Abstract
Background. This study aimed to evaluate general and condition-specific quality of life in esophageal atresia (EA) patients, identifying risk factors such as associated anomalies and chronic diseases, as well as examining their impact on life quality.
Methods. Patients operated on for EA between 2004 and 2020 comprised the study population. Pediatric Quality of Life (PedsQOL 4.0) and the Esophageal Atresia Quality of Life (EA-QOL) questionnaires were administered to parents of 2-7 year old children as well as both patients aged 8-17 year and their parents. Results of the PedsQOL 4.0 scale were compared with 43 healthy children.
Results. The study included 66 patients (40 aged 2-7 years, 26 aged 8-17 years), with 45.5% females and 54.5% males. The mean age was 7±4.4 years. Quality of life measured by EA-QOL and PedsQOL 4.0 questionnaires showed no significant differences based on patient sex, gestational age or having an anastomotic stricture. In the 8-17 age group, EA patients demonstrated significantly higher emotional scale quality of life than the healthy group (p=0.001) according to parent and child PedsQOL 4.0 questionnaire scores.
Conclusions. The better emotional functioning in the 8-17 age group supports their enhanced anxiety management. Sex, gestational age, or presence of an anastomotic stricture did not impact quality of life. While differences existed between patient age groups in the questionnaires administered, factors like anatomical EA type, repair mode, low birth weight, tracheomalacia, frequent lung infections, presence of associated vertebral, anorectal, cardiac, renal, limb anomalies and/or hydrocephalus (VACTERL-H), gastrostomy placement, and surgical interventions other than EA significantly influenced patients’ quality of life. These findings may guide implementing measures to enhance quality of life in EA patients.
Keywords: PedsQOL 4.0, EA-QOL, esophageal atresia, VACTERL-H, quality of life
Introduction
Esophageal atresia (EA) occurs at a rate of 2.4 per 10,000 live births, often accompanied by tracheoesophageal fistula (TEF) or without fistula, and involves esophageal discontinuity.1,2 Surgical repair remains the definitive treatment, with advancements in neonatal intensive care and surgical techniques leading to improved survival rates and decreased mortality rates since the first successful primary repair in 1941.3,4
Mortality rates, once high in both preoperative and postoperative periods, have now decreased to single digits.3 However, concerns have shifted towards long-term morbidity and quality of life issues persisting into adulthood.2 These include esophageal, gastrointestinal, pulmonary diseases, and developmental problems, significantly impacting patients and their families.5-7
Analyzing the relationship between postoperative physical development and their quality of life can significantly enhance the understanding of factors influencing the developmental process, the nature, and importance of the disease, thereby improving appropriate care and treatment outcomes.8 Due to the limited applicability of questions used to assess health-related quality of life (HRQOL) in EA patients, there has been a need to develop a condition-specific quality of life questionnaire. In a study conducted in 2018 in Sweden and Germany, specific HRQOL questions under the name Esophageal Atresia Quality of Life (EA-QOL) questionnaire9 tailored for EA patients was developed and the validity was demonstrated. In a study conducted in Türkiye in 2021, the Turkish feasibility and validity of both age- and disease-specific EA-QOL questionnaire items, originated from Sweden and Germany, were demonstrated.10
The quality of life of patients who have undergone surgery for EA can be improved through early intervention, effective treatment methods, and surgical procedures, which enhance the physical health, nutritional status, and social development of children. Such a hypothesis can be further tested through more detailed research to examine the impact of the postoperative recovery process on the general health and quality of life of these children.
As a rare disease, long-term quality of life in EA patients has not been studied extensively in the medical literature. Furthermore, the degree of development of a country and the sociocultural background of its people have an impact on the perceived quality of life, with culture explaining 15.9% of the variance obtained in one study.11 This study aims to evaluate the overall and condition-specific quality of life in EA patients who are under follow-up in a single unit in Türkiye. By, including accompanying anomalies and chronic illnesses as potential risk factors on life quality, the study seeks to enhance our understanding of EA’s impact and improve treatment outcomes
Materials and Methods
On 09/07/2022, an institutional ethics committee approval was granted under the decision number 2022/0507. The study included EA patients who were born and surgically treated between October 2004 and October 2020, and whose esophageal definitive surgery was performed at our pediatric surgical clinic. Demographic data, presence of VACTERL-H (vertebral anomalies, anorectal malformation, cardiac anomalies, TEF, renal anomalies, limb anomalies, and hydrocephalus) association and other anomalies, complications, surgical procedures performed, and radiological imaging data were retrospectively collected from hospital databases and patient records. EA is classified according to the Gross classification as follows: Type A: Isolated EA, in which both the proximal and distal esophageal segments end blindly without any tracheoesophageal fistula. Type B: EA with a proximal TEF and a blind-ending distal esophagus. Type C: EA with a blind-ending proximal esophagus and a distal TEF (the most common type). Type D: EA with both proximal and TEF. Type E: TEF without EA, also referred to as an “H-type” fistula.12
The study was conducted in accordance with the declaration of Helsinki. The legal guardians of the patients were informed of the purpose and content of the research. Written informed consent for participation in the study was obtained from patients aged >7 years as well as their parents by face-to-face intervention during regular outpatient clinic follow-up visits. This was followed by administration of the questionnaire. For patients who did not present to the outpatient clinic during the study period, verbal consent was obtained via telephone and the questionnaire was conducted remotely by the principal author.
