Graphical Abstract
Abstract
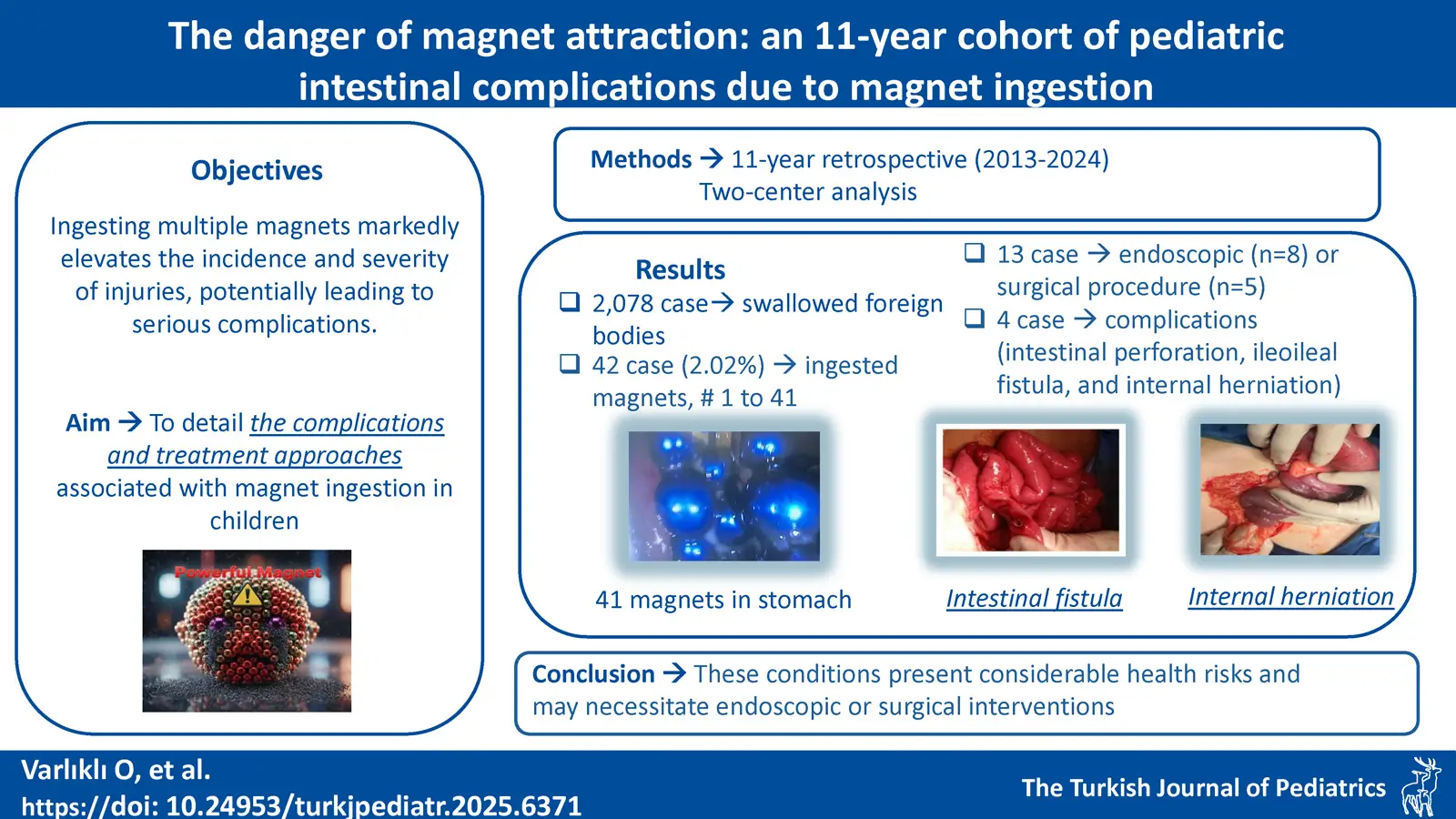
Introduction. In recent years, there has been a significant rise in the number of pediatric cases involving multiple magnet ingestion, resulting in increased incidence and morbidity of injuries. When a metal object and magnet are ingested, either single or multiple, they can cause serious complications such as intestinal obstruction, ischemia, necrosis, fistula, perforation, and even death. This study aims to detail the complications and treatment approaches associated with magnet ingestion in children.
Materials and Methods. In our study, we conducted a retrospective analysis of all cases involving the ingestion of a magnet along with a second metal object at two training and research hospitals in our province, which admit pediatric patients, between the years of 2013 and 2023.
