Graphical Abstract
Abstract
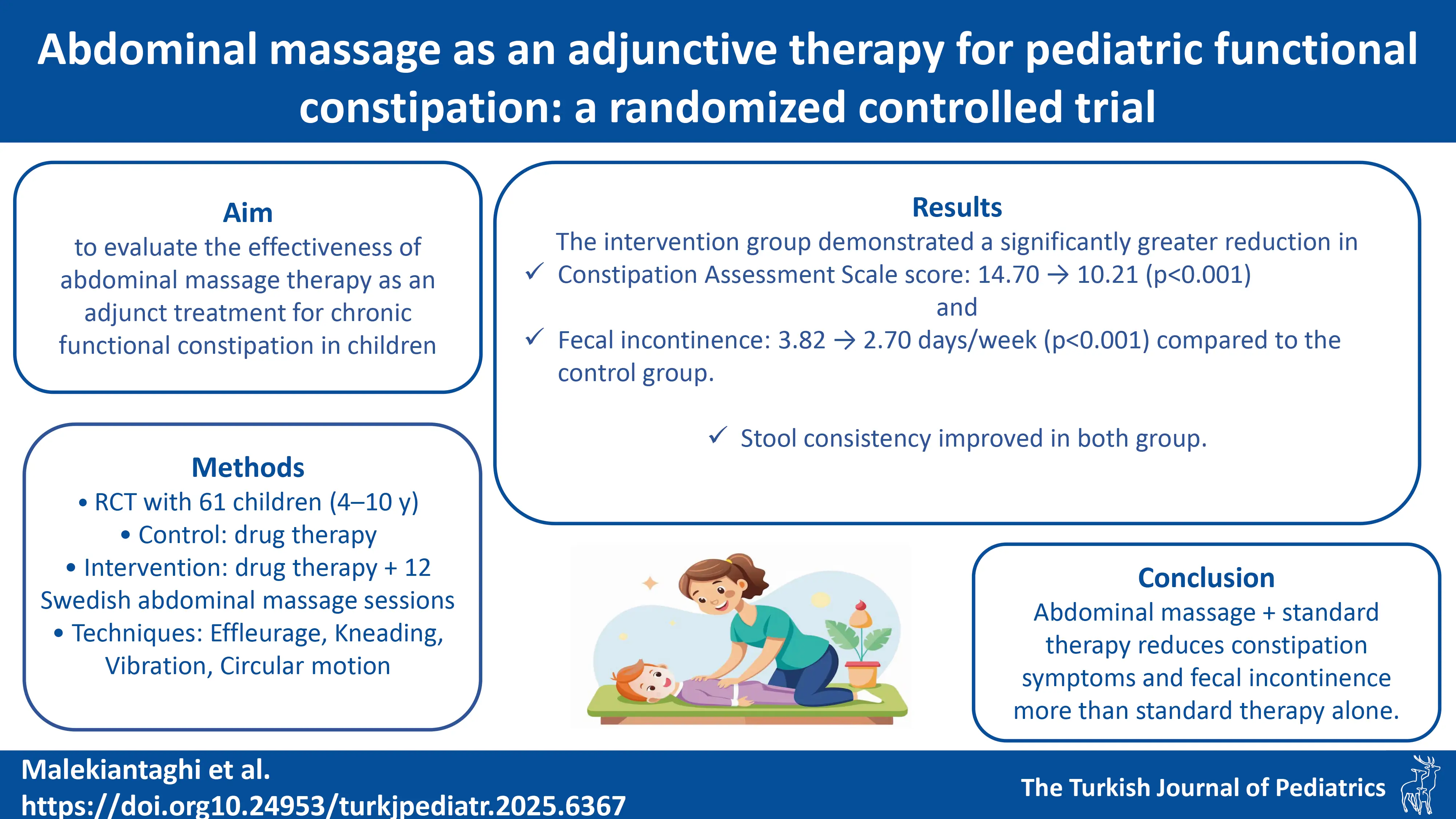
Background. Chronic functional constipation affects approximately 3% of children globally, leading to painful defecation, fecal incontinence, and abdominal discomfort. Abdominal massage may improve gastrointestinal motility by stimulating vagal activity and reducing abdominal muscle tension. This study aimed to evaluate the effectiveness of abdominal massage therapy as an adjunct treatment for chronic functional constipation in children.