Additionally, The Pediatric Quality of Life (PedsQOL 4.0) questionnaire was administered to healthy volunteers. These were children and the relevant proxies of volunteering hospital staff who were initially matched according to patient age groups. The questionnaires were conducted either face-to-face after obtaining written informed consent or by telephone interviews. The results were then statistically compared with the patient group.
The pediatric quality of life (PedsQOL 4.0)
The scale is designed to assess the health-related quality of life (HRQOL) of children and adolescents aged 2-17 years and consists of four main domains: Physical (8 items), Emotional (5 items), Social (5 items), and School Functioning (5 items), totaling 23 items. For children, the scale is divided into two age groups: 8-12 and 13-18 years. Additionally, there is a parent form that covers the age ranges of 2-4 and 5-7 years. Scoring is conducted through a linear conversion, where responses are converted to points as follows: 0=100, 1=75, 2=50, 3=25, and 4=0. Higher scores indicate better quality of life.13
The esophageal atresia quality of life (EA-QOL)
For children aged 2-7 years, there is a parent form, while for adolescents aged 8-17 years, both parent and child forms are available. The parent form for children aged 2-7 consists of a total of 17 questions, divided into three main categories. These include nutritional status (7 questions), physical health status (6 questions), and relationships with others (4 questions). For patients aged 8-17 years, there are a total of 24 questions, with both parents and the patient themselves providing answers. These questions are divided into four main categories. These include nutritional status (8 questions), relationships with others (7 questions), thoughts on body and scar (5 questions), and physical health status (4 questions). Responses are scored linearly on a scale of 0-100 (0-25-50-75-100). The score for each subcategory is the arithmetic average of the total scores divided by the number of items in that subcategory. The total score is obtained by dividing the total score of all items by the total number of items. The total score ranges from 0 to 100, with higher scores indicating better quality of life.14,15 The Turkish validity and reliability study of this questionnaire, developed by Dellenmark-Blom9 was conducted by Soyer et al.10 demonstrating its feasibility.
Statistical analyses
The relationship between two independent continuous variables, not normally distributed, was assessed using the Mann-Whitney U test. Categorical variables were examined using the chi-square test, with Yates continuity correction or Fisher’s exact test where applicable. Significance level was set at 0.05. Spearman rank correlation coefficient (Spearman’s rho) was used to analyze the correlation between non-normally distributed continuous variables. Statistical analyses were performed using MedCalc Statistical Software version 12.7.7 (MedCalc Software bvba, Ostend, Belgium; http://www.medcalc.org; 2013).
Results
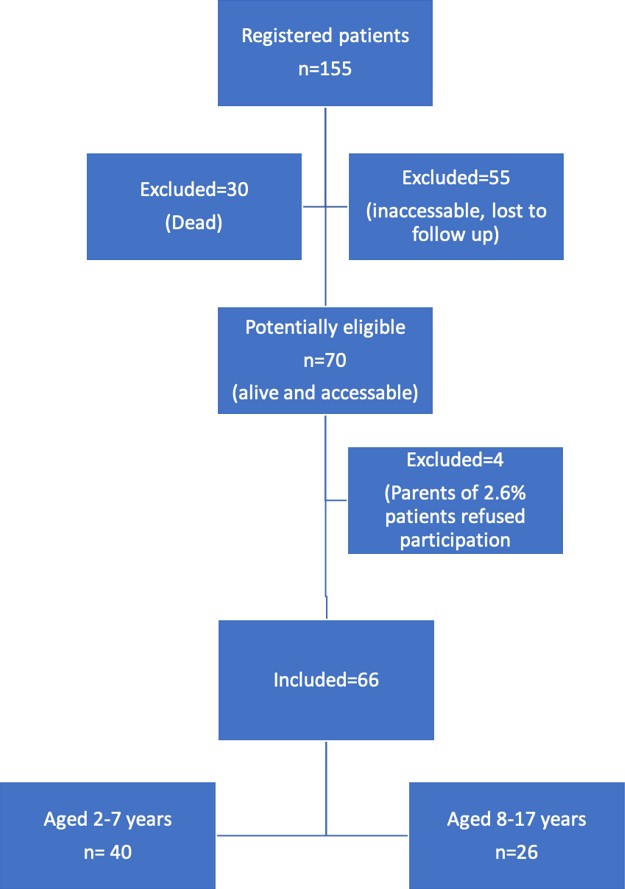
During the included time interval, 155 patients underwent surgery for EA at our clinic. Lost-to-follow-up, inaccessible (n=55) or deceased (n=30) patients were excluded. Parents of 4 patients (2.6%) refused participation. Sixty-six (42.6%) patients were included, with 40 aged 2-7 years and 26 aged 8-17 years (Fig. 1). The responses to the questionnaires were obtained during outpatient clinic visits in 34 patients and via telephone interview in 32. The demographic characteristics of the patients and their parents are summarized in Table I. Gross classification revealed 75.8% had type C EA, 15.2% type A, and others types B, D, and E. Concomitant anomalies included urinary system anomalies (25.8%), anorectal malformations (21.2%), vertebral anomalies (19.7%), limb anomalies (9.1%), major cardiac disease (7.6%), hydrocephalus (3%), and minor anomalies (21.2%). Five patients (7.6%) received special education for developmental delays. VACTERL-H association was present in 17 (25.8%) patients, and 2 (3%) had components of CHARGE (Coloboma, Heart disease, Atresia of the choanae, Retarded growth and mental development, Genital anomalies, and Ear malformations and hearing loss) syndrome. Genetic disorders were present in 2 (3%) patients, specifically homozygous mutations causing Fanconi anemia. Clinical follow-up and treatment details are summarized in Table II.