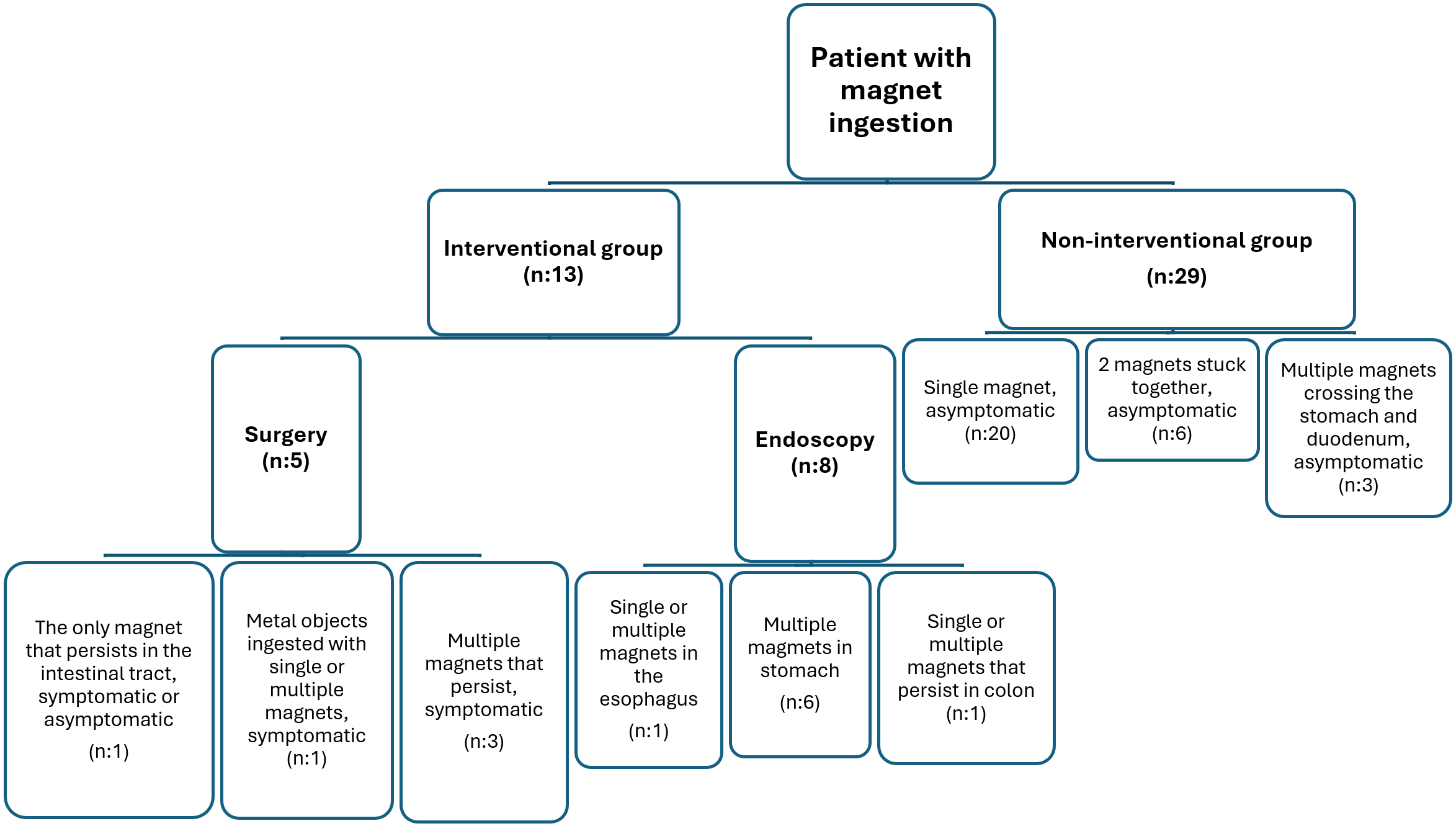
Results. A total of 42 patients had a history of magnet ingestion, with the number of ingested magnets ranging from 1 to 41. The median magnet size was 11 mm (range: 5.5-17.5 mm) and the median time to presentation was 24 hours (range: 3-48 hours). Thirteen patients (30.9%) required either endoscopic or surgical intervention to extract the magnets or address complications. Endoscopy was performed on eight patients, while surgical intervention was required for five patients. Among those who underwent surgery, four experienced complications, including intestinal perforation, ileoileal fistula, and internal herniation. Notably, no fatalities occurred following intervention. There was no statistically significant difference in age or magnet size between the interventional and non-interventional groups. However, the length of hospital stay was significantly longer in the interventional group compared to the non-interventional group (P<0.05).
Conclusions. The ingestion of magnets by children can result in serious complications, such as intestinal fistula, perforation, and volvulus. These conditions pose significant health risks and may require endoscopic or surgical intervention.
Keywords: magnet, foreign body, children, endoscopy, surgery
Introduction
Foreign body ingestion poses a significant health concern due to its prevalence, particularly among pediatric patients. Annually, approximately 100,000 incidents of foreign body ingestion are documented in the United States, with 80% of these cases involving children aged between 6 months to 3 years.1-3 While many cases of foreign body ingestion result in uncomplicated transit through the gastrointestinal tract, the ingestion of button batteries and multiple magnets has been associated with complications, including potentially life-threatening conditions.4,5 In fact, fatalities have been reported following the ingestion of multiple magnets.6 The tendency of toddlers to explore their environment orally leads to with increased instances of ingestion, while adolescents often ingest foreign bodies as a result of improper tongue and lip piercings. Less than 1% of foreign bodies in the stomach require surgery or cause complications, whereas 10–20% require endoscopic intervention.7,8
The notable rise in pediatric injuries related to magnets over the past two decades is a significant concern.4,9-12 This increase coincides with the growing sales of small, potent neodymium-iron-boron magnets, which are frequently sold as part of toy sets. This study aims to increase awareness of the potentially life-threatening consequences associated with the ingestion of multiple magnets by children, which may include obstruction, fistula formation, and perforation. This article serves as a reminder of the dangers associated with magnet ingestion and aims to highlight this issue.