Methods. This randomized controlled trial included 61 children aged 4–10 years (mean age 6.36 ± 1.77) diagnosed with functional constipation. Participants were randomly assigned to two groups: the control group, receiving standard drug therapy, and the intervention group, receiving 12 sessions of Swedish abdominal massage involving effleurage and gentle pressing, vibration of the small and large intestines, kneading of the abdomen, and clockwise circular movements in addition to drug treatment. Outcomes assessed included stool consistency (using the Bristol Stool Scale), constipation severity (measured by the Constipation Assessment Scale), and associated symptoms.
Results. Both groups showed improvements in stool consistency; however, no statistically significant difference was found between them. The intervention group demonstrated a significantly greater reduction in constipation symptoms (Constipation Assessment Scale scores decreased from 14.70 ± 1.29 to 10.21 ± 1.45, P < 0.001.) and fewer episodes of fecal incontinence (from 3.82 ± 1.33 to 2.70 ± 1.33 days/week, P < 0.001) compared to the control group.
Conclusion. A 12-session abdominal massage therapy program appears to be an effective adjunct treatment to standard pharmacological therapy for alleviating constipation-related symptoms in children. Larger, multicenter trials are needed to confirm these findings.
Keywords: Swedish abdominal massage, children, chronic constipation, functional constipation, Bristol Stool Scale, Constipation Assessment Scale
Introduction
Chronic functional constipation is one of the most common gastrointestinal disorders in children, with a global prevalence ranging from 7% to 30%. It often presents with symptoms such as painful defecation, abdominal discomfort, fecal incontinence, bloating, and reduced appetite. These symptoms can significantly impair a child’s physical, emotional, and social well-being, interfering with daily activities, school performance, and peer relationships. Constipation accounts for approximately 3–5% of general pediatric consultations and 10–25% of referrals to pediatric gastroenterologists.1-5
The management of chronic constipation typically involves pharmacological and non-pharmacological approaches. Pharmacological interventions include the use of laxatives such as stimulant laxatives, stool softeners, and fiber supplements, though long-term use may result in side effects and dependency.6,7 Non-pharmacological approaches aim to modify diet and behavior and include increased fiber and water intake, behavioral therapy, and complementary methods such as abdominal massage.8-12 Abdominal massage has been proposed as a supportive therapy that enhances colonic motility and facilitates bowel movements. Its physiological mechanism is thought to involve stimulation of the parasympathetic nervous system and vagal activity, leading to improved colonic transit and reduced fecal retention.13-15 Furthermore, it may help reduce dependence on laxatives and improve comfort during defecation.16-19 Despite emerging evidence, abdominal massage therapy remains underexplored as a treatment for chronic functional constipation in children. High-quality randomized controlled trials are needed to determine its efficacy as a supportive therapy in children with functional constipation.
This study aims to assess the effectiveness of abdominal massage therapy as an adjunct pharmacological treatment for chronic functional constipation in children, based on a randomized controlled trial conducted at Bahrami Children’s Hospital.
Materials and Methods
Study design and participants
This randomized controlled trial was conducted to assess the effects of abdominal massage therapy on children aged 4 to 10 years diagnosed with chronic functional constipation. Participants were recruited from the pediatric gastroenterology clinic at Bahrami Children’s Hospital between 2022 and 2023. Diagnosis was confirmed according to the Rome IV criteria for functional constipation.5,19 Written informed consent was obtained from the parent or legal guardian of each participant.
Inclusion and exclusion criteria
Children were eligible if they experienced fewer than three spontaneous bowel movements per week, exhibited symptoms such as painful defecation, large-diameter stools, fecal incontinence, and difficulty during bowel movements. Exclusion criteria included metabolic, endocrine, or anatomical causes of constipation, neurological disorders, Hirschsprung’s disease, severe systemic diseases (liver, kidney, heart), and current use of medications that may interfere with bowel function.