|
Sex distribution and ages were not significantly different between the patients and controls (p=0.881 and p=0.766, respectively). BMI, body mass index; SD, standard deviation. |
||
| Table I. Demographic characteristics of patients, parents and control participants (N=66). | ||
| Patients | Controls | |
| Sex, n (%) | ||
| Female |
|
|
| Male |
|
|
| Age, years (Mean±SD) |
|
|
| Height, cm (Mean±SD) |
|
|
| Weight, kg (Mean±SD) |
|
|
| BMI, kg/m2 (Mean±SD) |
|
|
| Birth weight, g (Mean±SD) |
|
|
| Gestational age, weeks (Mean±SD) |
|
|
| From twin pregnancy, n (%) |
|
|
| Has sibling, n (%) |
|
|
| Single parent, n (%) |
|
|
| Mother’s age, years (Mean±SD) |
|
|
| Mother's education level, n (%) | ||
| Elementary and middle school |
|
|
| High school and beyond |
|
|
|
145 patients were intubated for a median of 4 days (min-max: 1-115). 2Patients underwent anastomosis dilations for a median of 3 times (min-max: 1-16). EA, esophageal atresia; PSARP, posterior sagittal ano-rectoplasty |
|
| Table II. Clinical follow-up and treatment information (N=66). | |
|
|
|
| The center where first surgery was performed | |
| Our center |
|
| Other center |
|
| Esophagostomy |
|
| Placement of a gastrostomy |
|
| Preoperative gastrostomy placement for EA |
|
| Closure of gastrostomy |
|
| Primary repair |
|
| If there is primary repair | |
| Early |
|
| Late |
|
| Replacement surgery |
|
| Postoperative intubation1 |
|
| Refistula repair |
|
| Extraesophageal surgery |
|
| Fundoplication |
|
| PSARP or anoplasty |
|
| Colostomy |
|
| Colostomy closure |
|
| Major cardiac operation |
|
| Aortopexy |
|
| Duodenal atresia |
|
| Excision of esophageal diverticulum |
|
| Scoliosis surgery |
|
| Nephrectomy |
|
| Other |
|
| Tracheostomy |
|
| Tracheomalacia |
|
| Neurogenic bladder |
|
| Anastomotic stricture |
|
| Congenital esophageal stenosis |
|
| Dilation2 |
|
| Steroid administration |
|
| Resection anastomosis |
|
| Eosinophilic esophagitis |
|
| Recurrent lung infections |
|
| Scoliosis |
|
| Winged scapula |
|
The results of the EA-QOL questionnaire
The proxy report results of the EA-QOL questionnaire for children aged 2-7 years
The proxy report of the EA-QOL questionnaire for children aged 2-7 years (n=40) showed no significant differences based on Gross classification, birth weight (<2500 g, n=24), or gestational age (preterm n=16, term n=24) (Supplementary Table S1). Similarly, no significant differences were observed between those having VACTERL-H association (n=9), gastrostomy (n=15), non-EA surgeries (n=22), and those that did not (Supplementary Tables S1-S2). Patients with tracheomalacia complaints (n=7), had significantly lower scores in physical health status (median: 50, min–max: 33.3–100; p=0.019), relationships with others (median: 50, min–max: 25–83.3; p=0.001), and total (median: 60.2, min–max: 30.9–82.8; p=0.011) compared to patients without tracheomalacia. Patients experiencing frequent lung infections (n=9) had lower quality of life in the physical health status domain (median: 54.1, min–max: 33.3–79.2; p=0.002). No significant differences were observed in patients diagnosed with anastomotic stricture (n=24) or eosinophilic esophagitis (n=5) compared to those without these (Supplementary Table S3). Patients’ sex, parental education level, and presence of siblings did not create a difference (Supplementary Table S4).