Materials and Methods
This study was a retrospective, two-center analysis. The study was approved by the Kocaeli University Faculty of Medicine Clinical Research Ethics Committee (reference number GOKAEK-2024/01.13). A comprehensive collection and analysis of all cases of magnet ingestion admitted to Kocaeli University Hospital and Kocaeli City Hospital from January 2013 to December 2023 was conducted. The collected data encompassed demographic information, including age and sex, as well as medical history, symptoms, physical examination findings, diagnostic methods, treatments, post-treatment follow-up, and details regarding the ingestion of magnets, such as their quantity, size, localization, and the endoscopic and surgical interventions performed. Morbidity was defined as any injury directly attributable to magnets, encompassing perforation, fistula formation, obstruction, bleeding, infection, volvulus, and/or intestinal herniation. Patients who ingested magnets were categorized as follows: those who passed them spontaneously through the gastrointestinal tract were classified as mild; those requiring intervention were classified as moderate; and those presenting with complications were classified as severe. Patients were categorized into groups based on the ingestion of a single magnet or multiple magnets. Because patients who ingested multiple magnets exhibited similar clinical behavior to those who ingested a magnet alongside a metallic object, the latter were included in the multiple magnet ingestion group. Furthermore, distinct groups were established for patients who required medical intervention and those who did not. Statistical analysis was conducted using the chi-squared test to compare these groups. Categorical variables are presented as frequencies (percentages), whereas numerical variables are reported as the median with the interquartile range (25th-75th percentile, Q1-Q3). Statistical significance was determined by a p-value of less than 0.05, consistent with established statistical conventions.
Results
During the period spanning 2013 to 2023, the total number of emergency department visits for pediatric patients was 1,110,812. Of these, 2,078 patients (0.18%) had swallowed foreign bodies, and 42 patients (2.02%) had ingested magnets. The study sample comprised 42.8% male and 57.1% female patients, with 47.6% of the participants being under the age of four years. Statistical analysis revealed no significant difference between the groups concerning sex (P>0.05).
The median age, sex, magnet size and number, localization, duration of presentation, duration of hospital stay, and comparisons between patients who underwent intervention and those who did not, as well as between those who ingested a single magnet and those who ingested multiple magnets, are presented in Table I. The study revealed that severe consequences resulted in 9.5% of the cases. The outcomes for the 13 patients who underwent the intervention are outlined in Table II.
| GI: gastrointestinal | |||||||
| Table I. Comparison of patients undergoing and not undergoing intervention, and single and multiple magnet ingestion groups | |||||||
|
|
|
|
|
|
|
|
|
| Number, n (%) |
|
|
|
|
|
||
| Sex (M/F), n |
|
|
|
|
|
|
|
| Age, yr, median (Q1-Q3) |
|
|
|
|
|
|
|
|
Time to application, hr, median (Q1-Q3) |
|
|
|
|
|
|
|
| Magnet size, mm, median (Q1-Q3) |
|
|
|
|
|
|
|
| Number of magnets, median (Q1-Q3) |
|
|
|
|
|
|
|
| Hospitalization period, hours, median (Q1-Q3) |
|
|
|
|
|
|
|
| Location, n (%) | |||||||
| Upper GI tract |
|
|
|
|
|
||
| Esophagus |
|
|
|
|
|
||
| Stomach / duodenum |
|
|
|
|
|
||
| Lower GI tract |
|
|
|
|
|
||
| Ileum |
|
|
|
|
|
||
| Cecum |
|
|
|
|
|
||
| Colon |
|
|
|
|
|
||
| * 1 magnet + 28 staple wires | |||||||||
| Table II. Characteristics of patients undergoing intervention. | |||||||||
| Patient no. | Age | Sex | Number of magnets | Magnet size, mm | Ingestion time, hour | Location | Symptom | Damage | Intervention |
| 1 | 12 mo | M | 7 | 5.5 | 96 | Duodenum and colon | Abdominal pain and diarrhea | Perforation and fistula | Primary repair + appendectomy |
| 2 | 24 mo | F | 27 | 5.5 | 48 | Stomach and jejunum | Abdominal pain | Perforation, fistula and peritonitis | Resection anastomosis |
| 3 | 16 mo | F | 1 | 3.6 | 336 | Colon | - | - | Appendectomy |
| 4 | 3 yr | M | 2 | 30 | 120 | Ileum | Abdominal pain and fever | Perforation and fistula | Resection anastomosis |
| 5 | 10 yr | M | 1* | 5.5 | 240 | Ileum | Abdominal pain and fever | Perforation, fistula and internal herniation | Resection anastomosis |
| 6 | 4 yr | F | 1 | 19.5 | 1 | Esophagus | - | - | Endoscopy |
| 7 | 20 mo | M | 2 | 7 | 96 | Stomach and jejunum | - | - | Endoscopy |
| 8 | 18 mo | F | 41 | 5.5 | 48 | Stomach and jejunum | Abdominal pain | - | Endoscopy |
| 9 | 5 yr | F | 2 | 8.5 | 72 | Cecum | - | - | Colonoscopy |
| 10 | 12 mo | F | 2 | 12 | 4 | Stomach | - | Endoscopy | |
| 11 | 5 yr | F | 2 | 5.5 | 2 | Stomach | - | - | Endoscopy |
| 12 | 3 yr | F | 2 | 5.5 | 3 | Stomach | - | - | Endoscopy |
| 13 | 13 mo | F | 3 | 5.5 | 2 | Stomach | - | - | Endoscopy |
Among the children who ingested magnets, 22 (52.3%) ingested a solitary magnet, while 20 (47.7%) ingested multiple magnets. The number of magnets swallowed ranged from 1 to 41.
Median magnet size was 11 mm (Q1-Q3: 5.5-17.5 mm). A statistically significant difference was observed between the single and multiple magnet groups, as well as between the interventional group and that did not (P < 0.05). Median hospital stay was 24 hours (Q1-Q3: 3-48 hr). A statistically significant difference was identified between the single- and multiple-magnet groups, as well as between the intervention and non-intervention groups (P < 0.05) (Table I).
Most patients were asymptomatic (88.2%), while one patient experienced diarrhea (2.3%), and four patients had abdominal pain, restlessness, and fever (9.5%). The ingestion of magnets in asymptomatic patients was confirmed through the patient’s statement, family observation, and incidental plain radiography. Indications for intervention and medical follow-up in the interventional and non- interventional groups are given in Fig. 1.
