Abstract
Background. The global spread of coronavirus disease 2019 (COVID-19) and associated policies have caused negative consequences at the level of children, families, and services, resulting in physical, mental, and developmental issues in children, as well as limited access to healthcare. We evaluated the referral numbers, sources, and trends of a developmental-behavioral pediatrics (DBP) department in Türkiye as a Eurasian country, as well as the effects of the COVID-19 pandemic on referral variables.
Methods. This retrospective cohort study examined patient referral data to the Division of Developmental Behavioral Pediatrics, Department of Pediatrics, Hacettepe University between the years 2014 and 2021. We analyzed the changes in the number of referrals over time in 3-month intervals using polynomial regression models. The impact of the COVID-19 pandemic on referral reasons was evaluated.
Results. Polynomial regression analyses demonstrated significant nonlinear trends in consultation volumes across all categories. During the pre-pandemic period, referrals showed a marked increase, reaching a peak around 2018 before declining. In the post-pandemic period, an initial surge in consultations was followed by a notable decline after 2021. Notably, referral numbers had dropped to their lowest levels during the pandemic. Similarly, referrals to neonatal and pediatric clinics increased sharply until 2020, after which a plateau or slight decrease was observed, indicating a deceleration in growth over time. Referrals for perinatal-neonatal risks were 1.359 (95% confidence interval: 1.269-1.456) times higher than in the pre-pandemic period, and those for suspected autism were 1.209 (95% confidence interval: 0.987-1.478) times higher.
Conclusions. Although it is encouraging that our referral trends have improved in the 1.5 years since the COVID-19 pandemic, it is thought that health service constraints caused a considerable increase in prenatal risk and suspicion of autism referrals following the pandemic. Improvement and innovation in healthcare systems to prevent the long-term detrimental impacts of periodic interruptions in healthcare on children’s development and behavior is needed.
Keywords: coronavirus disease 2019, referral trends, developmental and behavioral pediatrics, pandemic
Introduction
Early childhood is a sensitive developmental period, and it’s known that all interventions that will reduce developmental risks and increase resilience in this period have positive effects on health, academic skills, and economic productivity in adulthood.1 Currently, the effectiveness of family-centered strategies during developmental follow-ups is known and primary healthcare providers have a key role in this regard. Primary care providers frequently do have not the competence to promote early childhood development due to the deficiency of educational curricula.2,3 However, in a study conducted in Türkiye, most parents stated that developmental issues were more frequently addressed in primary healthcare services.4 Time constraints, inadequate reimbursements, staffing shortages, and a lack of knowledge concerning referral alternatives for positive screening results are the most critical problems that pediatricians experience when completing developmental screening and building a referral chain for early intervention.5,6 All of these situations demonstrate the need for regulations in health systems, and it is emphasized that cooperation between all sectors, not just health and education, is required to improve early childhood development globally.3
Developmental behavioral problems affect approximately 15% of children in high-income countries (HICs), and this rate is expected to be higher in low-middle-income countries (LMICs).7 Pediatricians are crucial in preventing, identifying, and properly referring these conditions. Friedman, who used the definition “behavioral pediatrics” for the first time, asserted in 1975 that this field encompassed prevention, advocacy, delivering integrative healthcare, and clinical administration in addition to dealing with psychological, social, and learning problems. The need for a subspecialty with a central role in these fields was emphasized among pediatric departments.8,9 The American Board of Medical Specialties accepted the developmental-behavioral pediatrics (DBP) sub-specialty in 1999, despite long-standing conflict concerning department task definitions, particularly between representatives of psychiatry, neurology, and developmental and behavioral pediatric divisions.9 Developmental-behavioral pediatrics has been accepted as a subspecialty in Türkiye over the last decade and efforts to improve the maturation of the department are currently ongoing. There are comprehensive studies evaluating the workforce and referral volumes of the department, as well as revealing its competition with other pediatric subspecialties in HIC where developmental pediatrics has existed for years.7,10,11 In countries where DBP has newly been established, comparable research is currently limited.12 In Türkiye, as in the rest of the world, almost all developmental pediatricians work in academic medical centers, which are tertiary-level health institutions.11 These institutions are unique facilities for training and supporting pediatric residents in all patient visits, not just throughout their rotation, and for establishing collaborations with other disciplines.13
Since 2020, the COVID-19 pandemic has affected the entire world, and data on the long-term effects of such outbreak periods, particularly on the growth and development of children, are limited.14 In addition, the stress caused by the isolation; school closures; disrupted social lives; decreased physical activity; changes in daily routines, sleeping habits, and diet; exposure to home discord; and longer screen use, all had an impact on children’s and adolescents’ physical and mental health.15 It has been demonstrated that changes in the economic, psychosocial, and educational environments since the pandemic has caused declines in children’s cognitive functions and performance, as well as negative effects on mental health.16,17 COVID-19, which is predicted to have devastating effects on early childhood development, caught countries off guard, disrupting their healthcare infrastructure. The public’s access to health services has been restricted as a result of both government’s closure measures and policies aimed at reducing population movement, as well as the resulting economic challenges. Concerns about the potential of COVID-19 infection have also exacerbated the problem.18 Reports of a decline in childhood vaccines led us to believe that access to primary healthcare has diminished, interrupting the follow-up of healthy children and pregnant women.19-21 Access to health and support services, including early intervention, has grown more limited for at-risk children who are socioeconomically, culturally, and geographically disadvantaged and have developmental issues.22,23 High-Risk Infant Follow-Up (HRIF) programs in the United States of America (USA) highlight the importance of monitoring the effectiveness of clinical services on neonatal outcomes that were interrupted during the pandemic.24 Pediatric emergency applications decreased by about half during the pandemic, whereas child mental health applications increased.25,26 It is critical to investigate changes in clinical service capacity, patient volume, and reasons for hospital admissions during the pandemic, a period marked by uncertainty. Examining referrals to child health professionals for developmental and behavioral issues allows policymakers to develop long-term strategies through a better understanding of the consequences of this process.
This study aimed to investigate the referral volume, sources, and trends of a DBP department, as well as the factors influencing these trends, in one of the largest academic centers in Türkiye, a country where DBP has been established. Additionally, we hypothesized that the COVID-19 pandemic’s devastating effect on early childhood development would significantly increase department referral trends.