The proxy report results of the EA-QOL questionnaire for children aged 8-17 years
Patients with birth weights below 2500 grams (n=15) had lower quality of life in nutritional status (median: 81.3, min–max: 59.4–100; p=0.038), and body scar (median: 81, min–max: 80–100; p=0.047) domains. No significant difference was found based on preterm (n=11) or term birth. Type C EA patients (n=20) had significantly higher quality of life in nutritional status (median: 89.1, min–max: 71.9–100; p=0.019) and total scale (median: 94.2, min–max: 79.2–100; p=0.041) compared to Type A (n=5) (Supplementary Table S6). No significant difference was observed between patients with VACTERL-H association (n=8) or anastomotic strictures (n=16) compared to those without. Patients who had a gastrostomy (n=10) had lower quality of life in nutritional status (median: 76.6, min–max: 59.4–100; p=0.002), body scar (median: 80.5, min–max: 55–100; p=0.048), and total scale (median: 81.8, min–max: 53.3–100; p=0.019). Primarily repaired patients (n=19) scored higher in nutritional status (median: 87.5, min–max: 59.4–100; p=0.018) compared to replacement surgery (Supplementary Tables S6-S7). Patients with a history of frequent lung infections (n=7) had lower quality of life in relationships with others (median: 78.6, min–max: 57.1–100; p=0.006), body scar (median: 81.3, min–max: 62.5–100; p=0.037), physical health status (median: 81.3, min–max: 62.5–100; p=0.035), and total scale (median: 81.3, min–max: 58.3–99; p=0.035) (Supplementary Table S8). Sex, parental education level, and presence of siblings did not have significant effects (Supplementary Table S9-S10).
The child report results of the EA-QOL questionnaire for children aged 8-17 years
No significant difference was observed based on birth weight (< 2500 g, n=15) or gestational age (term, n=14). No significant difference was observed in any subscale of the questionnaire between patients with Gross Type C (n=20) and Type A (n=5) (Supplementary Table S11). Presence of VACTERL-H association (n=8) or anastomotic strictures (n=16) did not create a significant difference. Patients who underwent non-EA surgical procedures (n=18) had significantly lower scores in the physical health status (median: 93.7, min–max: 56.3–100; p=0.040), and total (median: 83.8, min–max: 72.9–100; p=0.026) subscales (Supplementary Tables S11-S13). Sex, parental education level, and presence of siblings did not significantly affect the quality of life as assessed by this questionnaire (Supplementary Table S14).
The results of the PedsQOL 4.0 questionnaire
The proxy report results of the PedsQOL 4.0 questionnaire for children born with EA aged 2-7 years
Patients with a birth weight below 2500 grams (n=16) had significantly lower quality of life in terms of physical functioning (median: 68.7, min–max: 12.5–100; p=0.005), social functioning (median: 77.5, min–max: 40–100; p=0.042) and total score (median: 74.5, min–max: 48.9–97.8; p=0.037). The patients who were preterm (n=24) did not show a significant difference compared to those who were not. There was no significant difference observed based on the EA Gross classification (type C, n=30 and type A, n=5). No significant difference was found between those with and VACTERL-H association (n=9) or anastomotic strictures (n=24) compared to those without.
There was no statistically significant difference between patients who underwent gastrostomy (n=15) and those who did not. The social functioning score (median: 80, min–max: 40–100; p=0.018) of patients (n=22) who underwent non-EA surgical procedures was significantly lower. No significant difference was found in quality-of-life scales based on complaints of tracheomalacia (n=7) or frequent lung infections (n=9). The patients’ sex and parental education level did not affect the quality of life measured by this questionnaire.
The proxy report results of the PedsQOL 4.0 questionnaire for children born with EA aged 8-17 years
For EA children aged 8-17 years (n=26), according to proxy reports on the PedsQOL 4.0 questionnaire, no significant difference was found in any of the scales based on birth weight (n=15, birth weight <2500 grams) or gestational age (n=11, preterm). Presence of VACTERL-H association (n=8) yielded a lower quality of life in terms of physical functioning (median: 77.5, min–max: 31.3–100; p=0.010), social functioning (median: 80, min–max: 40–100; p=0.033), and total score (median: 74.5, min–max: 48.9–97.8; p=0.037). No significant difference was found between patients who underwent non-EA surgical procedures (n=18) or primary esophageal repair (n=19) compared to those who did not. The patients’ sex, parental education level, and the presence of siblings did not affect quality of life. There was no significant difference observed between patients with anastomotic stricture (n=16) and those without.
The child report results of the PedsQOL 4.0 questionnaire for children born with EA aged 8-17 years
No significant difference was found in any of the scales based on birth weight (n=15, birth weight <2500 grams) or gestational age (n=11, preterm). However, those with VACTERL-H association (n=8) were found to have significantly lower quality of life in terms of emotional functioning (median: 82.5, min–max: 60–100; p=0.037), social functioning (median: 95, min–max: 75–100; p=0.049), and total score (median: 75.5, min–max: 66.3–91.3; p=0.042).
There was no significant difference observed between patients who underwent non-EA surgical procedures (n=18) or primary repair (n=19) compared to those who did not. The patients’ sex, parental education level, and the presence of siblings did not affect the quality of life in this questionnaire.