Among the patients who underwent endoscopic procedures, seven received esophagogastric interventions, while one underwent a colonoscopy. In one case, a single magnet located in the initial esophageal stricture was extracted via esophagoscopy. In six patients, magnets ranging from 1 to 41 were identified in the stomach, all of which were successfully removed through esophagogastroscopy (Fig. 2A). In one patient, a magnet was located in the stomach, with another found in the jejunum, adhering to the stomach magnet (Fig. 2B). The portion of the magnet attached to the jejunum, which was removed from the stomach by gastroscopy, passed through the digestive tract spontaneously the following day.
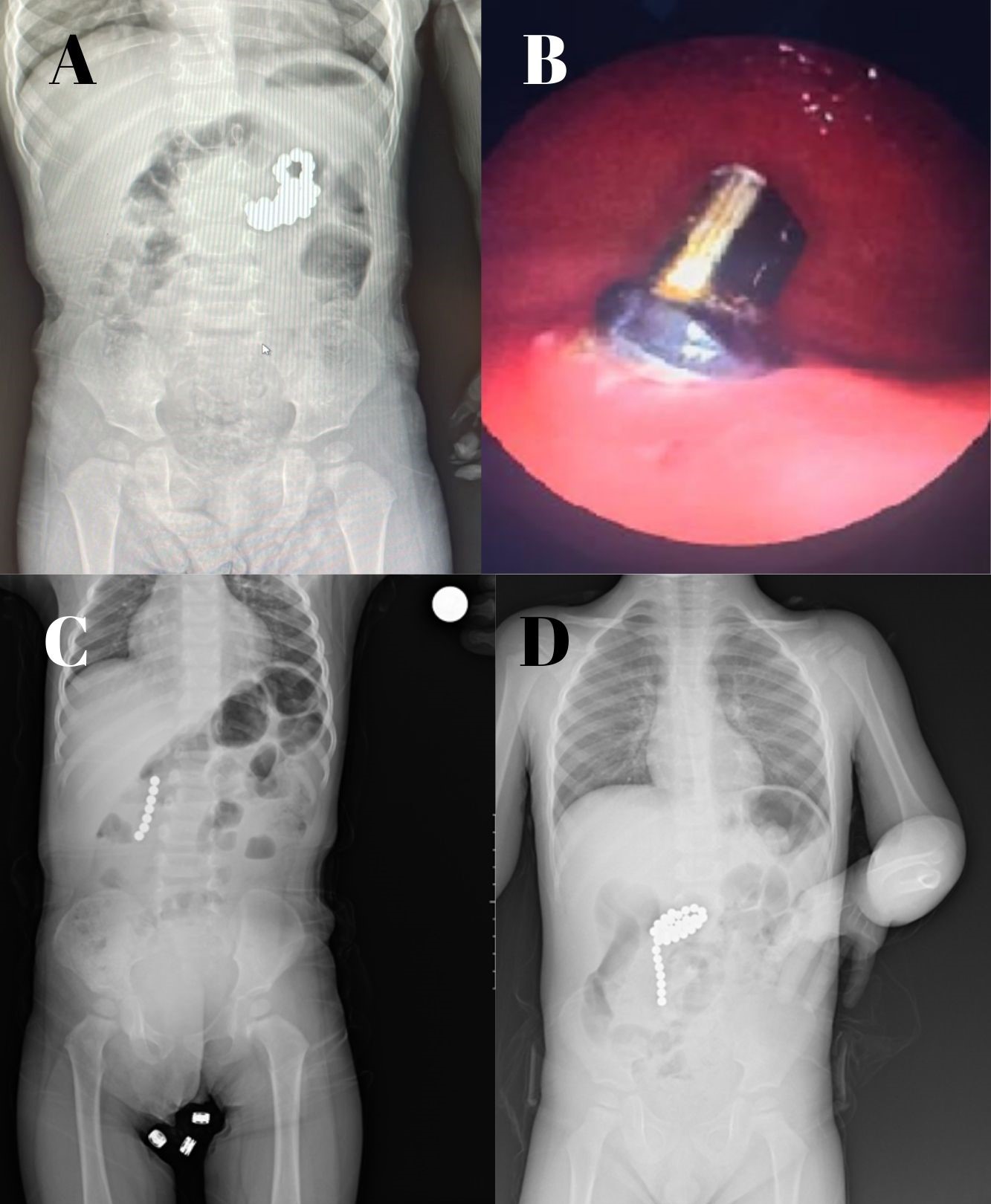
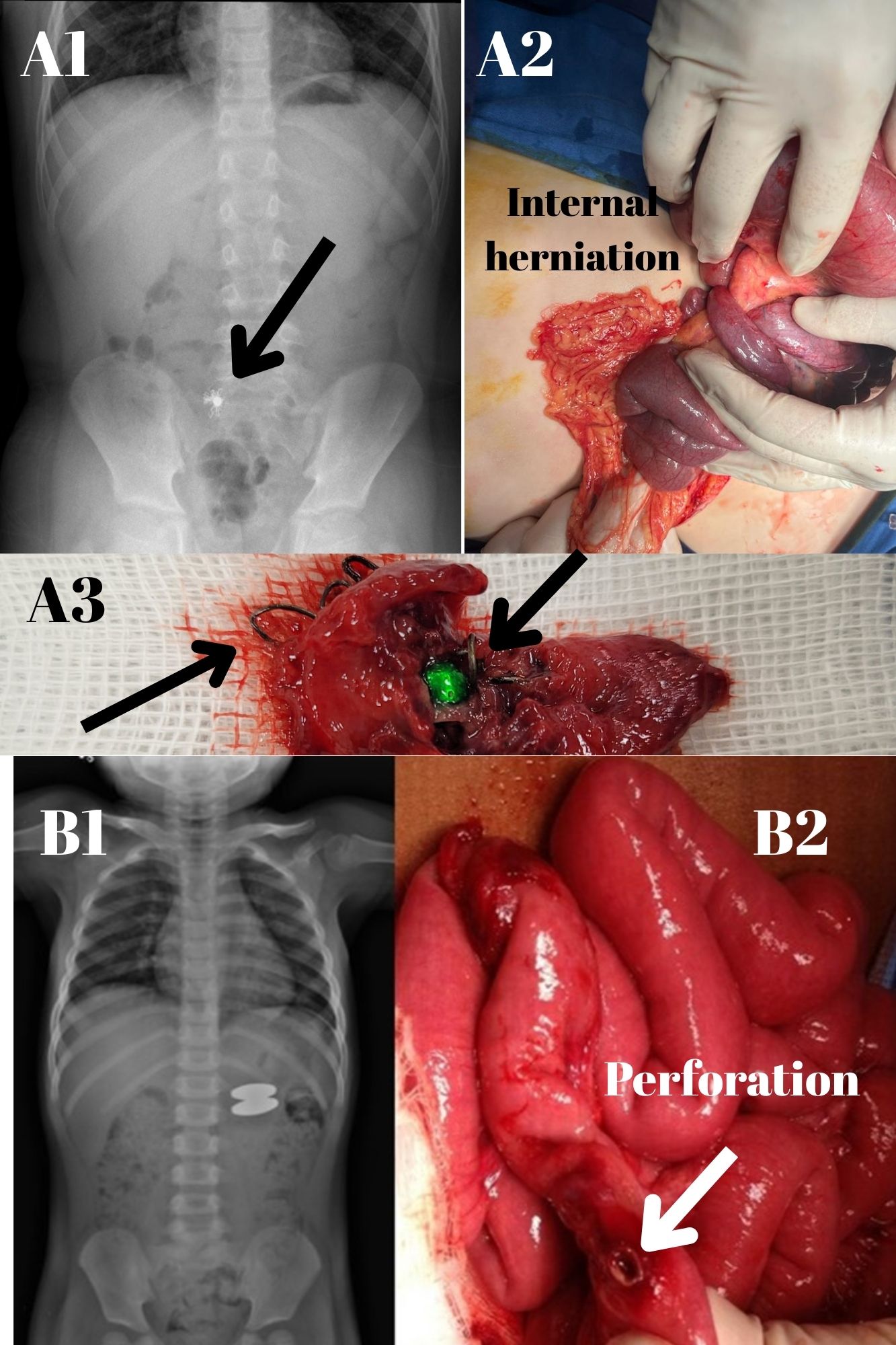
Five patients required surgery. Each patient underwent laparotomy; with the exception of one patient whose surgery was incidental. The indications for surgery included peritoneal signs, intestinal perforation, or intestinal obstruction. A 12-month-old male patient who ingested seven magnets presented with two perforations in her duodenum (Fig. 2C). A two-year-old female patient who ingested twenty-seven magnets presented with two perforations in the stomach and jejunum, which were surgically repaired using primary closure (Fig. 2D). A ten-year-old male patient who ingested 28 staples after swallowing a magnet developed an ileoileal fistula and internal herniation (Fig. 3A1-A3). A three-year-old male patient who ingested two magnets presented with an ileoileal fistula and a perforation (Fig. 3B1-B2). Primary repair was performed in three patients and resection in one patient. In one patient, a magnet found incidentally in the cecum was removed from the appendix and an appendectomy was performed. There were no postoperative or postprocedural complications, and all patients were discharged after recovery. No deaths occurred during the study period.
Discussion
The ingestion of foreign bodies represents a significant concern across all age groups, with evidence indicating that 75% of such cases involve patients under the age of four.13,14 In our study, we observed that only 20 (47.6%) patients were under the age of 4 years, and therefore, pediatric patients of any age should be considered in the differential diagnosis.