Materials and Methods
The Turkish Ministry of Health formally established DBP as a subspecialty of pediatrics in 2011. The Division of DBP was established in 2013 at Hacettepe University. The department provides services to families and children based on family-centered strategies. The primary patient group is children aged between 0 and 6 years who have developmental risks and delays. Patients who present directly or through referrals from family physicians and pediatric departments are evaluated on an average of 2 months. Since its establishment, the division has had a 1-month rotation in DBP for pediatric residents, and a 3-year fellowship training in the subspecialty.
Referral data for the Division of DBP, Department of Pediatrics, Hacettepe University between May 1st, 2014, and October 21st, 2021, were used in this retrospective cohort study. Approximately 8 years of patient referral data, including the pandemic period, were analyzed. Referral resources were classified as general pediatrics, pediatric subspecialties, and non-pediatric departments. Self-referrals were not included in the study, that is, these numbers only represent referrals from other specialists. Pediatric departmental referrals with fewer than 20 total referrals were classified as ‘other’. Due to the low number of referrals, pediatric surgery, orthopedics, neurosurgery, cardiovascular surgery, and urology departments were combined under ‘pediatric surgery branches’. The main reasons for referrals were categorized collaboratively by the researchers after reviewing the content and considering the potential referral reasons identified by the American Academy of Pediatrics (AAP) for the DBP; incomplete or inappropriate referrals were not considered.27 Changes in referral sources and reasons were initially investigated on an annual basis, followed by a review of the trend of change over time since 2019, both before and after the COVID-19 pandemic. Informed consent from the families was not obtained since this study was retrospective in design. The Ethics Committee of Hacettepe University approved this study (GO 21/1261).
Statistical analyses
The age and sex of children referred to the Division of Developmental Behavioral Pediatrics, Department of Pediatrics, Hacettepe University, as well as the quantity and distribution of referrals, were analyzed using descriptive statistics. To model the temporal trend in the number of consultations, a second-degree (quadratic) polynomial regression model was applied, as the dependent variable was continuous. Both the linear and quadratic terms of the year variable were included as independent predictors. The overall significance of the model was tested using the F-test, and the statistical significance of individual coefficients was assessed based on p-values. To evaluate model fit, performance metrics such as Mean Absolute Error (MAE), Root Mean Square Error (RMSE), Akaike Information Criterion (AIC), and Bayesian Information Criterion (BIC) were calculated. In addition, graphical comparisons between observed and predicted values were conducted to assess the model’s predictive accuracy.
We analyzed the changes in the number of referrals over time for the general pediatric outpatient clinic, neonatology, pediatric genetics, and pediatric metabolism departments that request the most referrals, in 3-month periods between 2014 and 2021. The effect of COVID-19 on perinatal risk and autism spectrum disorder (ASD) risk was calculated with 95% confidence relative risk. Polynomial regression analysis was conducted using the lm function from the base stats package in R, with both linear and quadratic terms of the year variable included in the model.28,29 The “ggplot2” package were used to plot polynomial regression curves.30 A p-value of less than 0.05 was considered significant.
Results
After excluding self-referrals, over approximately 8 years, 8412 children were referred to the Division of DBP, Department of Pediatrics, Hacettepe University. 59.5% were males and 40.5% were females. The median age was 18 months.
The departments that requested the most referrals were the general pediatric outpatient clinic (31.0%), neonatology (28.2%), pediatric metabolism (9.8%), and pediatric genetics (9.8%), respectively (Table I). Child and adolescent psychiatry (3.9%) and otolaryngology (3.0%) had the most referrals among non-pediatric departments. Other pediatric subspecialties, pediatric surgical branches, and non-pediatric departments all had referral rates of less than 3%. Patients were referred to the Division of DBP, Department of Pediatrics, Hacettepe University due to perinatal and neonatal risks (33.5%), speech delay (15.7%), a likelihood of developmental delays (14.1%), and developmental evaluation of patients with metabolic disorders (7.0%), respectively. The distribution of reasons for the children’s referrals during the study period is shown in Table II.
|
*Pediatric surgery, orthopedics, neurosurgery, cardiovascular surgery, and urology **Pediatric nephrology, rheumatology, intensive care, physical medicine and rehabilitation |
|
| Table I. Numbers of referrals to the department of developmental and behavioural pediatrics from other departments between 2014 and 2021 (N=8412). | |
|
|
|
| General pediatric outpatient clinic |
|
| Neonatology |
|
| Pediatric metabolism |
|
| Pediatric genetics |
|
| Child and adolescent psychiatry |
|
| Otorhinolaryngology |
|
| Pediatric neurology |
|
| Pediatric allergy |
|
| Pediatric gastroenterology |
|
| Pediatric endocrinology |
|
| Pediatric pulmonology |
|
| Pediatric cardiology |
|
| Pediatric hematology and oncology |
|
| Pediatric immunology |
|
| Plastic and reconstructive surgery |
|
| Pediatric infectious diseases |
|
| Other surgery clinics* |
|
| Pediatric emergency |
|
| Other non-surgical clinics** |
|
| Ophthalmology |
|
| Total |
|
| Table II. Referral reasons (2014 to 2021). | |
| Reasons |
|
| Infants and children at risk due to perinatal and neonatal history |
|
| Speech delay |
|
| Children at risk of developmental delays |
|
| Developmental evaluation of patients with metabolic disease |
|
| Feeding difficulties |
|
| Developmental evaluation of patients with a genetic syndrome |
|
| Global developmental delay |
|
| Autism diagnosis or suspicion |
|
| Behavioral problems |
|
| Motor development delays |
|
| Sleep problems |
|
| Problems with toilet habits |
|
| Children considered as being gifted |
|
| Total |
|
Between 2014 and 2021, the number of referrals grew each year, the number of referrals increased from 302 in 2014 to 1394 in 2021. Even though the referrals from the last two months were not considered, the highest number of referrals was reached in 2021. The number of referrals reduced after the COVID-19 pandemic began in 2020. Comparing the number of referrals over the last 3 years, Fig. 1 shows that there was a considerable drop in referrals during the 3-month lockdown period following March 2020, the start of the outbreak and then began to rise.