Parameters resulting in statistically significant differences from both surveys are summarized in Table III.
| Scores presented as median (min-max). EA-QOL, esophageal atresia quality of life; PedsQOL, pediatric quality of life; VACTERL-H, vertebral anomalies, anorectal anomalies, cardiac anomalies, tracheoesophageal fistula, renal anomalies, limb anomalies and hydrocephalus; EA, esophageal atresia. | |
| Table III. Parameters resulting in statistically significant differences from EA-QOL questionnaire and PedsQOL 4.0 questionnaire. | |
| Significant parameters creating differences | Evaluated categories |
| EA-QOL questionnaire | |
| Proxy report for ages 2-7 | |
| Tracheomalacia |
Lower physical health status [50 (33.3-100) vs. 83.3 (37.5-100); p=0.019], Interpersonal relationships [50 (25-83.3) vs. 100 (0-100); p=0.001], Total score [60.2 (30.9-82.8) vs. 84.4 (25-100) p=0.011] |
| Frequent respiratory infections | Lower physical health status [54.1 (33.3-79.2) vs. 83.3 (37.5-100): p=0.002] |
| Proxy report for ages 8-17 | |
| Birth weight below 2500 grams | Lower nutritional status [81.3 (59.4-100) vs 89.1 (81.3-100); p=0.038] |
| Isolated EA with replacement surgery | Lower nutritional status [75 (62.5-100) vs 87.5 (59.4-100); p=0.018] |
| Gastrostomy placement |
Lower nutritional status [76.6 (59.4-100) vs. 92.2 (75-100); p=0.002], Body scar [80.5 (55-100) vs.100 (80-100); p=0.048], Total score [81.8 (58.3-100) vs. 94.7 (79.2-100); p=0.019]. |
| Frequent respiratory infections | Lower total score [81.3 (58.3-99) vs. 93.8 (72.7-100); p=0.035] |
| Child self-report for ages 8-17 | |
| Patients who underwent surgeries other than EA |
Lower physical health status [93.7 (56.3-100) vs. 100 (87.5-100); p=0.040] Total score [83.8 (72.9-100) vs. 95.8 (83.3-100);p=0.026] |
| PedsQOL 4.0 questionnaire | |
| Proxy report for ages 2-7 | |
| Birth weight below 2500 grams |
Lower physical functioning [68.7 (12.5-100) vs. 96.9 (56.3-100): p=0.005], Social functioning [77.5 (40-100) vs 100 (60-100); p=0.042] Total score [70.1 (47.8-100) vs 89.5 (60.8-100); p=0.006) |
| Patients who underwent surgeries other than EA | Lower social functioning score [80 (40-100) vs.100 (40-100); p=0.018] |
| Proxy report for ages 8-17 | |
| VACTERL-H association |
Lower physical functioning [77.5 (31.3-100) vs. (98.4 (56.3-100); p=0.010] Social functioning [80 (40-100) vs. 100 (25-100); p=0.033] Total score [74.5 (48.9-97.8) vs. 92.3 (34.8-100); p=0.037] |
| Child self-report for ages 8-17 | |
| VACTERL-H association |
Lower emotional functioning [82.5 (60-100) vs. 100 (60-100); p=0.037] Social functioning [95 (75-100) vs. 100 (25-100); p=0.049] Total score [75.5 (66.3-91.3) vs. 92.9 (55.4-100); p=0.042] |
Comparison of PedsQOL 4.0 child and parental reports with a healthy volunteer group
A comparison of the PedsQOL 4.0 patient and healthy groups was conducted. Among the healthy volunteers, 21 (48.8%) were females, and 22 (51.2%) were males. There was no statistically significant difference in sex (p=0.881) or age group distributions (p=0.766) when patients and healthy children were compared. In both parental and child reports for ages 8-17 years, EA patients scored higher on the emotional subscale (median: 90, min–max: 60–100; p<0.001) compared to the healthy group (Table IV).
|
Mann-Whitney U test. min: Minimum, max: Maximum PedsQOL, pediatric quality of life. |
|||
| Table IV. Comparison of patient and control group's PedsQOL 4.0 questionnaire results. | |||
|
|
|
|
|
| PedsQOL 4.0, 8-17 years, children |
|
|
|
| Physical functioning |
|
|
|
| Emotional functioning |
|
|
|
| Social functioning |
|
|
|
| School functioning |
|
|
|
| Total |
|
|
|
| PedsQOL 4.0, 2-7 years, proxy |
|
|
|
| Physical functioning |
|
|
|
| Emotional functioning |
|
|
|
| Social functioning |
|
|
|
| School functioning |
|
|
|
| Total |
|
|
|
| PedsQOL 4.0, 8-17 years, proxy |
|
|
|
| Physical functioning |
|
|
|
| Emotional functioning |
|
|
|
| Social functioning |
|
|
|
| School functioning |
|
|
|
| Total |
|
|
|
Discussion
The question of how EA and its associated morbidities affect long-term quality of life has been addressed previously. In 5 out of 7 evaluated studies in a review, the quality of life of EA patients was found to be impaired compared to healthy references.16
In a study conducted in Sweden and Germany, when evaluating PedsQOL 4.0 proxy reports, lower total scores were obtained compared to the healthy population. However, interestingly, EA children obtained significantly better results in the emotional and social subscales.17 In our study, when comparing the reports of children and parents aged 8-17 years with those of the healthy population, the patient group obtained better scores in the emotional subscale. The challenging medical experiences that EA patients undergo from childhood and the frequent hospital visits may result in increased anxiety and depression.18 On the other hand, children with chronic illnesses may also learn to cope better with daily stressors compared to healthy references.19 Patients with EA probably adapt to their condition at an earlier age and employ coping strategies, supporting our findings.20,21
Sex may have an effect on the results obtained. In some studies in EA patients, girls scored higher on the school scale of the PEDQOL 4.0 questionnaire compared to boys.17,22 In another study, the proxy report obtained when EA patients were 8 years old, the school functional score of female children was low.23 Male patients on the other hand in both the 8-year-old and 12-year-old groups scored higher in emotional functioning compared to females.23 In our study, no significant differences were found between sexes in any of the questionnaires.