Rare earth metals, such as neodymium-iron-boron, are extensively employed in industry due to their exceptional power-to-size ratio, rendering them ideal for use in high-power magnets. These magnets exhibit a confining force that is 5-30 times stronger than that of conventional magnets.4,15,16 Specifically, the magnetic attraction force between 5 mm balls is approximately half a kilogram. This strong magnetic attraction between the intestines results in compression at pressure points, which cuts off blood flow and causes rapid damage to the wall of the intestine. This damage can cause ischemia, necrosis, and perforation.
Since the groundbreaking report by McCormick et al on magnet ingestion, there has been a proliferation of published material detailing the clinical manifestations, complications, and management of this phenomenon.4,11,12,17 In a single-center study conducted in China, the first instance of magnet ingestion was registered in 2015. By 2019, magnets accounted for a staggering 80% of all young children’s foreign body ingestion cases, and an astonishing 76.8% of these cases required surgical intervention.18 The literature is replete with evidence suggesting that the ingestion of multiple magnets significantly heightens the likelihood of hospitalization and surgical intervention, as well as the risk of developing complications.14,16,19 There have been reports of a high incidence of magnet ingestion in older children who use magnets to mimic facial piercings such as those in the lips, tongue, and nostrils.9 One such adolescent patient ingested two magnets while attempting to pierce his lip.
In the initial stages of magnet ingestion, children typically exhibit no symptoms. While the majority of children who ingested a single magnet remained asymptomatic, those who ingested multiple magnets exhibited symptoms of gastrointestinal distress, including fever, vomiting, diarrhea, and abdominal pain. Nausea/vomiting and abdominal pain are the most common non-specific symptoms, with their intensity and duration influenced by the quantity, strength, and location of the ingested magnets, as well as the time elapsed between ingestion and symptom manifestation.20 Following the confirmation of magnet ingestion through radiographic examination, the subsequent step involved assessing whether a single magnet, multiple magnets, or other metallic objects had been ingested. The expulsion of a foreign body, such as a coin or a small round object, can occur naturally and can be managed as an outpatient with daily X-ray examinations. In our study, laxatives were employed as a conservative treatment for 69% of the patients, and this method generally proved to be effective in most cases.
