Abstract
Background. Umbilical arterial catheterisation is a common intervention performed in the neonatal intensive care unit (NICU) especially in extremely preterm and extremely low birth weight neonates. Rarely catheter fracture or breakage can occur, leaving behind part of the catheter in the aorta. A handful of cases have been reported in the literature, with the majority being managed surgically. There is no well-established protocol or consensus on the optimal management of such situations, leaving clinicians to rely on innovative and individualized approaches to address this critical situation.
Case Presentation. We report the successful percutaneous retrieval of a fractured umbilical artery catheter (UAC) from the aorta of a very low birth weight preterm neonate born at 28 weeks of gestation, who was undergoing treatment for neonatal sepsis at our hospital’s NICU. The fractured catheter was retrieved via the right femoral artery using an improvised snare created by double-folding and inserting a 300 cm, 0.014-inch coronary guidewire into a Judkins Right (JR) 6F coronary guide catheter, forming a loop that protruded from its distal end. Following retrieval, the patient exhibited transiently weak pulses and decreased limb movement in the accessed limb. A duplex colour Doppler scan was performed which ruled out thrombosis or dissection. It was attributed to a spasm of the common femoral artery, which recovered eventually.
Conclusion. This case demonstrates the feasibility and effectiveness of successful percutaneous removal of the fractured UAC from the aorta in very low birth weight preterm neonates and underscores the importance of innovative use of improvising hardware, appropriating it to the small size of the patient.
Keywords: umbilical artery catheter, catheter fracture, percutaneous retrieval, improvised snare technique
Introduction
Umbilical arterial catheterisation is a commonly performed procedure in the neonatal intensive care unit (NICU), especially for extremely preterm and extremely low birth weight neonates. While it is a critical intervention for monitoring and managing these fragile patients, it carries inherent risks. Potential complications include catheter tip malposition, occlusion, bacterial infections, thrombosis, perforation of vessels during insertion, and vascular compromise of lower extremities or abdominal organs.1,2 In rare and particularly challenging cases, the catheter itself may become fractured, leading to internal migration or displacement. The options for removal of these broken fragments include surgical removal or percutaneous snaring. There is no well-established protocol or consensus on the optimal management of such cases, leaving clinicians to rely on innovative and individualized approaches to address this critical situation. In this report, we present a case of a very low birth weight neonate with a fractured umbilical artery catheter (UAC) lying in the descending aorta-common iliac-internal iliac artery.
Case Presentation
With informed consent obtained from the legal guardians, we present the case of a first-born female infant from an artificially conceived twin pregnancy, delivered at 28 weeks of gestation via emergency caesarean section due to prolonged premature rupture of membranes. She was undergoing treatment in the NICU at our hospital due to very low birth weight (1030 grams), respiratory distress and early onset neonatal sepsis. Appearance, Pulse, Grimace, Activity, and Respiration (APGAR) scores at 1 minute and 5 minutes after birth were 5/10 and 9/10, respectively. The neonate was intubated in the delivery room as she did not cry immediately after birth and was on invasive mechanical ventilation for 7 hours. Early rescue surfactant was administered through an endotracheal tube. Two 3.5 Fr umbilical catheters (VygonTM) were inserted for routine blood sampling, parenteral feeding and invasive blood pressure monitoring on day 1 of life with one catheter each in the umbilical vein and umbilical artery. On day 4, both catheters were removed. However, part of the UAC, which got fractured during removal, was left in the aorta/common iliac artery and went unnoticed. Chest X-ray performed on day 22 of life to evaluate the cause of apnoea episodes revealed a fractured UAC catheter lying in the neonate’s aorta. The neonate weighed 1300 g on this day. Investigations done before the procedure ruled out infection with a leucocyte count of 10.7 x 109/L, 77% neutrophils, C-reactive protein level of 0.57 mg/L and a sterile blood culture. Owing to a high surgical risk, the neonate was referred to us for percutaneous catheter retrieval.