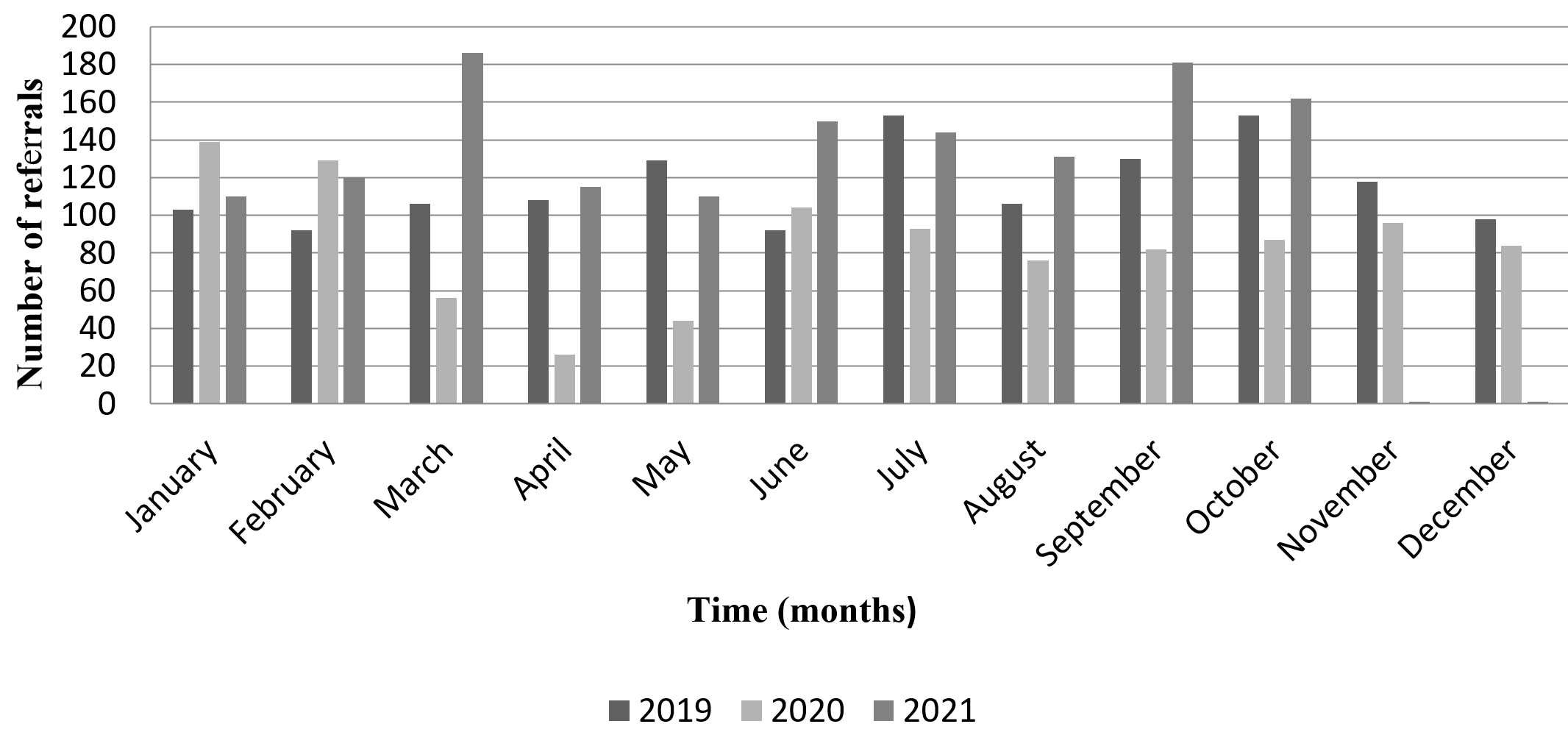
In the pre-pandemic period, the polynomial regression model revealed that both the linear (β = 37.03, p < 0.001) and quadratic (β = –0.95, p < 0.001) year terms were statistically significant. These results indicate a strong initial increase in consultation numbers, followed by a deceleration in growth and a shift toward decline around 2018. The model demonstrated excellent explanatory power, accounting for 81.0% of the variance (R2 = 0.810; Adjusted R2 = 0.792) with strong overall significance (F = 46.8, p < 0.001). Additional performance metrics included MAE = 40.77, RMSE = 48.12, AIC = 272.63, and BIC = 277.51 (Supplementary Table S1). As visualized in Fig. 2a, the number of referrals showed a consistent increase from 2014 to around 2018–2019, followed by a slight decline toward 2020. This quadratic pattern suggests a possible plateau or saturation effect in referral numbers shortly before the onset of the pandemic.
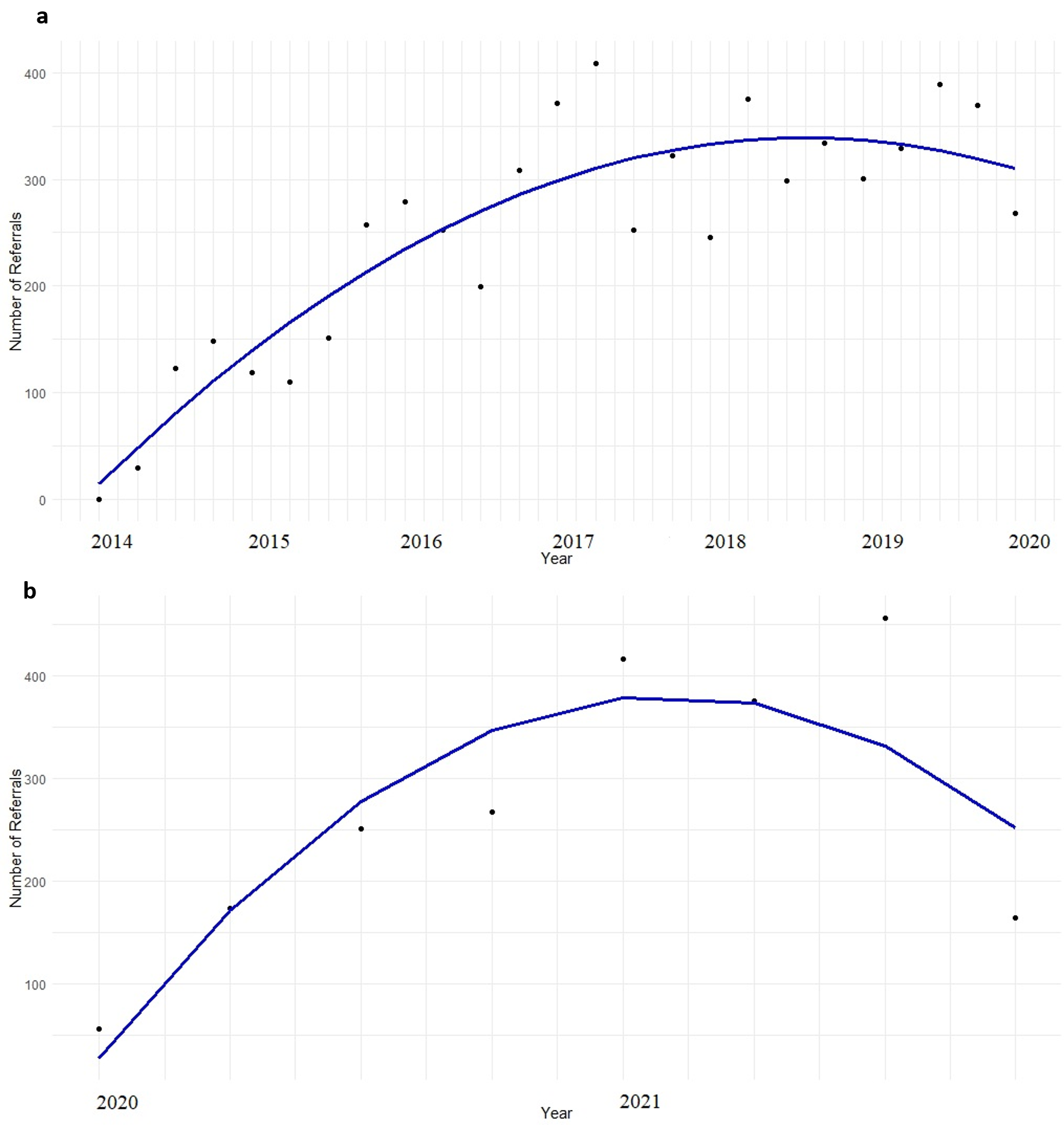
In the post-pandemic period, the polynomial regression model revealed that both the linear (β = 199.29, p = 0.02) and quadratic (β = –18.59, p = 0.03) year terms were statistically significant. These results indicate a sharp initial increase in consultation numbers, followed by a loss of momentum and a downturn beginning after 2021. The model demonstrated good explanatory power, accounting for 75.7% of the variance (R2 = 0.757; Adjusted R2 = 0.659) with overall significance (F = 7.77, p = 0.029). Model performance metrics included MAE = 48.55, RMSE = 63.76, AIC = 97.19, and BIC = 97.50 (Supplementary Table S2). As illustrated in Fig. 2b, the number of referrals increased sharply from early 2020 through 2021, reaching a peak in mid-2021. However, a noticeable decline followed, suggesting a non-linear recovery pattern. This may reflect healthcare system adaptations and fluctuations in patient behavior during the later phases of the pandemic.