Sample size calculation
Sample size was calculated based on a power analysis from a previous study by Van et al.20,21 considering a power of 80%, a confidence interval of 95%, and an improvement rate of 63% in the control group and 93% in the intervention group. The calculated sample size was 26 per group, resulting in a total of 28 participants in the control group and 33 participants in the intervention group.
Intervention protocol
Eligible participants were randomly assigned to either the control or intervention group using a Google Random Generator software to ensure equal allocation. The randomization process was not blinded, and both the participants and researchers were aware of group assignments. To minimize potential bias resulting from the lack of blinding, outcome assessors and data analysts were blinded to group allocation. All statistical analyses were conducted using de-identified and coded data. The control group received standard medical care, which included laxatives (polyethylene glycol) at a dose of 0.5 g/kg, adjusted based on individual needs. The intervention group received 12 sessions of Swedish abdominal massage therapy, in addition to the same drug treatment. The massage sessions were conducted twice a week for six weeks by a trained therapist with over four years of pediatric massage experience. This therapy involved Swedish abdominal massage, following a protocol described by Sinclair.22 Daily dietary intake of all participants was documented using food diaries throughout the study. Although no formal statistical comparison of dietary fiber or fluid intake was conducted between the groups, all participants and their families received standardized dietary advice. This included recommendations for adequate intake of fruits, vegetables, and fluids, and the avoidance of low-fiber foods and unhealthy snacks. Families were instructed not to make major dietary changes during the study or use dietary supplements unless approved by the study clinicians. We monitored the diet by reviewing the food diaries weekly. Laxative was administered based on each child’s clinical requirement, with the frequency monitored through follow-up consultations. Adverse events were monitored throughout the study using standardized forms completed by caregivers and verified by study clinicians. Events were classified as mild, moderate or severe based on predefined criteria.
Outcome measures
Primary outcomes included stool consistency, assessed using the Bristol Stool Scale (BSS)23, which categorizes stool types from 1 (hard lumps, severe constipation) to 7 (watery, severe diarrhea)24; and the severity of constipation symptoms, assessed using the Constipation Assessment Scale (CAS).25 CAS is a validated tool consisting of 8 items, each scored from 0 to 2. The total score ranges from 0 (no symptoms) to 16 (most severe symptoms). Higher scores indicate greater severity of constipation-related complaints, such as painful or infrequent defecation, bloating, and straining. The scale was completed at baseline and post-intervention to evaluate changes in symptom severity.25 Secondary outcomes included the frequency of fecal incontinence and the time until initiation of bowel movements. Symptoms were also monitored by evaluating straining, painful defecation, and withholding behavior.
Statistical analysis
All data were analyzed using SPSS version 22. Descriptive statistics, including means (± standard deviation) for continuous variables and frequencies (percentages) for categorical variables, were computed. The chi-square test was used for categorical data, and repeated measures ANOVA was performed to analyze differences in primary outcomes between groups over time. Non-parametric tests were applied for non-normal distributions. A p-value of less than 0.05 was considered statistically significant. All statistical analyses were conducted by analysts blinded to group allocation.
Ethical considerations
The study was approved by the Research Council of the Faculty of Medicine at Tehran University of Medical Sciences, and the ethical code (IR.TUMS.MEDICINE.REC.1401.268) was obtained. The study was also registered in the Iranian Registry of Clinical Trials (IRCT20230929059549N1). Informed consent was obtained from the parents or legal guardians, and confidentiality of patient information was maintained throughout the study. The research adhered to the ethical guidelines outlined in the Declaration of Helsinki.
