meta-analysis from 2012 to 2019. Autism 2021; 25: 862-873. https://doi.org/10.1177/1362361320971107
- Lindly OJ, Abate DJ, Park HJ, et al. The influence of policy on early diagnosis and other autism services: a narrative review. Rev J Autism Dev Disord 2024. https://doi.org/10.1007/s40489-023-00423-0
- Johnson CP, Myers SM; American Academy of Pediatrics Council on Children with Disabilities. Identification and evaluation of children with autism spectrum disorders. Pediatrics 2007; 120: 1183-1215. https://doi.org/10.1542/peds.2007-2361
- Nygren G, Sandberg E, Gillstedt F, Ekeroth G, Arvidsson T, Gillberg C. A new screening programme for autism in a general population of Swedish toddlers. Res Dev Disabil 2012; 33: 1200-1210. https://doi.org/10.1016/j.ridd.2012.02.018
- Wallace S, Fein D, Rosanoff M, et al. A global public health strategy for autism spectrum disorders. Autism Res 2012; 5: 211-217. https://doi.org/10.1002/aur.1236
- Pasco G, Clark B, Dragan I, et al. A training and development project to improve services and opportunities for social inclusion for children and young people with autism in Romania. Autism 2014; 18: 827-831. https://doi.org/10.1177/1362361314524642
- Shahrokhi H, Ghiasi A, Gholipour K, Fanid LM, Shamekhi HR, Iezadi S. Considerations about the implementation of an autism screening program in Iran from the viewpoints of professionals and parents: a qualitative study. BMC Psychiatry 2021; 21: 55. https://doi.org/10.1186/s12888-021-03061-0
- Khound M, Ghosh S, Kaushik JS. Enhancing skills for early detection and management of autism in schools. Indian J Pediatr 2024; 91: 1203. https://doi.org/10.1007/s12098-024-05199-7
- Vasudevan V, Nagel A, Thompson LA. What parents need to know about autism screening and early treatment. JAMA Pediatr 2024; 178: 844. https://doi.org/10.1001/jamapediatrics.2024.1324
- Rochyadi E, Wulandari R, Manar M, Sunanda E, Yuliana Y. Designing program to improve parent’s awareness towards autism child. Advanced Science Letters 2019; 25: 158-161. https://doi.org/10.1166/asl.2019.13209
- Lindly OJ, Abate D, Fuchu PL, et al. The impact of state policy on early autism diagnosis: a qualitative investigation. Autism 2025; 29: 2163-2180. https://doi.org/10.1177/13623613251336813
- T.C. Resmi Gazete. Otizm Spektrum Bozukluğu Olan Bireylere Yönelik Ulusal Eylem Planı (2016-2019). Ankara: Başbakanlık Basımevi; 2016. Available at: https://www.resmigazete.gov.tr/eskiler/2016/12/20161203-16.htm
- Dursun OB, Turan B, Öğütlü H, et al. A new model for recognition, referral, and follow-up of autism spectrum disorder: a nationwide program. Autism Research 2022; 15: 1961-1970. https://doi.org/10.1002/aur.2813
- Abubakar A, Ssewanyana D, Newton CR. A Systematic review of research on autism spectrum disorders in Sub-Saharan Africa. Behav Neurol 2016; 2016: 3501910. https://doi.org/10.1155/2016/3501910
- McCormack G, Dillon A, Healy O, Walsh C, Lydon S. Primary care physicians’ knowledge of autism and evidence-based interventions for autism: a systematic review. Rev J Autism Dev Disord 2020; 7: 226-241. https://doi.org/10.1007/s40489-019-00189-4
- Harrison AJ, Slane MM, Hoang L, Campbell JM. An international review of autism knowledge assessment measures. Autism 2017; 21: 262-275. https://doi.org/10.1177/1362361316638786
- Eray S, Murat D. Effectiveness of autism training programme: an example from Van, Turkey. J Pak Med Assoc 2017; 67: 1708-1713.
- Carbone PS, Norlin C, Young PC. Improving early identification and ongoing care of children with autism spectrum disorder. Pediatrics 2016; 137: e20151850. https://doi.org/10.1542/peds.2015-1850
- Bordini D, Lowenthal R, Gadelha A, Araujo Filho GM, Mari Jde J, Paula CS. Impact of training in autism for primary care providers: a pilot study. Braz J Psychiatry 2015; 37: 63-66. https://doi.org/10.1590/1516-4446-2014-1367
- Major NE, Peacock G, Ruben W, Thomas J, Weitzman CC. Autism training in pediatric residency: evaluation of a case-based curriculum. J Autism Dev Disord 2013; 43: 1171-1177. https://doi.org/10.1007/s10803-012-1662-1
- Bakare MO, Ebigbo PO, Agomoh AO, Menkiti NC. Knowledge about childhood autism among health workers (KCAHW) questionnaire: description, reliability and internal consistency. Clin Pract Epidemiol Ment Health 2008; 4: 17. https://doi.org/10.1186/1745-0179-4-17
- Gürbüz Özgür B, Aksu H, Eser E. Validity and reliability of the Turkish version of the knowledge about childhood autism among health workers questionnaire. Psychiatry and Clinical Psychopharmacology 2019; 29: 765-773. https://doi.org/10.1080/24750573.2019.1637326
- Cohen J. Statistical power analysis for the behavioural sciences. 2nd ed. Hillsdale, New Jersey: Lawrence Erlbaum Associates; 1988.
- Gurbuz Ozgur B, Aytac H. Outcomes of autism spectrum disorder screening and follow-up program in a sample of Turkey. Psychiatry and Clinical Psychopharmacology 2020; 30: 241-247. https://doi.org/10.5455/PCP.20200507075604
- Eseigbe EE, Nuhu FT, Sheikh TL, Eseigbe P, Sanni KA, Olisah VO. Knowledge of childhood autism and challenges of management among medical doctors in Kaduna State, Northwest Nigeria. Autism Res Treat 2015; 2015: 892301. https://doi.org/10.1155/2015/892301
- Unigwe S, Buckley C, Crane L, Kenny L, Remington A, Pellicano E. GPs’ confidence in caring for their patients on the autism spectrum: an online self-report study. Br J Gen Pract 2017; 67: e445-e452. https://doi.org/10.3399/bjgp17X690449
- Igwe MN, Bakare MO, Agomoh AO, Onyeama GM, Okonkwo KO. Factors influencing knowledge about childhood autism among final year undergraduate medical, nursing and psychology students of University of Nigeria, Enugu State, Nigeria. Ital J Pediatr 2010; 36: 44. https://doi.org/10.1186/1824-7288-36-44
- Sengupta K, Lobo L, Krishnamurthy V. Educational and behavioral interventions in management of autism spectrum disorder. Indian J Pediatr 2017; 84: 61-67. https://doi.org/10.1007/s12098-015-1967-0
Copyright and license
Copyright © 2025 The Author(s). This is an open access article distributed under the Creative Commons Attribution License (CC BY), which permits unrestricted use, distribution, and reproduction in any medium or format, provided the original work is properly cited.