The polynomial regression model for pediatric outpatient clinic referrals indicated that both the linear (β = 8.18, p = 0.004) and quadratic (β = –0.16, p = 0.044) year terms were statistically significant. These results suggest a curvilinear trend characterized by an initial increase in consultation numbers that gradually slowed and leveled off over time. The model explained 47.5% of the variance (R2= 0.475; Adjusted R2 = 0.439) and was overall statistically significant (F = 13.1, p < 0.001). Model performance metrics were MAE = 24.28, RMSE = 31.09, AIC = 318.77, and BIC = 324.63 (Supplementary Table S3). As illustrated in Fig. 3a, the number of pediatric referrals increased steadily between 2014 and approximately 2020, reaching a plateau, followed by a slight decline towards 2021. This non-linear trend may reflect the combined influence of service expansion during the earlier years and pandemic-related disruptions in later years.
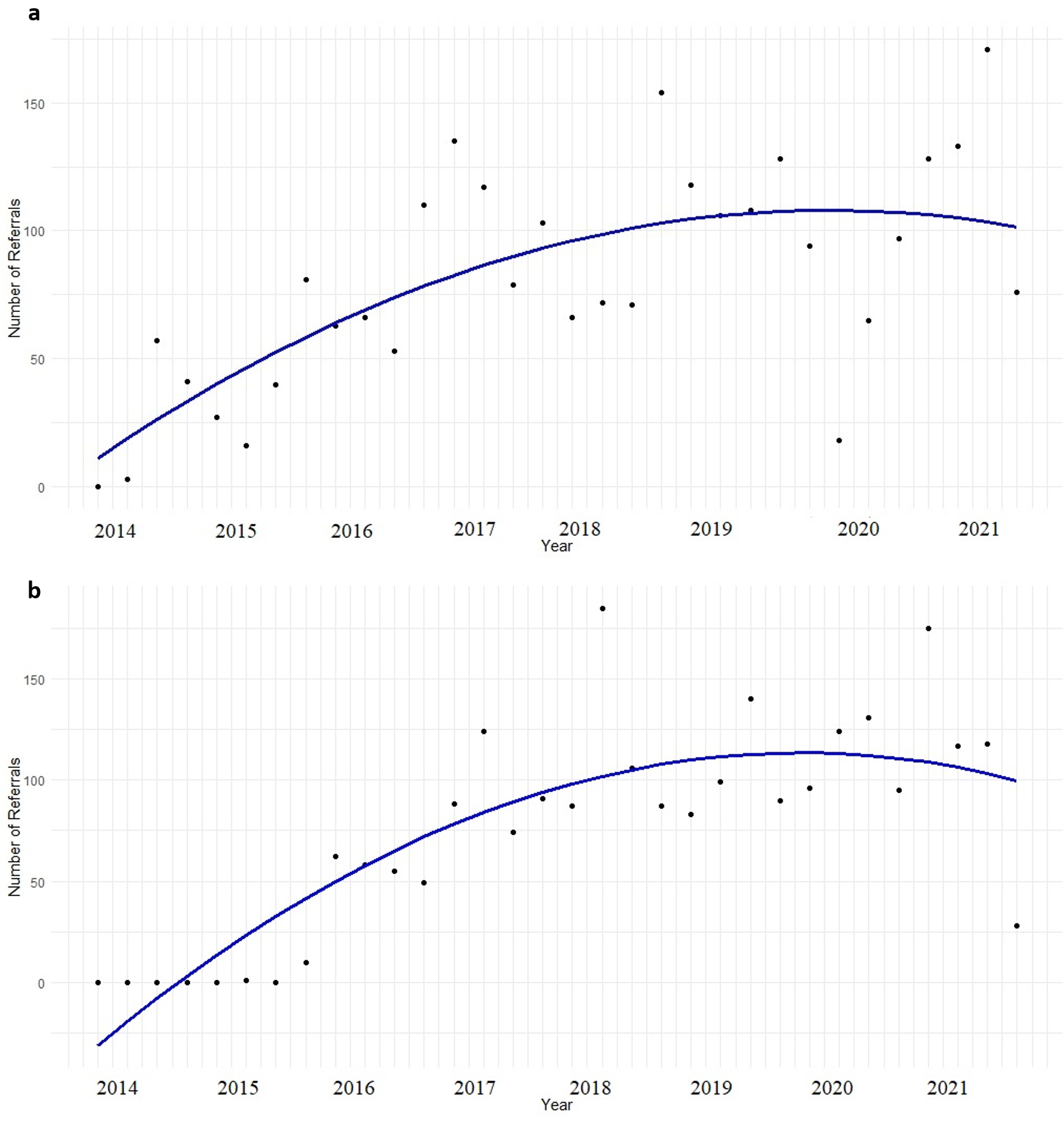
The polynomial regression model for neonatology outpatient clinic referrals demonstrated that all year-related terms were statistically significant: the intercept (β = –43.65, p = 0.018), linear term (β = 12.71, p < 0.001), and quadratic term (β = –0.26, p = 0.001). These findings indicate a clear initial increase in referrals, followed by a gradual deceleration and eventual decline, suggesting a non-linear trajectory. The model explained 69.0% of the variance (R2 = 0.690; Adjusted R2 = 0.669) and was overall statistically significant (F = 32.26, p < 0.001). Model performance indices supported this fit, with MAE = 22.10, RMSE = 29.74, AIC = 314.92, and BIC = 320.79 (Supplementary Table S4). As visualized in Fig. 3b, referral rates exhibited a steady upward trajectory from 2014 through 2020, followed by a modest decline in 2021. The significant quadratic effect suggests a nonlinear shift in referral patterns, potentially attributable to systemic changes in neonatal care provision or the indirect effects of the COVID-19 pandemic.