Results
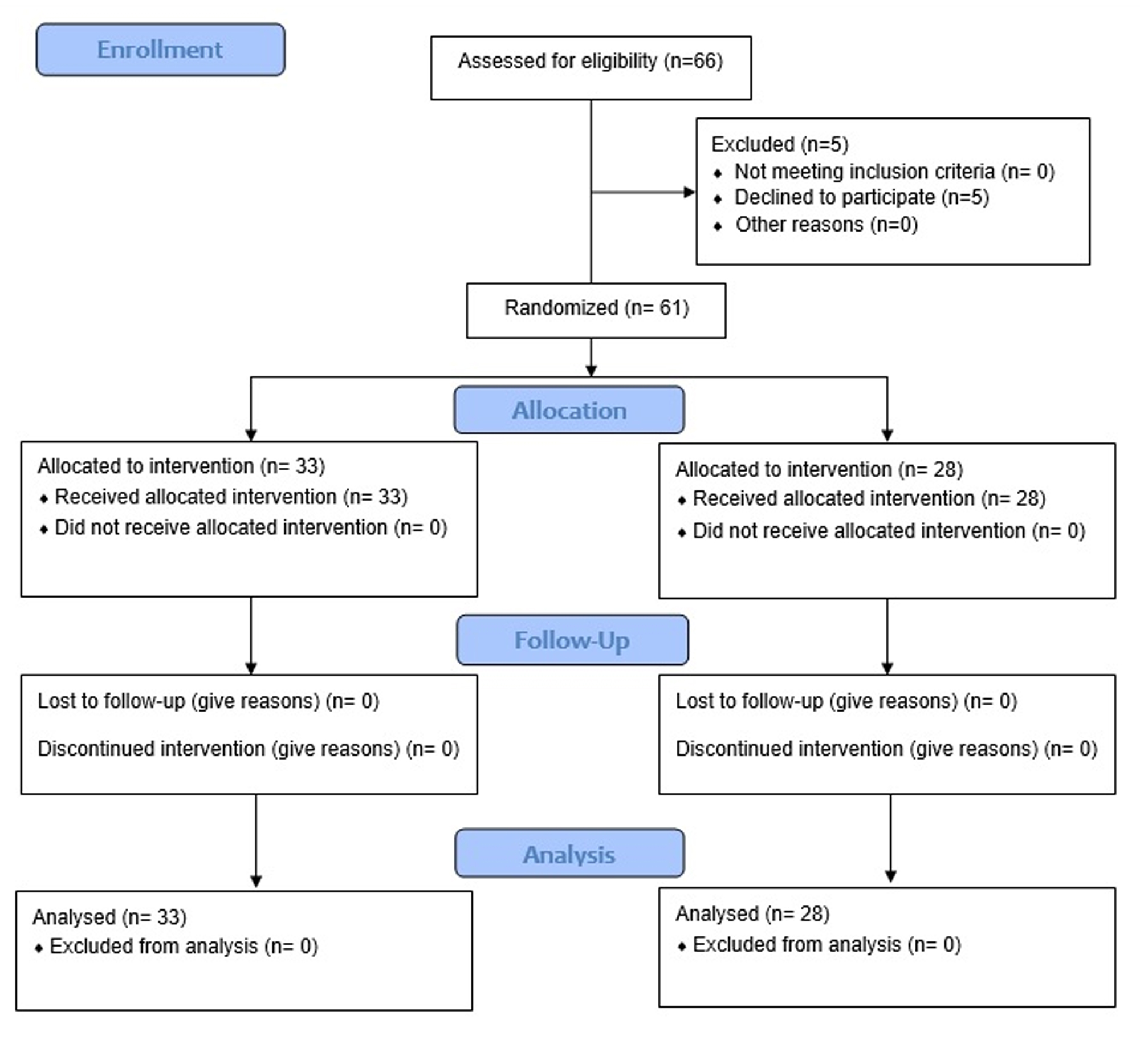
A total of 66 participants were enrolled in the study with parental consent, with 5 children discontinuing participation (Fig. 1). The baseline demographic and clinical characteristics, including age, gender, height, and weight, showed no significant differences between the control and intervention groups (P > 0.05), indicating balanced allocation (Table I). Among the 61 participants, 41% were female and 59% were male, with an average age of 6.36 ± 1.77 years.
| Table I. Demographic characteristics of participants | ||||
| Characteristic |
(n=61) |
(n=28) |
(n=33) |
|
| Age (years) |
|
|
|
|
| Female gender |
|
|
|
|
| Height (cm) |
|
|
|
|
| Weight (kg) |
|
|
|
|
At baseline, no significant differences were observed between the groups in terms of stool consistency, constipation severity, frequency of straining, or frequency of retentive fecal incontinence (P > 0.05) (Table II). The frequency of laxative use was also similar between the groups (P > 0.05).