In an assessment conducted 20 years after EA repair, the quality of life of patients who underwent primary repair was better than those who underwent colon interposition.24 Patients with colon interposition suffered more from various gastrointestinal and respiratory symptoms.24 In a pilot study, it was noted that patients with Gross type C EA who underwent primary repair had milder feeding difficulties, while those who underwent complex and complicated surgeries experienced significant feeding difficulties.25 In our study, in the proxy report of the EA-QOL questionnaire for patients aged 8-17 years, patients who underwent replacement surgery had lower scores for feeding status and total quality of life. A similar finding was reported before where parental reports of patients aged 8-17 years had lower quality of life associated with nutrition when primary anastomosis was not performed.14
The overall quality of life of EA patients showed that patients with distal fistula (Type C) scored higher in the proxy report at age 2-7 years compared to those with isolated (Type A) atresia, while no significant difference was found in the child report for patients aged 8-17 years.17 Our study partly supports this finding because distal fistula patients had higher scores in feeding and total scores in the parental report of the EA-QOL questionnaire for ages 8-17 years. However, the type of EA did not give a significant result in the same age group for the child report or in the parental report for patients aged 2-7 years. Although the reasons for the differences between studies are not entirely clear, it is possible that different levels of expectations regarding the quality of life of the family or the child could be an explanatory factor.
In cases where EA is too complex to be operated on in the neonatal period or becomes complicated due to postoperative complications, resulting in an inability to orally feed, a gastrostomy is performed. It was found that 2-7 years old patients who underwent gastrostomy scored lower on feeding status scales and their quality of life in terms of their social life was adversely affected.14 In our study, however, there was no difference in quality of life between those who underwent gastrostomy before or after EA surgery and those who did not in the proxy reports of the same age group. However, proxy reports for patients aged 8-17 years showed those who underwent gastrostomy had significantly lower scores in feeding status, body scar, and total score quality of life. Although the expected results may vary depending on age and scales, the use of gastrostomy can be considered a factor negatively affecting quality of life.
One of the most common complications following EA repair is anastomotic stricture. The treatment involves dilating the stricture by using a balloon or a bougie.26,27 While the need for anastomotic dilation is observed in approximately 36% of patients within the first 2 years after Gross type C EA surgery, there is a decrease in the need for dilation over time.28 In our study, quality-of-life scales did not differ between patients who experienced anastomotic strictures and underwent dilation compared to those without strictures. In one study, the need for dilation at least once in children aged 8-17 years was reported as a risk factor in the feeding status scale.14 Our contradicting results can be due to differences in expectations of quality of life between parents and children, inadequacy in understanding the questions, and/or less scrutiny of the problems. Furthermore, esophageal dilatations alleviate the disturbing stricture symptoms which may positively affect life quality as reported in one other study.29
In our study, presence of VACTERL-H association negatively affected the quality of life in emotional functioning, social functioning, and total subscales in the 8-17 age group according to the child report of the PedsQOL 4.0 questionnaire but not on the EA-QOL scale. A similar finding was previously attributed to the fact that the focus of EA-QOL questionnaire questions are on the upper gastrointestinal system and respiratory problems and the prioritization of the severity of anorectal or cardiac malformations rather than the number of VACTERL-H components.14
In EA patients, respiratory disorders, impairs quality of life and respiratory symptoms are found to be more common compared to healthy groups.7 Approximately 50% of EA patients are hospitalized due to respiratory tract diseases, which can have a significant impact on both children and parents, mostly in early childhood.30 Respiratory symptoms were reported to negatively affect physical health status, relationships with others, and total scores in the 2-7 age group EA-QOL questionnaire.14 Similarly, in our study, in the 8-17 age group EA-QOL parent report, patients with frequent lung infections and those with tracheomalacia findings in the 2-7 age group were observed to report negative effects on their physical health status, relationships with others, and total scores. We can conclude that respiratory tract disorders affect EA patients more in terms of physical and social aspects. Additionally, respiratory system symptoms are more commonly seen at younger ages.14 In accordance with this, tracheomalacia was not observed in the 8-17 age group in our study.
In our study, patients who underwent non-EA surgical procedures like colostomy creation and closure, surgery for anorectal malformation, fundoplication, and cardiac surgery could not be subdivided for individual assessment due to the small number of cases within groups. According to parental responses, patients were adversely affected by non-EA surgeries in social functioning in the 2-7 years PedsQOL 4.0 questionnaire and in physical health status and overall quality of life in the 8-17 years EA-QOL questionnaire. Fundoplication surgery was previously reported to have positive effects on patients’ overall quality of life.31 Surgical interventions can improve an individual’s nutrition and respiratory issues. However, complications that may arise after surgical procedures can have the opposite effect. Conditions such as incontinence or constipation that may develop after anal atresia surgery can negatively affect the patient’s quality of life socially and psychologically.32 We cannot make strict comments about the impact of individual non-EA surgical procedures because of small patient numbers.