The relative risk was analyzed to evaluate the change in referral reasons from before the COVID-19 outbreak. Following the pandemic, the number of referrals for infants and children at risk due to perinatal and neonatal history was 1.359 (95% confidence interval: 1.269-1.456) times higher than before the pandemic. Furthermore, the number of children referred with a diagnosis or suspicion of autism was 1.209 (95% confidence interval: 0.987-1.478) times higher after the pandemic.
Discussion
This study reveals the referral trends of the DBP sub-specialty, which provides training, research, and service within one of the largest and best-equipped academic institutions in Türkiye. Furthermore, the study had to include the COVID-19 pandemic periods to evaluate the possible effects of the pandemic on developmental and behavioral issues, particularly in developing countries.
DBP training and services persisted in a few centers, one of which was an academic facility, throughout the period when referrals to the DBP, Department of Pediatrics, Hacettepe University were examined between 2014 and 2021. In Türkiye, a similar two-center study reported an annual 1.18-fold increase (95% confidence interval: 1.09-1.28) in DBP referrals between 2010 and 2017.12 The number of referrals increased rapidly in the pre-pandemic period, peaked in 2018, and declined toward 2020, reaching a low point during the pandemic. Following an initial post-pandemic surge, a marked decline was observed after mid-2021, indicating an early recovery that later lost momentum. These trends likely reflect the expansion and eventual saturation of the division’s services and workforce over time. Additionally, given that the number of referrals in longitudinal studies evaluating the DBP workforce trend in HICs has mostly remained constant in recent years, it is clear that the demand for DBP training programs, research, and services will continue to grow in countries where DBP’s have recently been established.10,11
A significant upward trend was observed in pediatric outpatient clinic referrals from 2014 to 2020, followed by a slight decline in 2021. This pattern suggests that the rapid increase in referrals may have reached a plateau. In a comprehensive study conducted in the USA, pediatric generalists were responsible for the majority of referrals to the DBP for both time points.10 This improvement in awareness is quite encouraging, given the critical requirement of a developmental perspective in pediatrics and the lack of knowledge of pediatric residents on psychological and developmental issues.5,27,31 We believe that time and rotation training was the most effective factors in this trend in referrals. As a result, the establishment of DBPs in developing countries, the increase in the number of training and service institutions, and subsequently, the support and collaboration of DBP specialists with young pediatricians throughout their residency training in chronic/inpatient follow-ups, as well as DBP rotations, allows them to improve their necessary knowledge and skills about developmental issues before serving in primary care.13
The model for neonatal outpatient referrals demonstrated a sharp upward trend beginning in 2016, which plateaued and showed a slight decline after 2020, indicating a deceleration and eventual reversal in referral growth. Likewise, referrals from the neonatology department and perinatal risk-related referrals ranked first in a multicenter study analyzing referrals to DBP outpatient clinics in Türkiye.32 In HICs, the number of neonatal follow-up referrals is relatively low.5,10 This condition in developing countries is likely to be attributed to an increase in high- risk babies, caused by the inability to entirely remove maternal social, environmental, and biological risk factors, as well as improved neonatal survival and limited health services in rural regions.33,34 There is a definite need for policies that will improve mother and newborn health as well as health services. Furthermore, the high and growing awareness of the neonatal department, which serves a growing population of high-risk infant patients, is of utmost importance. The most common reasons for referral, after perinatal issues, were children with speech delays and developmental delay risk. A longitudinal study of pediatricians’ developmental screening and referral trends in the USA reported that most referrals to a developmental or medical specialist were due to developmental delays in milestones and global developmental delays.5
DBP is a subspecialty that addresses the possible causes of complicated developmental and behavioral issues among children and uses system-based practices and neurodevelopmental approaches to achieve optimal developmental outcomes. Neurologists, child psychiatrists, DBP professionals, and physical medicine and rehabilitation specialists frequently collaborate in the care of children with behavioral, developmental, and learning difficulties, which have become much more common worldwide.27 The multidisciplinary nature of DBP education and practice is essential. Unfortunately, since the establishment of DBP, specialists working in this discipline have remarked that they face competition with other pediatric subspecialists and practice constraints due to a lack of clinical support from other professionals.7,10,11 According to research, pediatric subspecialists screen and refer children and their families for psychological concerns at an extremely low rate.31 However, it is well-known that the majority of children followed in these subspecialties have chronic medical conditions and are at high risk for developmental and behavioral problems, and family-level psychosocial stressors.35 Most pediatric subspecialties, as well as child and adolescent psychiatry, had referral rates of less than 5% in this study. It is well-known that collaboration practices between various disciplines and professions are linked with improved health outcomes, accordingly, we need appropriate strategies to reduce potential competition, recognize DBP’s education, service, advocacy, and research roles in pediatrics, and ensure effective collaborations.36,37 Given that the majority of DBP specialists in countries where the division was newly established are university-based, improved awareness and collaboration of other pediatric subspecialties in these institutions will eventually have a positive influence on primary care services.