| Control group only received drug treatment. Intervention group additionally received 12 sessions of Swedish abdominal massage. | ||||
| Table II. Analysis of stool variables | ||||
| Variable |
|
|
|
|
| Bristol Stool Scale | ||||
| Before treatment |
|
|||
| Type 1 |
|
|
|
|
| Type 2 |
|
|
|
|
| After treatment |
|
|||
| Type 3 |
|
|
|
|
| Type 4 |
|
|
|
|
| P-value within group |
|
|
||
| Constipation Assessment Scale | ||||
| Before treatment |
|
|
|
|
| After treatment |
|
|
|
|
| P-value within group |
|
|
||
| Straining | ||||
| Before treatment |
|
|
|
|
| After treatment |
|
|
|
|
| P-value within group |
|
|
||
| Painful defecation | ||||
| Before treatment |
|
|
|
|
| After treatment |
|
|
|
|
| P-value within group |
|
|
||
| Retentive fecal incontinence | ||||
| Before treatment |
|
|
|
|
| After treatment |
|
|
|
|
| P-value within group |
|
|
||
| Withholding behavior | ||||
| Before Treatment |
|
|
|
|
| After Treatment |
|
|
|
|
| P-value within group |
|
|
||
Stool consistency
Stool consistency was assessed using BSS. At baseline, stool consistency was predominantly classified as type 1 or type 2, indicative of constipation. After treatment, both groups showed improvement in stool consistency, with a shift towards types 3 (sausage-shaped, with cracks) and 4 (smooth and soft, resembling a sausage). However, there was no significant difference in stool consistency between the two groups (P > 0.05) (Table II).
Constipation severity
Constipation severity was assessed using CAS, where higher scores indicate more severe symptoms. In the control group, there was no significant reduction in constipation severity, with average CAS scores decreasing slightly from 14.54 ± 1.57 to 14.18 ± 1.56 (P = 0.398). Conversely, the intervention group showed a significant decrease in constipation symptoms, with the average CAS score reducing from 14.70 ± 1.29 to 10.21 ± 1.45 (P < 0.001) (Table II).
Straining and painful defecation
The frequency of straining decreased in both groups, from 82.1% to 39.3% in the control group and from 72.7% to 39.3% in the intervention group; however, the difference between groups was not statistically significant (P = 0.601). The frequency of painful defecation decreased significantly in both groups. In the control group, the percentage decreased from 71.4% to 25% (P < 0.001), while in the intervention group, it decreased from 72.7% to 27.3% (P < 0.001). No significant difference in the frequency of painful defecation was found between the two groups (P = 0.538) (Table II).
Retentive fecal incontinence and withholding behavior
The frequency of retentive fecal incontinence decreased significantly in the intervention group, from 3.82 ± 1.33 days per week at baseline to 2.70 ± 1.33 days per week post-treatment (P < 0.001). In the control group, this change was not significant, decreasing from 3.79 ± 1.59 to 3.57 ± 1.20 days per week (P = 0.372). Withholding behavior also decreased in both groups: from 64.3% to 32.1% in the control group (P = 0.016) and from 66.7% to 30.3% in the intervention group (P = 0.003), but there was no significant difference between the groups (P = 0.548) (Table II).
Adverse events
In the intervention group, 5 out of 33 participants (15.2%) reported mild abdominal discomfort during massage sessions, which resolved without intervention. No serious adverse events were reported in either group. In the control group, 2 out of 28 participants (7.1%) experienced mild diarrhea, likely related to laxative use.
Discussion
The findings demonstrated that abdominal massage significantly improved CAS and reduced fecal incontinence compared to pharmacological treatment alone. However, no significant difference was observed in stool consistency between the groups (P > 0.05), indicating that the effect of abdominal massage on stool consistency remains inconclusive based on our results. Therefore, claims regarding improvements in stool consistency should be made cautiously and require further investigation.