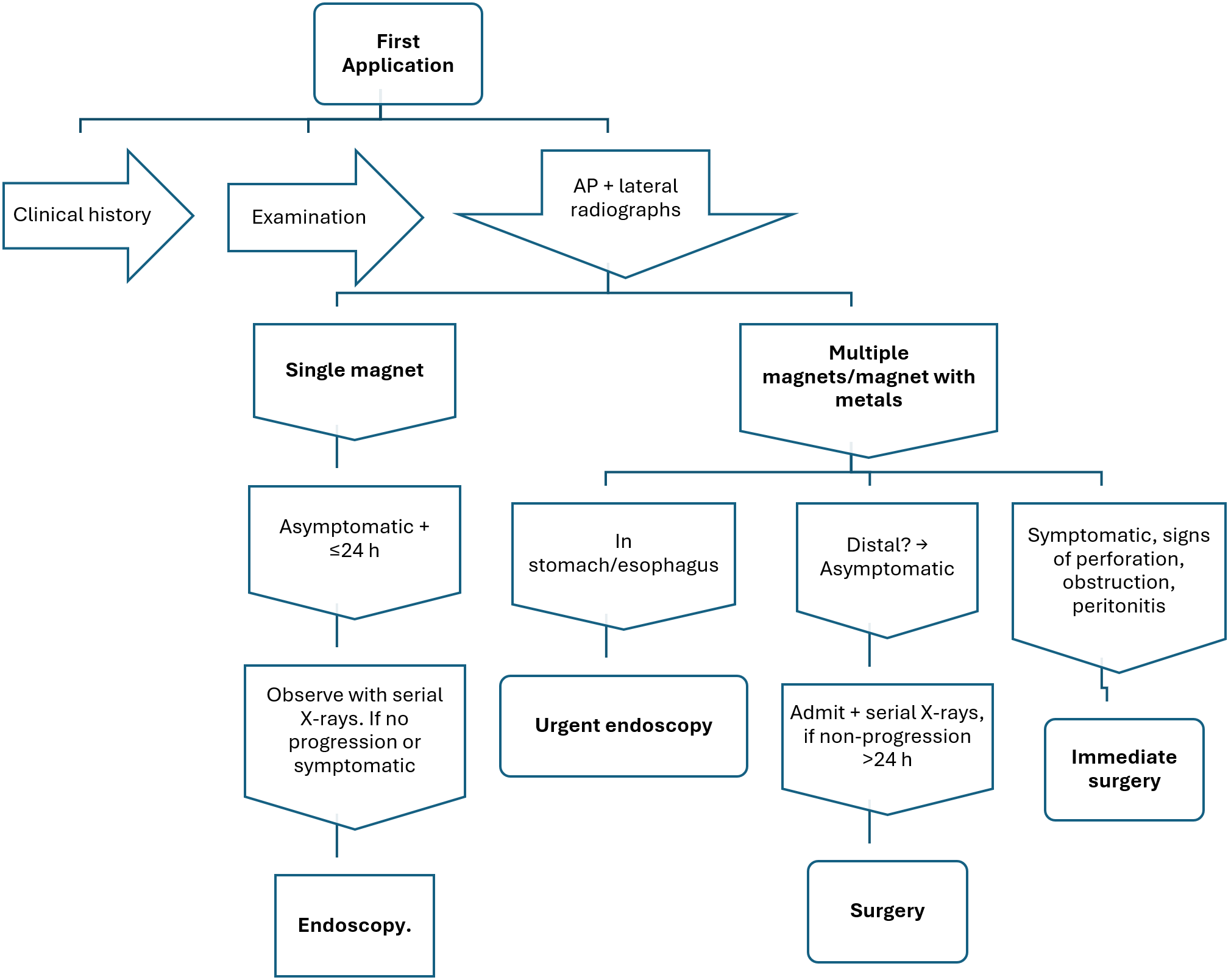
The likelihood of sustaining significant gastrointestinal injuries, such as perforation and obstruction, increases with the ingestion of an increased number of magnets. In instances where multiple magnets or a single magnet is ingested with additional metallic objects, it is advisable to conduct serial radiographic examinations at 4 to 6 hour intervals. In this study, all patients underwent plain radiographs (anteroposterior and lateral views) of the neck, chest, and abdomen, as plain X-rays have a high diagnostic yield. Computerized tomography scans were performed in more complex cases to detect inflammation and small perforations. If it is not possible to distinguish between single and multiple magnet ingestions with certainty, inpatient treatment following the multiple-magnet regimen should be initiated. When there are several magnets, one magnet, or a secondary metallic foreign body in the stomach, endoscopic intervention is necessary. Multiple magnets or a single magnet with a secondary metallic foreign body in the stomach should be surgically removed, especially if there are symptoms or obstructive findings visible on abdominal radiographs. Nonsurgical inpatient therapy, including a bowel regimen and serial radiographic surveillance, is recommended for asymptomatic patients with several magnets or one magnet plus another metallic foreign body in the stomach. Endoscopic or surgical intervention may be considered if there is no progression of the magnet after 48 hours. Modifications to the algorithm proposed by Sola et al. in 2018 were made by Mostafa et al. in 2021.11,21
It is imperative to acknowledge that the ingestion of metal objects, aside from a solitary magnet, can pose substantial risks comparable to those associated with the ingestion of multiple magnets. One of our cases involved a patient who ingested 28 staples along with a magnet, resulting in a fistula and perforation in the intestines, a scenario similar to the ingestion of multiple magnets (Fig. 3A1-A3). The management of magnet ingestion in pediatric patients should be tailored to the specific characteristics of the magnet, the duration since ingestion, and the patient’s clinical condition. Prompt endoscopic or surgical intervention can prevent severe complications. The diagnostic clues and treatment algorithms for clinicians dealing with pediatric patients are presented in Fig. 4.