The policies associated with the global COVID-19 pandemic caused negative implications at the level of children, families, and services, leading to physical, mental, and developmental issues in children, increased parental anxieties and household stress, and restricted access to healthcare.22 The pandemic has resulted in a decline in vaccine orders and vaccination admissions, according to reports from the Centers for Disease Control and Prevention (CDC).19 Diminished vaccine administrations and, as a consequence, interruptions in well-child follow-up could preclude the diagnosis of developmental delays and referral to early intervention programs for children, who are the most vulnerable to the pandemic’s devastating effects.38 These potential morbidities in children are likely to occur more frequently in developing countries, where healthcare restrictions and economic challenges are more severe. In this study, the number of referrals steadily increased after 2014, reaching its peak in 2018, followed by a plateau and subsequent decline. Following a sharp drop to its lowest levels during the pandemic, referral numbers began to rise again in the post-pandemic period. This demonstrates that the pandemic’s detrimental effects on access to healthcare are being mitigated. Furthermore, as compared with the pre-pandemic period, the increase in referrals due to perinatal risk was a remarkable finding in our research. As shown by studies, pregnant women are minimizing their pregnancy follow-up checkups because of concerns about the danger of COVID-19 infection39, and they are experiencing significant mental health issues, particularly depression and anxiety symptoms, as a result of pandemic-related conditions.40 Additionally, access to healthcare may have negatively affected maternal, fetal, and neonatal health22,41, increasing the number of high-risk babies and the requirement for follow-up. According to comprehensive studies, there would be a significant increase in maternal and child deaths in LMICs if the deterioration in healthcare during the pandemic is not resolved and the health system’s sustainability is not preserved.18
ASD is a biologically based neurodevelopmental disorder with an increasing frequency, characterized by persistent deficits in social communication and social interaction. In the USA, ASD was diagnosed in one in every 59 children in 2018.42 Identification of this increasingly prevalent disorder, as well as enrolment of children in early intervention services, improves outcomes and reduces long-term costs for families and governments.43,44 Even though the necessity of face-to-face field evaluations in the autism diagnostic process is well known, the barriers and solutions in autism examinations during the outbreak are being challenged all over the world.45,46 Telehealth has recently been adopted for DBP monitoring, mainly in HICs.47,48 Clinic access for children with suspected or diagnosed autism may be further prolonged in Türkiye where healthcare interruptions and social inequalities are more severe and telehealth services cannot be structured. The accumulation of children who cannot receive health services due to these disadvantages may be the cause of the 1.209-fold increase in referrals requested from our department with the suspicion of autism after the pandemic. Children lost opportunities for social interaction with their peers as a result of social distancing measures within their daily life during the pandemic period, and their social skills regressed. Parent-child interactions were also damaged by the chaotic home environment caused by school closures, parental jobs lost, economic challenges, or the requirement of working from home.38,49,50 Furthermore, during the pandemic, children’s screen time increased.51,52 Significant longitudinal research has indicated that screen time in 1-year-olds is associated with ASD and autism-like symptoms.53,54 All of these potential consequences could have resulted in an increase in DBP referrals for suspected autism. It will take time to determine the potential impact of the COVID-19 outbreak on the prevalence of autism and our study’s findings draw attention to this emerging topic.
One of the study’s strengths is that our center is one of the three major academic institutions providing residency training and family-centered services in the field of DBP in Türkiye and it analyses patient referrals over an 8-year period. The changes in the numbers and reasons for referrals, as well as the departments that request them, over time, indicate that developing strategies and collaborations for both our department and countries where DBP will be re-established is recommended. Another strength of our study is that it is the first to evaluate DBP referrals during the COVID-19 pandemic, demonstrating the pandemic’s potential deleterious impacts on early childhood, including at-risk children. The fact that it was a single-center study can be considered a limitation, despite the fact that it was conducted in one of the rare and comprehensive academic centers where a DBP clinic is located. One further limitation of the study is the lack of data on the crucial final diagnosis. Additional research on diagnostic processes or delays in diagnosis in DBP clinics could contribute to the body of literature.
We believe that time and assistant rotations were the most critical factors in the significant increase in referrals following the establishment of the DBP department. It is possible that the services and training we provide are in response to a lack of knowledge and support in pediatric practice regarding developmental difficulties. This should be encouraging to countries where DBPs will be established. To effectively meet awareness and referral increases, interdisciplinary collaborations should be established and practices that will improve productivity should be planned, given the limited DBP workforce in countries where the division has newly been established. Although it is encouraging that our referral trends have improved in the 1.5 years since the COVID-19 pandemic, health service constraints may have caused a considerable increase in prenatal risk and suspicion of autism referrals to our department following the pandemic. Identifying the pandemic’s indirect effects is critical for policymakers. Governments in developing countries should improve their healthcare systems to prevent the long-term detrimental impacts of periodic interruptions in healthcare on children’s development and behavior.
Ethical approval
The study was approved by Ethics Committee of Hacettepe University Faculty of Medicine (date: 07.12.2021, number: GO21/1261).
Source of funding
The authors declare the study received no funding.
Conflict of interest
The authors declare that there is no conflict of interest.