The therapeutic efficacy of abdominal massage may be attributed to its potential to enhance gastrointestinal motility and stimulate bowel movements, although the exact physiological mechanisms in children with chronic functional constipation require further research. Previous studies have reported that abdominal massage can improve colonic transit time and reduce constipation symptoms, supporting our findings.15,26
The abdominal massage intervention was well-tolerated, with no serious adverse effects reported. Mild abdominal discomfort observed in a few children was transient and did not necessitate discontinuation of therapy. These results align with prior studies suggesting that abdominal massage is a safe complementary therapy for children with functional constipation. A 2019 systematic review confirmed the effectiveness and safety of several complementary interventions, including massage, without any reported adverse effects.27
Our results are consistent with a randomized controlled trial comparing drug therapy with manual physiotherapy—including abdominal massage—in children with functional constipation, which demonstrated symptom relief and improved stool consistency, although no statistically significant difference between treatment groups was found.28 Moreover, systematic reviews have highlighted abdominal massage as a useful intervention to alleviate constipation severity and associated symptoms such as bloating and pain.28 Participants in our study showed improvement in stool form, transitioning from severe constipation types (1 and 2) to more normal stool types (3 and 4) after treatment, indicating clinical benefit. This is aligned with findings from other pediatric studies, including research on infants with early-onset constipation who experienced symptom relief following abdominal massage.29 However, our study focused on older children with more established behavioral and dietary patterns, suggesting that the benefits of massage extend across a wider pediatric age range.
A randomized controlled trial comparing drug therapy to manual physiotherapy in children with functional constipation found both methods effective in symptom relief and stool consistency improvement, although no statistically significant superiority was observed.30 Although quality of life (QoL) and psychosocial factors were not formally assessed in our study, these are important dimensions to consider in future research. Future research should incorporate validated QoL assessments to examine this potential benefit more rigorously.
Functional constipation is influenced by complex interactions among physiological, psychological, social, and cultural factors. A systematic review and meta-analysis revealed that children with functional constipation report a lower quality of life compared to their healthy peers.31 Previous literature highlights that parental education, psychological health, and caregiving strategies significantly affect constipation management outcomes.32,33 In our study, parents were provided with information about the pathophysiology of constipation and the mechanisms through which massage could help, which likely enhanced their engagement. Although no formal satisfaction assessment was conducted, the observed clinical improvements and regular follow-up sessions may have contributed to maternal satisfaction. Furthermore, a recent systematic review underscored the association between pediatric constipation and exposure to stress, suggesting that life stressors—both at home and in school—can act as contributing factors.34 In our context, it is reasonable to assume that symptom relief positively affected maternal emotional well-being, as improvements in the child’s condition may reduce caregiver stress.
Limitations
Several limitations should be noted. First, the absence of a massage-only group limits the ability to isolate the specific effects of abdominal massage apart from pharmacological treatment. Second, the lack of a sham massage (placebo control) group reduces the ability to distinguish true therapeutic effects from placebo responses. Third, QoL and caregiver satisfaction were not evaluated. Lastly, the relatively small sample size and single-center design may limit generalizability. Larger, multicenter studies with longer follow-up and more comprehensive outcome measures are needed to validate and expand upon these findings.
Conclusion
In conclusion, this study provides evidence that abdominal massage combined with conventional drug therapy is an effective safe complementary intervention for children with chronic functional constipation. The underlying physiological mechanisms—such as parasympathetic stimulation and enhanced gastrointestinal motility—support its therapeutic potential. While further research is needed to address study limitations, our findings support abdominal massage as a safe, cost-effective, and non-invasive complementary strategy. Future investigations should evaluate long-term efficacy, impacts on quality of life, and caregiver-administered protocols to improve adherence and accessibility.
Ethical approval
The study was approved by the Research Council of the Faculty of Medicine at Tehran University of Medical Sciences, and the ethical code (IR.TUMS.MEDICINE.REC.1401.268) was obtained. The study was also registered in the Iranian Registry of Clinical Trials (IRCT20230929059549N1). Informed consent was obtained from the parents or legal guardians, and confidentiality of patient information was maintained throughout the study. The research adhered to the ethical guidelines outlined in the Declaration of Helsinki.
Source of funding
The authors declare the study received no funding.
Conflict of interest
The authors declare that there is no conflict of interest.