Patients who ingest multiple magnets should be closely monitored in a controlled clinical setting due to their potential for complications, even if they do not exhibit clinical symptoms. Magnets with smaller diameters pose a greater risk of complications and should be approached with caution. When more than one magnet is ingested, complications can arise in 11-50% of cases, including intestinal perforation, which may require surgical intervention.22,23 Of the 13 patients who underwent surgery in our series, 30.7% had bowel perforation at baseline, and the most common site of perforation was the small intestine.19 In our study, the intervention rate in the multiple magnet group also showed a significant difference (P<0.05). Our hospital admission rate was 36.1%, aligning with the reported range of 27-68%.24,25 Notably, in our study, the duration of hospitalization for patients who ingested multiple magnets showed a statistically significant difference between those who required intervention and those who did not (P<0.05).
If magnet fragments are in the esophagus, stomach, duodenum, or colon, prompt removal by endoscopy within the first 24 hours is crucial. Delaying medical intervention allows magnetic beads to travel from the stomach and eventually reach the intestine, thereby increasing the risk of complications. The success rate of endoscopic removal of magnets is reported to be between 66% and 89% in most cases.11,21 In our series, 62.5% of the patients who underwent endoscopy has magnets successfully removed within the first 24 hours, while the others were removed after 24 hours.20,26 The efficacy of endoscopic removal is significantly influenced by the positioning of the magnets, the duration before the endoscopic procedure, and the expertise of the medical professionals involved. Magnets that have penetrated the mucosa are particularly difficult to remove. It is important to note that magnets may adhere to the device or be displaced during the endoscopy process. In one of our cases, we were unable to detect the magnets in the cecum during colonoscopy, but we were able to locate them after they had adhered to the device and were identified after removing it from the rectum. In instances where endoscopic removal is unfeasible or complications arise during the procedure, surgical intervention may become necessary. Depending on the available resources and the expertise of the medical team, surgical removal can be performed using either laparotomy or laparoscopy. Nonetheless, the laparoscopic extraction of magnets presents challenges due to their tendency to adhere to surgical instruments.
Due to the significant health hazards associated with strong magnets, it is imperative to prevent young children from ingesting these objects. The small and shiny nature of magnets can attract the curiosity of children. In order to reduce these risks, parents and caregivers must make sure that magnetic toys adhere to strict safety regulations and keep all magnets, especially those made of rare earth elements like neodymium, in places that are out of children’s reach. Public awareness initiatives, child-resistant packaging, and clear warning labels on products that contain magnets are essential. Ultimately, prevention can be achieved through responsible product design and vigilant adult supervision.
One possible limitation of this study is that the data were collected retrospectively, which inherently carries the risk of bias or missing information. Data may not have been fully transferred due to changes in the hospital database system. Thus, we may have missed cases of ingested foreign bodies and not reached the true incidence rates. However, we would like to highlight the strengths of our study. This study presents comprehensive information about why magnetic attraction continues to be a danger to children and how it poses risks. In addition, it offers physicians a detailed algorithm for both diagnosis and treatment.
Conclusions
The incidence of severe injuries resulting from magnet ingestion in children is on the rise. In instances where a child presents to the pediatric emergency department with suspected magnet ingestion, it is crucial to achieve a prompt and accurate diagnosis to prevent serious complications. Early detection is essential, as delays may lead to severe outcomes, including gastrointestinal perforation, volvulus, and fistula formation, particularly when multiple magnets are involved. These high-risk scenarios can often be mitigated through timely imaging and intervention. Therefore, it is imperative that magnet ingestion is neither overlooked nor misdiagnosed, as early recognition is vital for preventing life-threatening sequelae and ensuring optimal patient outcomes.
Ethical approval
The study was approved by Kocaeli University Faculty of Medicine (date: January 18, 2024, number: GOKAEK-2024/01.13).
Source of funding
The authors declare the study received no funding.
Conflict of interest
The authors declare that there is no conflict of interest.