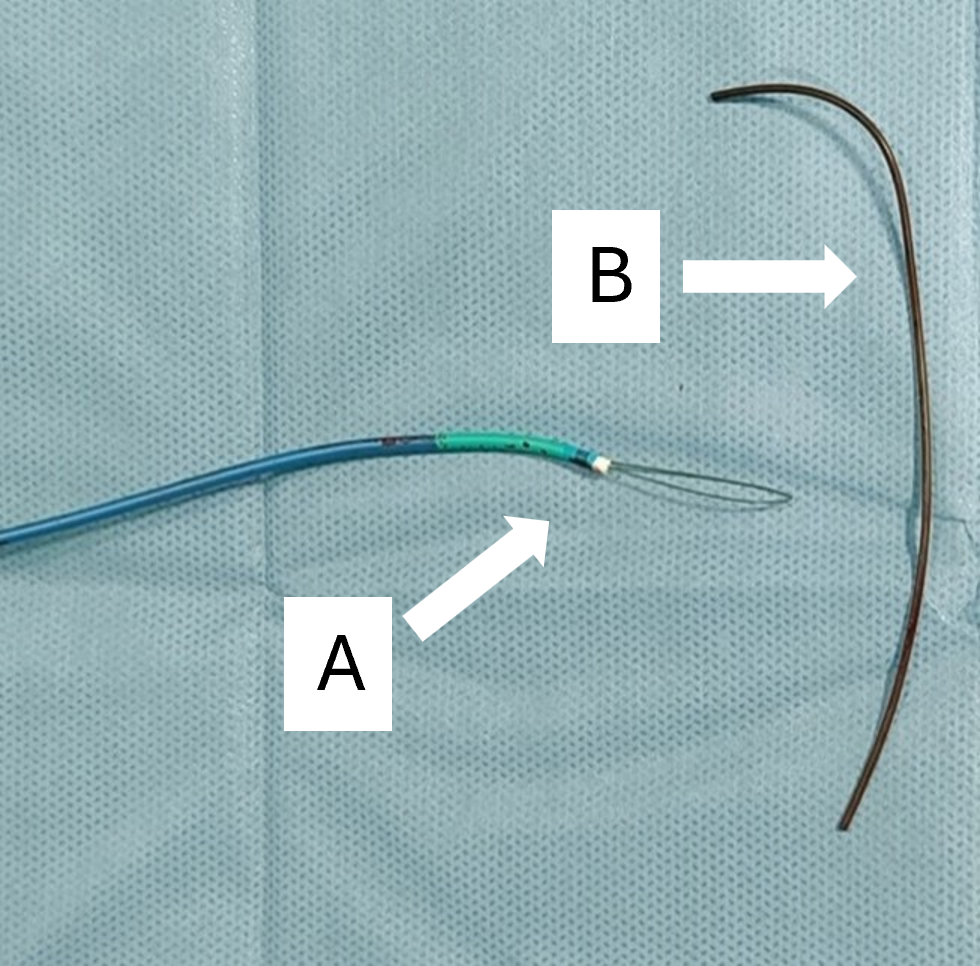
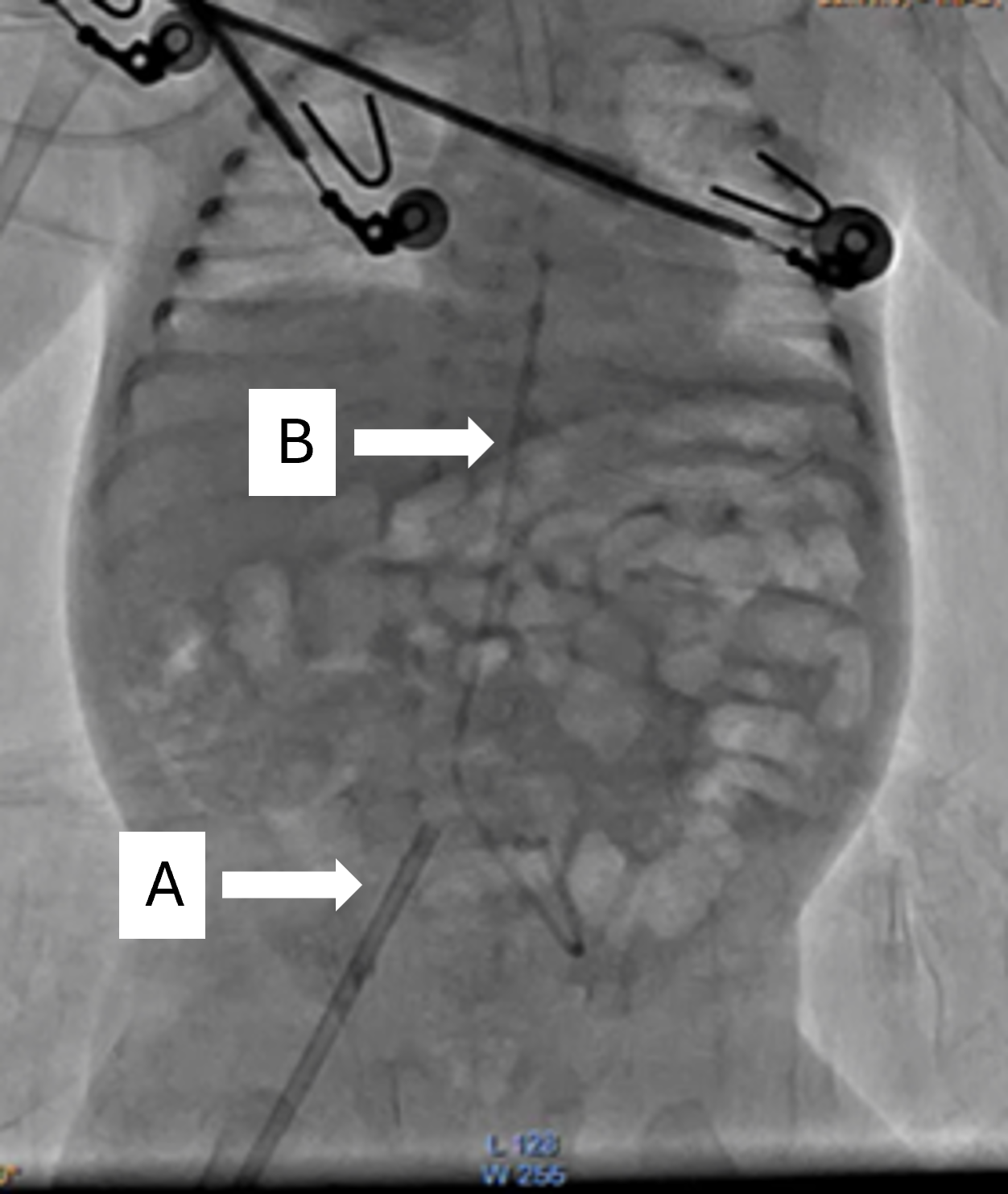
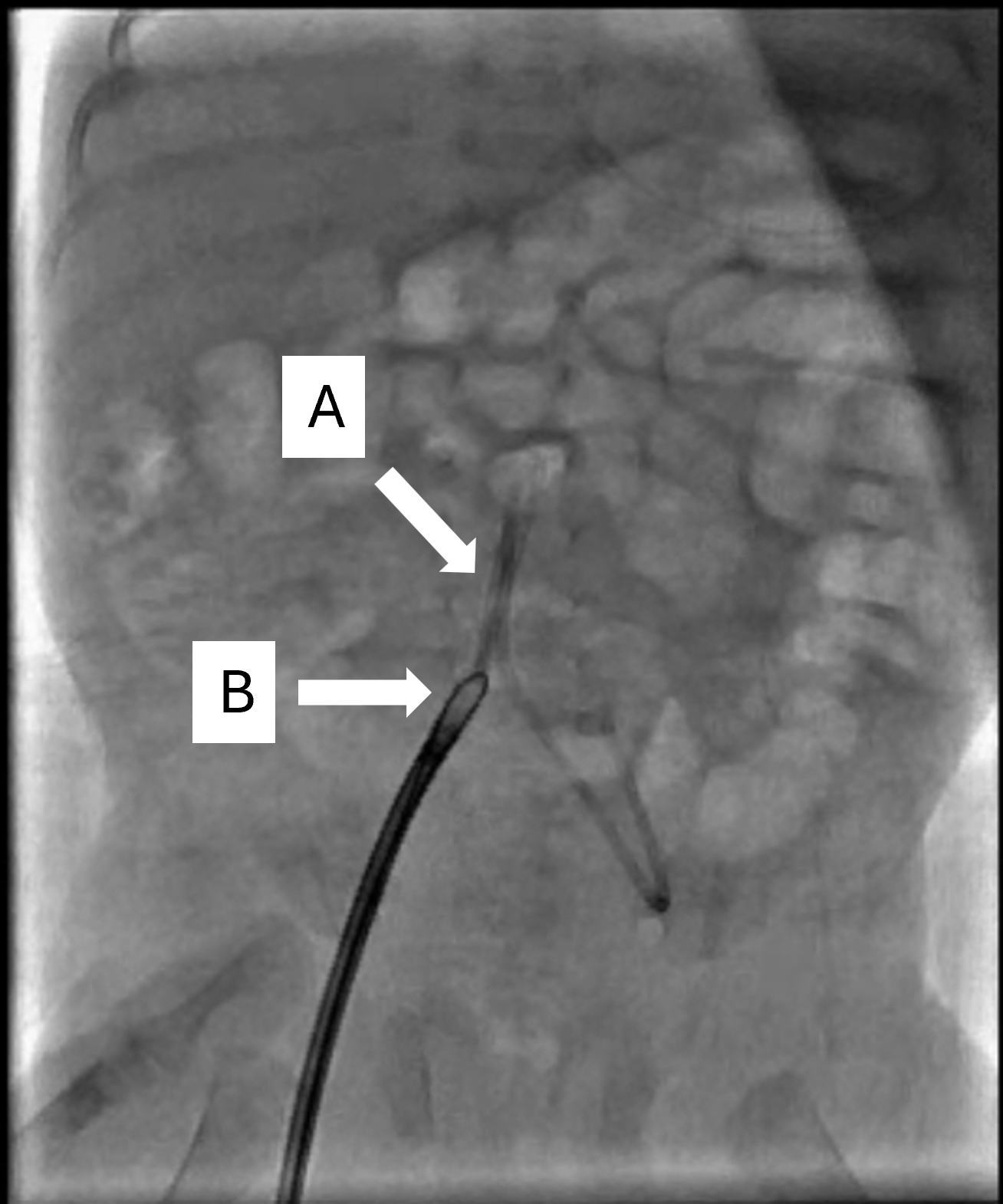
Under general anaesthesia a 20-Gauge intravenous cannula was used to gain right femoral artery access, through which a 0.035-inch hydrophilic guidewire (TerumoTM), followed by a 6F Radifocus radial sheath (TerumoTM) was introduced. Thirty units of unfractionated heparin (UFH) were administered to prevent catheter-related thrombosis. An improvised snare was prepared by double folding a 300 cm 0.014-inch Balanced-Middle-Weight (AbbottTM) coronary guidewire which was inserted in a Judkins Right (JR) 6F coronary guide catheter creating a loop protruding through its distal end (Fig. 1A). The broken catheter was caught within the loop at the level of the descending thoracic aorta and was snared out through the femoral sheaths (Fig. 2, Fig. 3; also see Video 1 in the Supplementary Materials). During the procedure, there was a blood loss of 10-15 mL (15% of the total blood volume of the neonate), which was replaced by packed red blood cell transfusion. Weak pulses with signs of hypoperfusion were noticed in the right lower limb post procedure which was managed with warm packs and a pre-emptive continuous infusion of UFH (28 U/kg/hour); the latter was discontinued once a duplex colour Doppler scan ruled out thrombosis or dissection. Hence, the hypoperfusion was finally attributed to the spasm of the common femoral artery, which later recovered spontaneously. Invasive mechanical ventilation was continued for 2 more days and switched to non-invasive ventilator support, subsequently which the patient was weaned off 23 days later. Subsequently, the neonate developed late-onset neonatal sepsis due to Klebsiella pneumoniae, which was successfully treated with antibiotics. The neonate was discharged finally on the 51st day of life. Further outpatient examination revealed functionally normal right lower limb with well palpable distal pulses. The neonate is doing well with a follow-up of 5 months.