References
- Bassotti G, Usai Satta P, Bellini M. Chronic idiopathic constipation in adults: a review on current guidelines and emerging treatment options. Clin Exp Gastroenterol 2021; 14: 413-428. https://doi.org/10.2147/CEG.S256364
- Levy EI, Lemmens R, Vandenplas Y, Devreker T. Functional constipation in children: challenges and solutions. Pediatric Health Med Ther 2017; 8: 19-27. https://doi.org/10.2147/PHMT.S110940
- Rajindrajith S, Devanarayana NM, Weerasooriya L, Hathagoda W, Benninga MA. Quality of life and somatic symptoms in children with constipation: a school-based study. J Pediatr 2013; 163: 1069-72.e1. https://doi.org/10.1016/j.jpeds.2013.05.012
- Bezgin S, Atıcı A, Çelikkaya ME, et al. An investigation of the effects of abdominal massage on the severity of functional constipation in preschool children and the quality of life of their mothers: a randomized controlled study. Journal of Social and Analytical Health 2023; 3: 69-76. https://doi.org/10.5281/zenodo.7642774
- Drossman DA. Functional gastrointestinal disorders: history, pathophysiology, clinical features and Rome IV. Gastroenterology 2016; 150: P1262-P1279. https://doi.org/10.1053/j.gastro.2016.02.032
- Wang C, Shang L, Zhang Y, et al. Impact of functional constipation on health-related quality of life in preschool children and their families in Xi’an, China. PLoS One 2013; 8: e77273. https://doi.org/10.1371/journal.pone.0077273
- Field T. Pediatric massage therapy research: a narrative review. Children (Basel) 2019; 6: 78. https://doi.org/10.3390/children6060078
- Gao L, Jia C, Huang H. Paediatric massage for treatment of acute diarrhoea in children: a meta-analysis. BMC Complement Altern Med 2018; 18: 257. https://doi.org/10.1186/s12906-018-2324-4
- Daniali M, Nikfar S, Abdollahi M. An overview of interventions for constipation in adults. Expert Rev Gastroenterol Hepatol 2020; 14: 721-732. https://doi.org/10.1080/17474124.2020.1781617
- Włodarczyk J, Waśniewska A, Fichna J, Dziki A, Dziki Ł, Włodarczyk M. Current overview on clinical management of chronic constipation. J Clin Med 2021; 10: 1738. https://doi.org/10.3390/jcm10081738
- Kovacic K, Sood MR, Mugie S, et al. A multicenter study on childhood constipation and fecal incontinence: effects on quality of life. J Pediatr 2015; 166: 1482-7.e1. https://doi.org/10.1016/j.jpeds.2015.03.016
- Tabbers MM, DiLorenzo C, Berger MY, et al. Evaluation and treatment of functional constipation in infants and children: evidence-based recommendations from ESPGHAN and NASPGHAN. J Pediatr Gastroenterol Nutr 2014; 58: 258-274. https://doi.org/10.1097/MPG.0000000000000266
- Boonruab J, Poonsuk P, Damjuti W. Effect of court-type Thai traditional massage versus Senokot treatment on chronic constipation: a randomized controlled trial. J Evid Based Integr Med 2020; 25: 2515690X20960644. https://doi.org/10.1177/2515690X20960644
- Doğan İG, Gürşen C, Akbayrak T, et al. Abdominal massage in functional chronic constipation: a randomized placebo-controlled trial. Phys Ther 2022; 102: pzac058. https://doi.org/10.1093/ptj/pzac058
- Silva CA, Motta ME. The use of abdominal muscle training, breathing exercises and abdominal massage to treat paediatric chronic functional constipation. Colorectal Dis 2013; 15: e250-e255. https://doi.org/10.1111/codi.12160
- Gu X, Zhang L, Yuan H, Zhang M. Analysis of the efficacy of abdominal massage on functional constipation: a meta-analysis. Heliyon 2023; 9: e18098. https://doi.org/10.1016/j.heliyon.2023.e18098
- Bromley D. Abdominal massage in the management of chronic constipation for children with disability. Community Pract 2014; 87: 25-29.