References
- Gummin DD, Mowry JB, Spyker DA, et al. 2018 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 36th Annual Report. Clin Toxicol (Phila) 2019; 57: 1220-1413. https://doi.org/10.1080/15563650.2019.1677022
- Brown DJ. Small bowel perforation caused by multiple magnet ingestion. J Emerg Med 2010; 39: 497-498. https://doi.org/10.1016/j.jemermed.2008.04.007
- Kramer RE, Lerner DG, Lin T, et al. Management of ingested foreign bodies in children: a clinical report of the NASPGHAN Endoscopy Committee. J Pediatr Gastroenterol Nutr 2015; 60: 562-574. https://doi.org/10.1097/MPG.0000000000000729
- Seguier-Lipszyc E, Samuk I, Almog A, Silbermintz A, Kravarusic D. Multiple magnet ingestion in children: a problem on the rise. J Paediatr Child Health 2022; 58: 1824-1828. https://doi.org/10.1111/jpc.16117
- Labadie M, Vaucel JA, Courtois A, et al. Button battery ingestion in children (PilBouTox®): a prospective study describing the clinical course and identifying factors related to esophageal impaction or severe cases. Dysphagia 2023; 38: 446-456. https://doi.org/10.1007/s00455-022-10485-7
- Olczak M, Skrzypek E. A case of child death caused by intestinal volvulus following magnetic toy ingestion. Leg Med (Tokyo) 2015; 17: 184-187. https://doi.org/10.1016/j.legalmed.2014.11.007
- Thomson M, Tringali A, Dumonceau JM, et al. Paediatric gastrointestinal endoscopy: European Society for Paediatric Gastroenterology Hepatology and Nutrition and European Society of Gastrointestinal Endoscopy Guidelines. J Pediatr Gastroenterol Nutr 2017; 64: 133-153. https://doi.org/10.1097/MPG.0000000000001408
- Gezer HÖ, Ezer SS, Temiz A, İnce E, Hiçsönmez A. Ingested foreign bodies in children: do they really pass spontaneously from the gastrointestinal tract? A single-centre experience with 1000 cases. Ulus Travma Acil Cerrahi Derg 2020; 26: 247-254. https://doi.org/10.14744/tjtes.2019.40350
- Agbo C, Lee L, Chiang V, et al. Magnet-related injury rates in children: a single hospital experience. J Pediatr Gastroenterol Nutr 2013; 57: 14-17. https://doi.org/10.1097/mpg.0b013e318292fa2e
- Naji H, Isacson D, Svensson JF, Wester T. Bowel injuries caused by ingestion of multiple magnets in children: a growing hazard. Pediatr Surg Int 2012; 28: 367-374. https://doi.org/10.1007/s00383-011-3026-x
- Mostafa MS, Darwish AA. Magnet ingestion in children and its implications: tertiary centre experience. Pediatr Surg Int 2021; 37: 937-944. https://doi.org/10.1007/s00383-021-04889-z
- Middelberg LK, Leonard JC, Shi J, et al. High-powered magnet exposures in children: a multi-center cohort study. Pediatrics 2022; 149: e2021054543. https://doi.org/10.1542/peds.2021-054543
- Huang X, Hu J, Xia Z, Lin X. Multiple magnetic foreign body ingestion in pediatric patients: a single-center retrospective review. Pediatr Surg Int 2021; 37: 639-643. https://doi.org/10.1007/s00383-020-04814-w
- Chang A, Yeap E, Lee E, et al. Decade of the dangers of multiple magnet ingestion in children: a retrospective review. J Paediatr Child Health 2022; 58: 873-879. https://doi.org/10.1111/jpc.15863
- Shaul E, Agawu A, Wood P, Umhoefer K, Mamula P. Management of magnet ingestions at a large tertiary care children’s hospital. J Pediatr Gastroenterol Nutr 2022; 75: 334-339. https://doi.org/10.1097/MPG.0000000000003502
- Nugud AA, Tzivinikos C, Assa A, et al. Pediatric magnet ingestion, diagnosis, management, and prevention: a European Society for Paediatric Gastroenterology Hepatology and Nutrition (ESPGHAN) position paper. J Pediatr Gastroenterol Nutr 2023; 76: 523-532. https://doi.org/10.1097/MPG.0000000000003702
- McCormick S, Brennan P, Yassa J, Shawis R. Children and mini-magnets: an almost fatal attraction. Emerg Med J 2002; 19: 71-73. https://doi.org/10.1136/emj.19.1.71
- Cai DT, Shu Q, Zhang SH, Liu J, Gao ZG. Surgical treatment of multiple magnet ingestion in children: a single-center study. World J Clin Cases 2020; 8: 5988-5998. https://doi.org/10.12998/wjcc.v8.i23.5988
- Alansari AN, Baykuziyev T, Soyer T, et al. Magnet ingestion in growing children: a multi-center observational study on single and multiple magnet incidents. Sci Rep 2024; 14: 4575. https://doi.org/10.1038/s41598-024-55127-0
- Han Y, Youn JK, Oh C, Lee S, Seo JM, Kim HY. Ingestion of multiple magnets in children. J Pediatr Surg 2020; 55: 2201-2205. https://doi.org/10.1016/j.jpedsurg.2019.11.021
- Sola R, Rosenfeld EH, Yu YR, St Peter SD, Shah SR. Magnet foreign body ingestion: rare occurrence but big consequences. J Pediatr Surg 2018; 53: 1815-1819. https://doi.org/10.1016/j.jpedsurg.2017.08.013
- Miyamoto R, Okuda M, Kikuchi S, Iwayama H, Hataya H, Okumura A. A nationwide questionnaire survey on accidental magnet ingestion in children in Japan. Acta Paediatr 2021; 110: 314-325. https://doi.org/10.1111/apa.15428
- Abbas MI, Oliva-Hemker M, Choi J, et al. Magnet ingestions in children presenting to US emergency departments, 2002-2011. J Pediatr Gastroenterol Nutr 2013; 57: 18-22. https://doi.org/10.1097/MPG.0b013e3182952ee5
- Hernández Anselmi E, Gutiérrez San Román C, Barrios Fontoba JE, et al. Intestinal perforation caused by magnetic toys. J Pediatr Surg 2007; 42: E13-E16. https://doi.org/10.1016/j.jpedsurg.2006.12.066
- Waters AM, Teitelbaum DH, Thorne V, Bousvaros A, Noel RA, Beierle EA. Surgical management and morbidity of pediatric magnet ingestions. J Surg Res 2015; 199: 137-140. https://doi.org/10.1016/j.jss.2015.04.007
- Chavan R, Bachkaniwala V, Tadkalkar V, Gandhi C, Rajput S. Endoscopic management of magnet ingestion and its adverse events in children. VideoGIE 2022; 7: 302-307. https://doi.org/10.1016/j.vgie.2022.03.008
Copyright and license
Copyright © 2025 The Author(s). This is an open access article distributed under the Creative Commons Attribution License (CC BY), which permits unrestricted use, distribution, and reproduction in any medium or format, provided the original work is properly cited.