Discussion
Umbilical venous and arterial catheterisations are commonly employed in NICUs to establish prolonged venous access and provide direct arterial access for blood sampling and monitoring, particularly in infants with very low birth weight. Although inserting a UAC is conceptually straightforward, at times it can present significant challenges in clinical settings. Optimal positioning involves the catheter advancing through the umbilicus, descending via the umbilical artery, continuing through the anterior branch of the internal iliac artery, into the common iliac artery, and finally entering the aorta.3 The proximal catheter tip is placed usually in one of the two positions: between the sixth and ninth thoracic vertebrae or at the level of the third or fourth lumbar vertebrae.4 A meta analysis concluded that a higher position of the tip should be preferred to a lower one to avoid vascular complications.5 Numerous dreaded complications like aortic dissection, aortic pseudoaneurysm, aortic thrombosis, renal artery thrombosis, umbilical artery perforation, fracture/breakage have been reported in the literature.6-11 Levit et al.12 reported an overall complication rate of 2.5% among 2035 UAC usage in the NICU over an 11 year period. The most common complication was catheter breakage or fracture, accounting for approximately 40% of all reported complications. The potential reasons for this complication could be inadvertent damage to the catheter during insertion, fixation and removal, particularly from needles or scissors.10 Contributing factors may include catheter material used (Polyurethane has more mechanical strength compared to silicone.), manufacturing defects or prolonged use, which can lead to structural weakening of the catheter.11
After an extensive literature search, we could find only 14 cases of umbilical artery retrieval prior to ours. The majority were retrieved by a surgical approach and only 4, including ours, were successful in a percutaneous approach.13-15 The major problems in adopting a percutaneous approach are difficult vascular access in fragile neonates, local complications post procedure, and limited availability of necessary hardware and technical expertise.16-18
If the stump is visible or palpable at the local site, then local surgical exploration and retrieval should be attempted as done by Doodnath et al.16 and Maggioni et al.17 in their respective cases. In our case, the possibility of local exploration to pull out the UAC from the umbilical area was ruled out since roentgenogram had already shown that its proximal end had embolised into the common iliac artery.
Most of the authors relied upon surgical retrieval with or without local imaging assistance. Lackey et al. were the first to report retrieval of a UAC from the thoracic aorta using a surgical approach.19 In a similar case, Murphy et al. employed a transumbilical surgical approach for catheter retrieval.20 In another case, Dennis et al. reported a 7-day-old neonate with a fractured UAC, where imaging revealed the catheter extended into the umbilical cord stump.11 In this case, despite undergoing exploratory laparotomy and ileal resection, the broken catheter could not be removed surgically, and it was later found to have embolized into the aorta. The operators eventually used intra-operative ultrasound guidance to locate the catheter, which was successfully removed through an aortotomy following aortic cross-clamping. Aortotomy would require cross clamping, hampering perfusion to distal organs with possible grave consequences of ischemia to the spinal cord, limbs and other organs. In another noteworthy case, Uwaifo et al.15 used transcarotid access for retrieval of a UAC from the descending thoracic aorta after failed infraumbilical surgical exploration and transductal approach through a femoral venous access. In this case, the ductus arteriosus was closed and there was lower limb ischemia to begin with, which might have forced them to prefer transcarotid access; however, carotid access may pose a risk of ischemic injury to the brain as well as difficulty achieving hemostasis since there is no bony support behind the vessel against which compression can be easily achieved. In our case there were no signs of lower limb hypoperfusion, therefore we could safely introduce a 6F radial-access sheath which was wide enough to accommodate the UAC even if it was folded or bent on itself at the point where it was captured by the improvised snare.
As neonates, particularly those with low birth weight, are more susceptible to catheter-associated risks, continuous monitoring and early detection are crucial in preventing catastrophic outcomes. Measuring the length of the catheter after routine retrieval, early removal after usage, avoiding tight sutures around the catheter, monitoring the proximal tip position periodically with an ultrasound or X-ray can be done to prevent this catastrophic complication.4 Retrieving foreign bodies using commercially available snares, due to their large diameters, may cause damage to the small vessels in neonates, especially those who are very low birth weight.
Conclusion
The successful percutaneous retrieval of the fractured UAC from the aorta using a make-shift snare improvised from coronary angioplasty hardware in this very low birth weight neonate demonstrates the feasibility and effectiveness of minimally invasive techniques in managing rare and complex complications in neonatal care. Despite the challenges posed by the unexpected catheter fracture and subsequent migration, prompt diagnosis and intervention led to a favourable outcome. A team effort from cardiology, neonatology and anaesthesia helped in achieving this goal.
Supplementary materials
Ethical approval
As per our institutional protocol, ethical committee approval is not required for case reports. Informed consent was obtained from the legal guardians of our patient presented in our case report.
Source of funding
The authors declare the study received no funding.
Conflict of interest
The authors declare that there is no conflict of interest.
References
- Green C, Yohannan MD. Umbilical arterial and venous catheters: placement, use, and complications. Neonatal Netw 1998; 17: 23-28.
- Dilli D, Özyazici E, Fettah N, et al. Rupture and displacement of umbilical arterial catheter: bilateral arterial occlusion in a very low birth weight preterm. Arch Argent Pediatr 2015; 113: e283-e285. https://doi.org/10.5546/aap.2015.eng.e283
- Dumpa V, Avulakunta ID. Umbilical artery catheterization. Treasure Island (FL): StatPearls Publishing; 2025.