- Elbasan B, Bezgin S. The effects of reflexology on constipation and motor functions in children with cerebral palsy. Pediatr Neonatol 2018; 59: 42-47. https://doi.org/10.1016/j.pedneo.2017.01.005
- Rome Foundation. Rome IV criteria. 2016. Available at: https://theromefoundation.org/rome-iv/rome-iv-criteria/
- van Engelenburg-van Lonkhuyzen ML, Bols EM, Benninga MA, Verwijs WA, de Bie RA. Effectiveness of pelvic physiotherapy in children with functional constipation compared with standard medical care. Gastroenterology 2017; 152: 82-91. https://doi.org/10.1053/j.gastro.2016.09.015
- Kemal Ö. Power analysis and sample size, when and why? Turk Arch Otorhinolaryngol 2020; 58: 3-4. https://doi.org/10.5152/tao.2020.0330
- Sinclair M. The use of abdominal massage to treat chronic constipation. J Bodyw Mov Ther 2011; 15: 436-445. https://doi.org/10.1016/j.jbmt.2010.07.007
- Duong NK, Shrestha S, Park D, et al. Bristol stool scale as a determinant of hepatic encephalopathy management in patients with cirrhosis. Am J Gastroenterol 2022; 117: 295-300. https://doi.org/10.14309/ajg.0000000000001550
- Mínguez Pérez M, Benages Martínez A. The Bristol scale - a useful system to assess stool form? Rev Esp Enferm Dig 2009; 101: 305-311.
- Dal Molin A, McMillan SC, Zenerino F, et al. Validity and reliability of the Italian Constipation Assessment Scale. Int J Palliat Nurs 2012; 18: 321-325. https://doi.org/10.12968/ijpn.2012.18.7.321
- Canbulat Sahiner N, Demirgoz Bal M. A Randomized controlled trial examining the effects of reflexology on children with functional constipation. Gastroenterol Nurs 2017; 40: 393-400. https://doi.org/10.1097/SGA.0000000000000196
- Paknejad MS, Motaharifard MS, Barimani S, Kabiri P, Karimi M. Traditional, complementary and alternative medicine in children constipation: a systematic review. Daru 2019; 27: 811-826. https://doi.org/10.1007/s40199-019-00297-w
- Dehghan M, Malakoutikhah A, Ghaedi Heidari F, Zakeri MA. The effect of abdominal massage on gastrointestinal functions: a systematic review. Complement Ther Med 2020; 54: 102553. https://doi.org/10.1016/j.ctim.2020.102553
- Ririn YA, Israyati N. The effect of massage therapy in overcoming constipation in infants aged 7-12 months. Science Midwifery 2021; 9: 228-231.
- Blanco Díaz M, Bousoño García C, Segura Ramírez DK, Rodríguez Rodriguez ÁM. Manual physical therapy in the treatment of functional constipation in children: a pilot randomized controlled trial. J Altern Complement Med 2020; 26: 620-627. https://doi.org/10.1089/acm.2020.0047
- Vriesman MH, Rajindrajith S, Koppen IJN, et al. Quality of life in children with functional constipation: a systematic review and meta-analysis. J Pediatr 2019; 214: 141-150. https://doi.org/10.1016/j.jpeds.2019.06.059
- van Dijk M, de Vries GJ, Last BF, Benninga MA, Grootenhuis MA. Parental child-rearing attitudes are associated with functional constipation in childhood. Arch Dis Child 2015; 100: 329-333. https://doi.org/10.1136/archdischild-2014-305941
- Çağan Appak Y, Yalın Sapmaz Ş, Doğan G, Herdem A, Özyurt BC, Kasırga E. Clinical findings, child and mother psychosocial status in functional constipation. Turk J Gastroenterol 2017; 28: 465-470. https://doi.org/10.5152/tjg.2017.17216
- Liyanarachchi H, Rajindrajith S, Kuruppu C, et al. Association between childhood constipation and exposure to stressful life events: a systematic review. Neurogastroenterol Motil 2022; 34: e14231. https://doi.org/10.1111/nmo.14231
Copyright and license
Copyright © 2025 The Author(s). This is an open access article distributed under the Creative Commons Attribution License (CC BY), which permits unrestricted use, distribution, and reproduction in any medium or format, provided the original work is properly cited.