References
- Black MM, Walker SP, Fernald LC, et al. Early childhood development coming of age: science through the life course. Lancet 2017; 389: 77-90. https://doi.org/10.1016/S0140-6736(16)31389-7
- Ertem IO, World Health Organization (WHO). Developmental difficulties in early childhood: prevention, early identification, assessment and intervention in low-and middle-income countries: a review. Geneva, Switzerland: WHO; 2012. Available at: https://www.who.int/publications/i/item/9789241503549
- Richter LM, Daelmans B, Lombardi J, et al. Investing in the foundation of sustainable development: pathways to scale up for early childhood development. Lancet 2017; 389: 103-118. https://doi.org/10.1016/S0140-6736(16)31698-1
- Çelen Yoldaş T, Özmert EN, Bayazıt Y, Tanrıkulu B, Yetim H, Çakır B. Developmental concerns, parental perceptions and missed opportunities from different levels of health centers in a middle-income country. Indian J Pediatr 2021; 88: 16-22. https://doi.org/10.1007/s12098-020-03302-2
- Lipkin PH, Macias MM, Baer Chen B, et al. Trends in pediatricians’ developmental screening: 2002–2016. Pediatrics 2020; 145: e20190851. https://doi.org/10.1542/peds.2019-0851
- Belamarich PF, Gandica R, Stein RE, Racine AD. Drowning in a sea of advice: pediatricians and American Academy of Pediatrics policy statements. Pediatrics 2006; 118: e964-e978. https://doi.org/10.1542/peds.2006-0652
- Bridgemohan C, Bauer NS, Nielsen BA, et al. A workforce survey on developmental-behavioral pediatrics. Pediatrics 2018; 141: e20172164. https://doi.org/10.1542/peds.2017-2164
- Friedman SB. Behavioral pediatrics: interaction with other disciplines. J Dev Behav Pediatr 1985; 6: 202-214. https://doi.org/10.1097/00004703-198506040-00007
- Haggerty RJ, Friedman SB. History of developmental-behavioral pediatrics. J Dev Behav Pediatr 2003; 24: S1-S18. https://doi.org/10.1097/00004703-200302001-00001
- Roizen NJ, Ruch-Ross HS, Bauer NS, et al. Developmental-behavioral pediatrics 13 years after the first board certification: evolving subspecialty. J Dev Behav Pediatr 2021; 42: 83-90. https://doi.org/10.1097/DBP.0000000000000876
- Rimsza ME, Ruch-Ross HS, Clemens CJ, Moskowitz WB, Mulvey HJ. Workforce trends and analysis of selected pediatric subspecialties in the United States. Acad Pediatr 2018; 18: 805-812. https://doi.org/10.1016/j.acap.2018.04.008
- Bingoler Pekcici EB, Gumus Dogan D, Ozalp Akin E, et al. Referral trends in two pioneering developmental-behavioral pediatric centers in Turkey. J Dev Behav Pediatr 2021; 42: 227-233. https://doi.org/10.1097/DBP.0000000000000881
- Stein RE. Are we on the right track? Examining the role of developmental behavioral pediatrics. Pediatrics 2015; 135: 589-591. https://doi.org/10.1542/peds.2014-3274
- Araújo LA, Veloso CF, Souza MC, Azevedo JMC, Tarro G. The potential impact of the COVID-19 pandemic on child growth and development: a systematic review. J Pediatr (Rio J) 2021; 97: 369-377. https://doi.org/10.1016/j.jped.2020.08.008
- Wang G, Zhang Y, Zhao J, Zhang J, Jiang F. Mitigate the effects of home confinement on children during the COVID-19 outbreak. Lancet 2020; 395: 945-947. https://doi.org/10.1016/S0140-6736(20)30547-X
- Deoni S, Beauchemin J, Volpe A, D’Sa V. Impact of the COVID-19 pandemic on early child cognitive development: initial findings in a longitudinal observational study of child health. Medrxiv [Preprint] 2021: 2021.08.10.21261846. https://doi.org/10.1101/2021.08.10.21261846
- Samji H, Wu J, Ladak A, et al. Review: mental health impacts of the COVID-19 pandemic on children and youth - a systematic review. Child Adolesc Ment Health 2022; 27: 173-189. https://doi.org/10.1111/camh.12501
- Roberton T, Carter ED, Chou VB, et al. Early estimates of the indirect effects of the COVID-19 pandemic on maternal and child mortality in low-income and middle-income countries: a modelling study. Lancet Glob Health 2020; 8: e901-e908. https://doi.org/10.1016/S2214-109X(20)30229-1
- Santoli JM, Lindley MC, DeSilva MB, et al. Effects of the COVID-19 pandemic on routine pediatric vaccine ordering and administration - United States, 2020. MMWR Morb Mortal Wkly Rep 2020; 69: 591-593. https://doi.org/10.15585/mmwr.mm6919e2
- Bramer CA, Kimmins LM, Swanson R, et al. Decline in child vaccination coverage during the COVID-19 pandemic - Michigan Care Improvement Registry, May 2016-May 2020. Am J Transplant 2020; 20: 1930-1931. https://doi.org/10.1111/ajt.16112
- Langdon-Embry M, Papadouka V, Cheng I, Almashhadani M, Ternier A, Zucker JR. Notes from the field: rebound in routine childhood vaccine administration following decline during the COVID-19 pandemic - New York City, March 1-June 27, 2020. MMWR Morb Mortal Wkly Rep 2020; 69: 999-1001. https://doi.org/10.15585/mmwr.mm6930a3
- Goldfeld S, O’Connor E, Sung V, et al. Potential indirect impacts of the COVID-19 pandemic on children: a narrative review using a community child health lens. Med J Aust 2022; 216: 364-372. https://doi.org/10.5694/mja2.51368
- Eapen V, Hiscock H, Williams K. Adaptive innovations to provide services to children with developmental disabilities during the COVID-19 pandemic. J Paediatr Child Health 2021; 57: 9-11. https://doi.org/10.1111/jpc.15224
- Panda S, Somu R, Maitre N, Levin G, Singh AP. Impact of the coronavirus pandemic on High-Risk Infant Follow-Up (HRIF) programs: a survey of academic programs. Children (Basel) 2021; 8: 889. https://doi.org/10.3390/children8100889
- Lazzerini M, Barbi E, Apicella A, Marchetti F, Cardinale F, Trobia G. Delayed access or provision of care in Italy resulting from fear of COVID-19. Lancet Child Adolesc Health 2020; 4: e10-e11. https://doi.org/10.1016/S2352-4642(20)30108-5
- Cheek JA, Craig SS, West A, Lewena S, Hiscock H. Emergency department utilisation by vulnerable paediatric populations during the COVID-19 pandemic. Emerg Med Australas 2020; 32: 870-871. https://doi.org/10.1111/1742-6723.13598
- Weitzman CC, Baum RA, Fussell J, et al. Defining developmental-behavioral pediatrics. Pediatrics 2022; 149: e2021054771. https://doi.org/10.1542/peds.2021-054771
- Venables WN, Ripley BD. Modern applied statistics with S. New York: Springer; 2002. https://doi.org/10.1007/978-0-387-21706-2_14
- R Core Team. R: a language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2024.
- Wickham H, Chang W, Wickham MH. ggplot2: create elegant data visualisations using the grammar of graphics. Version 2.1. 2016.