- Ramasethu J. Complications of vascular catheters in the neonatal intensive care unit. Clin Perinatol 2008; 35: 199-222. https://doi.org/10.1016/j.clp.2007.11.007
- Barrington KJ. Umbilical artery catheters in the newborn: effects of position of the catheter tip. Cochrane Database Syst Rev 2000; 1999: CD000505. https://doi.org/10.1002/14651858.CD000505
- Wang J, Semple T, Bautista-Rodriguez C, et al. Umbilical artery catheter, aortic dissection, carotid cannulation, and pseudoaneurysm in a neonate: a tale of propagating pathology. Ann Pediatr Cardiol 2020; 13: 87-90. https://doi.org/10.4103/apc.APC_67_19
- Molanus D, van Scherpenzeel M, Derikx J, van den Dungen F. Umbilical artery perforation: a potentially life-threatening complication of umbilical artery catheterisation. BMJ Case Rep 2017; 2017: bcr2017222664. https://doi.org/10.1136/bcr-2017-222664
- Kotnis R, Salloum A, Hitchcock R. Retained umbilical artery catheter presenting as an umbilical abscess. Arch Dis Child Fetal Neonatal Ed 2000; 83: F74. https://doi.org/10.1136/fn.83.1.f74e
- Greenberg R, Waldman D, Brooks C, et al. Endovascular treatment of renal artery thrombosis caused by umbilical artery catheterization. J Vasc Surg 1998; 28: 949-953. https://doi.org/10.1016/s0741-5214(98)70074-6
- Choi SJ, Raziuddin D, Haller JO. Broken umbellical artery catheter: a report of two cases. Am J Dis Child 1977; 131: 595. https://doi.org/10.1001/archpedi.1977.02120180109022
- Dennis PB, Dave N, Shah H, Dias R. A novel use of ultrasound for the extraction of a fractured umbilical arterial catheter. Indian J Anaesth 2019; 63: 660-662. https://doi.org/10.4103/ija.IJA_202_19
- Levit OL, Shabanova V, Bizzarro MJ. Umbilical catheter-associated complications in a level IV neonatal intensive care unit. J Perinatol 2020; 40: 573-580. https://doi.org/10.1038/s41372-019-0579-3
- Simon-Fayard EE, Kroncke RS, Solarte D, Peverini R. Nonsurgical retrieval of embolized umbilical catheters in premature infants. J Perinatol 1997; 17: 143-147.
- Smith PL. Umbilical catheter retrieval in the premature infant. J Pediatr 1978; 93: 499-502. https://doi.org/10.1016/s0022-3476(78)81178-0
- Uwaifo OO, Crittendon I, Lucas VS. Percutaneous retrieval of embolized umbilical arterial catheter in extreme premature infant. J Vasc Access 2025; 26: 671-675. https://doi.org/10.1177/11297298241228613
- Doodnath R, Landreth-Smith B, Rampersad B. Retrieval of a broken umbilical artery catheter in a neonate. J Neonatol 2022; 36: 371-374. https://doi.org/10.1177/09732179221100664
- Maggioni A, Sattar S, Thakkar H, Milan A. Infraumbilical surgical retrieval of transected umbilical artery catheter in an 840 g newborn. BMJ Case Rep 2022; 15: e247296. https://doi.org/10.1136/bcr-2021-247296
- Birkhold M, Khalifeh A, Strauch E. Bilateral lower extremity ischemia due to a retained umbilical artery catheter in a preterm neonate. J Pediatr Surg Case Rep 2020; 56: 101424. https://doi.org/10.1016/j.epsc.2020.101424
- Lackey DA, Taber P. An unusual complication of umbilical artery catheterization. Pediatrics 1972; 49: 281-283. https://doi.org/10.1542/peds.49.2.281
- Murphy KD, Le VA, Encarnacion CE, Palmaz JC. Transumbilical intravascular retrieval of an umbilical artery catheter. Pediatr Radiol 1995; 25(Suppl 1): S178-S179.
Copyright and license
Copyright © 2025 The Author(s). This is an open access article distributed under the Creative Commons Attribution License (CC BY), which permits unrestricted use, distribution, and reproduction in any medium or format, provided the original work is properly cited.