Our study has some limitations. Due to being a single-center, the number of patients was limited, and the groups were not homogeneously distributed. Therefore, some important comorbidities like individual components of VACTERL-H association cannot be analyzed in a more detailed manner. Some others like presence of neurogenic bladder or type of cardiac anomaly could not be statistically analyzed. On the other hand, all patients in our study were followed up and treated at a single center in a similar protocol which is important for consistency in obtaining and evaluating patient data.
Conclusions
This is the first study in Türkiye which applied an evaluated both the PedsQOL 4.0 and the specific EA-QOL tools to EA patients, to our knowledge. Previous studies on the quality of life related to EA were mostly conducted in high income, western countries. The expectations regarding quality of life may be higher or at least different in such countries, potentially leading to lower perceived quality of life outcomes in patient groups. Our study is a step to improve knowledge about the perceived quality of life in individuals originating from a unique sociocultural background and afflicted with a rare disease.
Ethical approval
The study was approved by İstanbul Medeniyet University Faculty of Medicine Ethics Committee (date: 07.09.2022, number: 2022/0507).
Source of funding
The authors declare the study received no funding.
Conflict of interest
The authors declare that there is no conflict of interest.
References
- Pedersen RN, Calzolari E, Husby S, Garne E; EUROCAT Working Group. Oesophageal atresia: prevalence, prenatal diagnosis and associated anomalies in 23 European regions. Arch Dis Child 2012; 97: 227-232. https://doi.org/10.1136/archdischild-2011-300597
- Dingemann C, Eaton S, Aksnes G, et al. ERNICA Consensus Conference on the management of patients with esophageal atresia and tracheoesophageal fistula: diagnostics, preoperative, operative, and postoperative management. Eur J Pediatr Surg 2020; 30: 326-336. https://doi.org/10.1055/s-0039-1693116
- Zimmer J, Eaton S, Murchison LE, De Coppi P, Ure BM, Dingemann C. State of play: eight decades of surgery for esophageal atresia. Eur J Pediatr Surg 2019; 29: 39-48. https://doi.org/10.1055/s-0038-1668150
- Tennant PWG, Pearce MS, Bythell M, Rankin J. 20-year survival of children born with congenital anomalies: a population-based study. Lancet 2010; 375: 649-656. https://doi.org/10.1016/S0140-6736(09)61922-X
- Harmsen WJ, Aarsen FJ, van der Cammen-van Zijp MHM, et al. Developmental problems in patients with oesophageal atresia: a longitudinal follow-up study. Arch Dis Child Fetal Neonatal Ed 2017; 102: F214-F219. https://doi.org/10.1136/archdischild-2015-309976
- Rayyan M, Allegaert K, Omari T, Rommel N. Dysphagia in children with esophageal atresia: current diagnostic options. Eur J Pediatr Surg 2015; 25: 326-332. https://doi.org/10.1055/s-0035-1559818
- Nurminen P, Koivusalo A, Hukkinen M, Pakarinen M. Pneumonia after repair of esophageal atresia-incidence and main risk factors. Eur J Pediatr Surg 2019; 29: 504-509. https://doi.org/10.1055/s-0038-1675775
- Rozensztrauch A, Śmigiel R, Patkowski D. Congenital esophageal atresia-surgical treatment results in the context of quality of life. Eur J Pediatr Surg 2019; 29: 266-270. https://doi.org/10.1055/s-0038-1641597
- Dellenmark-Blom M, Dingemann J, Witt S, et al. The Esophageal-Atresia-Quality-of-Life Questionnaires: feasibility, validity and reliability in Sweden and Germany. J Pediatr Gastroenterol Nutr 2018; 67: 469-477. https://doi.org/10.1097/MPG.0000000000002019
- Soyer T, Arslan UE, Ulukaya Durakbaşa Ç, et al. Feasibility, reliability, and validity of the Turkish Version of the Esophageal-Atresia-Quality-of-Life Questionnaires to assess condition-specific quality of life in children and adolescents born with esophageal atresia. Turk J Gastroenterol 2021; 32: 640-650. https://doi.org/10.5152/tjg.2021.201005
- Molzahn AE, Kalfoss M, Schick Makaroff K, Skevington SM. Comparing the importance of different aspects of quality of life to older adults across diverse cultures. Age Ageing 2011; 40: 192-199. https://doi.org/10.1093/ageing/afq156
- Spitz L. Oesophageal atresia. Orphanet J Rare Dis 2007; 2: 24. https://doi.org/10.1186/1750-1172-2-24
- Varni JW, Seid M, Rode CA. The PedsQL: measurement model for the pediatric quality of life inventory. Med Care 1999; 37: 126-139. https://doi.org/10.1097/00005650-199902000-00003
- Dellenmark-Blom M, Quitmann J, Dingemann J, et al. Clinical factors affecting condition-specific quality-of-life domains in pediatric patients after repair of esophageal atresia: the Swedish-German EA-QOL study. Eur J Pediatr Surg 2020; 30: 96-103. https://doi.org/10.1055/s-0039-1693729