- Green C, Stein RE, Storfer-Isser A, et al. Do subspecialists ask about and refer families with psychosocial concerns? A comparison with general pediatricians. Matern Child Health J 2019; 23: 61-71. https://doi.org/10.1007/s10995-018-2594-y
- Pekcici EBB, Sucakli A, Elitok K, et al. Addressing early childhood development and developmental difficulties in Turkey: a training programfor developmental pediatrics units. Arch Argent Pediatr 2020; 118: e384-e391. https://doi.org/10.5546/aap.2020.eng.e384
- Vaivada T, Gaffey MF, Bhutta ZA. Promoting early child development with interventions in health and nutrition: a systematic review. Pediatrics 2017; 140: e20164308. https://doi.org/10.1542/peds.2016-4308
- Olusanya BO, Davis AC, Wertlieb D, et al; Global Research on Developmental Disabilities Collaborators. Developmental disabilities among children younger than 5 years in 195 countries and territories, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Glob Health 2018; 6: e1100-e1121. https://doi.org/10.1016/S2214-109X(18)30309-7
- Perrin JM, Anderson LE, Van Cleave J. The rise in chronic conditions among infants, children, and youth can be met with continued health system innovations. Health Aff (Millwood) 2014; 33: 2099-2105. https://doi.org/10.1377/hlthaff.2014.0832
- World Health Organization (WHO). Framework for action on interprofessional education and collaborative practice. Geneva, Switzerland: WHO; 2010. Available at: https://www.who.int/publications/i/item/framework-for-action-on-interprofessional-education-collaborative-practice
- Kelly DP. Interdisciplinary collaborative future for developmental-behavioral pediatrics: barriers and opportunities. J Dev Behav Pediatr 2013; 34: 523-528. https://doi.org/10.1097/DBP.0b013e31829d1f44
- Irwin M, Lazarevic B, Soled D, Adesman A. The COVID-19 pandemic and its potential enduring impact on children. Curr Opin Pediatr 2022; 34: 107-115. https://doi.org/10.1097/MOP.0000000000001097
- Doncarli A, Araujo-Chaveron L, Crenn-Hebert C, et al. Impact of the SARS-CoV-2 pandemic and first lockdown on pregnancy monitoring in France: the COVIMATER cross-sectional study. BMC Pregnancy Childbirth 2021; 21: 799. https://doi.org/10.1186/s12884-021-04256-9
- Iyengar U, Jaiprakash B, Haitsuka H, Kim S. One year into the pandemic: a systematic review of perinatal mental health outcomes during COVID-19. Front Psychiatry 2021; 12: 674194. https://doi.org/10.3389/fpsyt.2021.674194
- Yoshikawa H, Wuermli AJ, Britto PR, et al. Effects of the global coronavirus disease-2019 pandemic on early childhood development: short- and long-term risks and mitigating program and policy actions. J Pediatr 2020; 223: 188-193. https://doi.org/10.1016/j.jpeds.2020.05.020
- Baio J, Wiggins L, Christensen DL, et al. Prevalence of autism spectrum disorder among children aged 8 years - autism and developmental disabilities monitoring network, 11 sites, United States, 2014. MMWR Surveill Summ 2018; 67: 1-23. https://doi.org/10.15585/mmwr.ss6706a1
- Fuller EA, Kaiser AP. The effects of early intervention on social communication outcomes for children with autism spectrum disorder: A Meta-analysis. J Autism Dev Disord 2020; 50: 1683-1700. https://doi.org/10.1007/s10803-019-03927-z
- Cidav Z, Munson J, Estes A, Dawson G, Rogers S, Mandell D. Cost offset associated with early start denver model for children with autism. J Am Acad Child Adolesc Psychiatry 2017; 56: 777-783. https://doi.org/10.1016/j.jaac.2017.06.007
- McNally Keehn R, Tomlin A, Ciccarelli MR. COVID-19 pandemic highlights access barriers for children with autism spectrum disorder. J Dev Behav Pediatr 2021; 42: 599-601. https://doi.org/10.1097/DBP.0000000000000988
- Zwaigenbaum L, Bishop S, Stone WL, et al. Rethinking autism spectrum disorder assessment for children during COVID-19 and beyond. Autism Res 2021; 14: 2251-2259. https://doi.org/10.1002/aur.2615
- Srinivasan R, Wallis KE, Soares N. Global trends in telehealth among clinicians in developmental-behavioral pediatric practice: a COVID-19 snapshot. J Dev Behav Pediatr 2022; 43: 32-37. https://doi.org/10.1097/DBP.0000000000000963
- Wallis KE, Mulé C, Mittal S, et al. Use of telehealth in fellowship-affiliated developmental behavioral pediatric practices during the COVID-19 pandemic. J Dev Behav Pediatr 2021; 42: 314-321. https://doi.org/10.1097/DBP.0000000000000897
- Glynn LM, Davis EP, Luby JL, Baram TZ, Sandman CA. A predictable home environment may protect child mental health during the COVID-19 pandemic. Neurobiol Stress 2021; 14: 100291. https://doi.org/10.1016/j.ynstr.2020.100291
- Li X, Jiao D, Matsumoto M, et al. Home environment and social skills of Japanese preschool children pre-and post-COVID-19. Early Child Dev Care 2022; 192: 2475-2486. https://doi.org/10.1080/03004430.2021.2021896
- Lima Rocha HA, Correia LL, Leite ÁJM, et al. COVID-19 and children’s screen time in Ceará, Brazil: a repeated cross-sectional survey. J Child Media 2022; 16: 415-423. https://doi.org/10.1080/17482798.2021.2007967
- Farah R, Zivan M, Niv L, Havron N, Hutton J, Horowitz-Kraus T. High screen use by children aged 12-36 months during the first COVID-19 lockdown was associated with parental stress and screen use. Acta Paediatr 2021; 110: 2808-2809. https://doi.org/10.1111/apa.15979
- Kushima M, Kojima R, Shinohara R, et al. Association between screen time exposure in children at 1 year of age and autism spectrum disorder at 3 years of age: the Japan environment and children’s study. JAMA Pediatr 2022; 176: 384-391. https://doi.org/10.1001/jamapediatrics.2021.5778
- Heffler KF, Sienko DM, Subedi K, McCann KA, Bennett DS. Association of early-life social and digital media experiences with development of autism spectrum disorder-like symptoms. JAMA Pediatr 2020; 174: 690-696. https://doi.org/10.1001/jamapediatrics.2020.0230
Copyright and license
Copyright © 2025 The Author(s). This is an open access article distributed under the Creative Commons Attribution License (CC BY), which permits unrestricted use, distribution, and reproduction in any medium or format, provided the original work is properly cited.