- Dellenmark-Blom M, Chaplin JE, Gatzinsky V, et al. Health-related quality of life experiences among children and adolescents born with esophageal atresia: development of a condition-specific questionnaire for pediatric patients. J Pediatr Surg 2016; 51: 563-569. https://doi.org/10.1016/j.jpedsurg.2015.09.023
- Dellenmark-Blom M, Quitmann J, Dingemann C. Health-related quality of life in patients after repair of esophageal atresia: a review of current literature. Eur J Pediatr Surg 2020; 30: 239-250. https://doi.org/10.1055/s-0040-1710389
- Flieder S, Dellenmark-Blom M, Witt S, et al. Generic health-related quality of life after repair of esophageal atresia and its determinants within a German-Swedish cohort. Eur J Pediatr Surg 2019; 29: 75-84. https://doi.org/10.1055/s-0038-1672144
- Peetsold MG, Heij HA, Deurloo JA, Gemke RJ. Health-related quality of life and its determinants in children and adolescents born with oesophageal atresia. Acta Paediatr 2010; 99: 411-417. https://doi.org/10.1111/j.1651-2227.2009.01579.x
- Hampel P, Rudolph H, Stachow R, Laß-Lentzsch A, Petermann F. Coping among children and adolescents with chronic illness. Anxiety Stress Coping 2005; 18: 145-155. https://doi.org/10.1080/10615800500134639
- Dellenmark-Blom M, Chaplin JE, Jönsson L, Gatzinsky V, Quitmann JH, Abrahamsson K. Coping strategies used by children and adolescents born with esophageal atresia - a focus group study obtaining the child and parent perspective. Child Care Health Dev 2016; 42: 759-767. https://doi.org/10.1111/cch.12372
- Dellenmark-Blom M, Chaplin JE, Quitmann JH, et al. The prevalence and role of coping strategies in the nutritional intake of children born with esophageal atresia: a condition-specific approach. Dis Esophagus 2019; 32: doz004. https://doi.org/10.1093/dote/doz004
- Meade T, Dowswell E. Health-related quality of life in a sample of Australian adolescents: gender and age comparison. Qual Life Res 2015; 24: 2933-2938. https://doi.org/10.1007/s11136-015-1033-4
- Ten Kate CA, Rietman AB, van de Wijngaert Y, et al. Longitudinal health status and quality of life after esophageal atresia repair. J Pediatr Gastroenterol Nutr 2021; 73: 695-702. https://doi.org/10.1097/MPG.0000000000003293
- Ure BM, Slany E, Eypasch EP, Weiler K, Troidl H, Holschneider AM. Quality of life more than 20 years after repair of esophageal atresia. J Pediatr Surg 1998; 33: 511-515. https://doi.org/10.1016/s0022-3468(98)90100-2
- Baird R, Levesque D, Birnbaum R, Ramsay M. A pilot investigation of feeding problems in children with esophageal atresia. Dis Esophagus 2015; 28: 224-228. https://doi.org/10.1111/dote.12178
- Tambucci R, Angelino G, De Angelis P, et al. Anastomotic strictures after esophageal atresia repair: incidence, investigations, and management, including treatment of refractory and recurrent strictures. Front Pediatr 2017; 5: 120. https://doi.org/10.3389/fped.2017.00120
- Durakbasa CU, Ersoy F, Pirim A, Oskayli MC. Clinical outcome of endoscopic balloon dilatations employed in benign paediatric oesophageal pathologies. J Minim Access Surg 2023; 19: 62-68. https://doi.org/10.4103/jmas.jmas_79_22
- Salö M, Stenström P, Anderberg M, Arnbjörnsson E. Anastomotic strictures after esophageal atresia repair: timing of dilatation during the first two postoperative years. Surg J (N Y) 2018; 4: e62-e65. https://doi.org/10.1055/s-0038-1646950
- Dellenmark-Blom M, Örnö Ax S, Öst E, et al. Postoperative morbidity and health-related quality of life in children with delayed reconstruction of esophageal atresia: a nationwide Swedish study. Orphanet J Rare Dis 2022; 17: 239. https://doi.org/10.1186/s13023-022-02381-y
- Chetcuti P, Phelan PD. Respiratory morbidity after repair of oesophageal atresia and tracheo-oesophageal fistula. Arch Dis Child 1993; 68: 167-170. https://doi.org/10.1136/adc.68.2.167
- Granderath FA, Kamolz T, Schweiger UM, Pointner R. Quality of life, surgical outcome, and patient satisfaction three years after laparoscopic Nissen fundoplication. World J Surg 2002; 26: 1234-1238. https://doi.org/10.1007/s00268-002-6416-3
- Hassink EA, Rieu PN, Brugman AT, Festen C. Quality of life after operatively corrected high anorectal malformation: a long-term follow-up study of patients aged 18 years and older. J Pediatr Surg 1994; 29: 773-776. https://doi.org/10.1016/0022-3468(94)90367-0
Copyright and license
Copyright © 2025 The Author(s). This is an open access article distributed under the Creative Commons Attribution License (CC BY), which permits unrestricted use, distribution, and reproduction in any medium or format, provided the original work is properly cited.